Some symptoms of the disease: the appearance of dark spots before the eyes, blurred vision, narrowing of the field of vision, difficulty distinguishing colors, blindness in half of vision.
The disease can develop at any age and in any person.
Causes of optic nerve atrophy: infectious diseases; traumatic brain and eye injuries; diseases of the nervous system; circulatory disorders; poisoning;
Optic nerve atrophy can also be unilateral (develops in only one eye) or bilateral (develops in both eyes at once), stationary and progressive, partial and complete.
It is impossible to completely cure optic nerve atrophy. However, it is possible to slow down and even stop the pathological process.
It is important to quickly begin treatment not only of atrophy, but also of the disease that caused it.
Chelyabinsk, Pobeda Ave., 287, 9th floor.
+7
Honey. license No. LO-74-01-003927 dated 01/19/2017
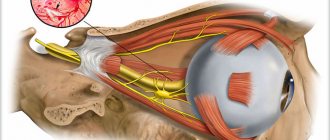
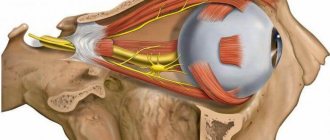
Optic nerve subatrophy is damage to nerve fibers with further destruction and death. The optic nerve consists of axons of nerve fibers that form the retina, from which information flows to the visual cortex, and from there the information is processed and presented in the form of an image. Subatrophy provokes the entry of distorted information into the brain.
Damage to the optic nerve is quite rare, but in most patients, irreversible processes of atrophy of nerve fibers lead to blindness. Treatment of the pathological process is aimed at eliminating the main cause that led to these changes.
Etiological factors in the development of optic nerve subatrophy
Damage and death of nerve fibers can provoke various diseases of the optic nerve and retina of the eye: inflammatory processes, swelling, dystrophic changes, poor circulation, exposure to toxic substances, injuries to the eyeball.
More often, pathology develops with damage to the central nervous system, as well as with a hereditary predisposition. Various pathological conditions can also lead to the disease:
- congenital atrophy occurs as a result of abnormalities in the formation of the organ of vision during intrauterine development of the fetus under the influence of unfavorable factors (various diseases and the use of medications during pregnancy);
- infections and inflammatory processes of the eyes;
- intoxication of the body with drugs and alcoholic beverages;
- ARVI, FLU;
- diseases of the central nervous system (meningitis, purulent process of the brain, syphilis of the brain and others);
- atherosclerotic deposits of blood vessels of the neck and brain;
- persistent increase in blood pressure;
- increased IOP;
- profuse bleeding (blood loss of 30% of the total volume).
Primary atrophy is caused by:
- hypertonic disease;
- atherosclerotic changes in blood vessels;
- diseases of the spine (curvature, displacement of the vertebrae, disruption of the integrity of the fibrous capsule, accompanied by compression of the spinal cord).
Secondary subatrophy develops as a result of:
- acute intoxication processes, in particular after drinking high doses of alcohol;
- retinitis (inflammation of the retina);
- cancer processes;
- injury.
Provoking factors
Only a doctor can determine the exact cause of optic nerve atrophy. There may be several factors simultaneously that provoke necrotic processes. Most often, the disease occurs due to disorders in the spinal cord or brain. Changes in the nervous system or serious trauma to the skull may also have a negative impact. Various types of intoxication, as well as vascular diseases, occur in patients in 25% of cases.
Necrotic processes can be caused by high blood pressure or chronic pathologies that affect the condition of blood vessels.
There are other factors that influence the deterioration of a person’s condition, these include:
- Poisoning with alcohol, tobacco, chemical components or methanol.
- Disorders in the central nervous system. Abscess, meningitis, tumor or sclerosis are another cause of the disorder.
- Fasting, lack of beneficial microelements in the body or regular diets.
- Hereditary predisposition.
- Diseases that affect the condition of the eye apparatus. This includes glaucoma, neuritis and retinal dystrophy.
- Infectious diseases such as herpes, syphilis, influenza or meningitis.
Classification of the disease
There are several classifications of the pathological process. Depending on the cause:
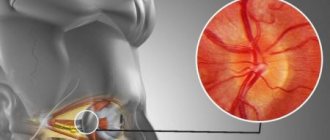
- Primary – atrophy of nerve fibers occurs when the peripheral neurons of the visual pathway are compressed. The optic disc remains unchanged with clearly defined boundaries.
- Secondary – swelling of the optic disc develops, its boundaries are blurred as a result of pathological changes in the retina.
- Glaucomatous subatrophy - the cause is high IOP, resulting in collapse of the lamina cribrosa of the sclera.
According to the degree of progression of the pathology, they are distinguished:
- initial (slight blanching of the optic disc, preservation of the color of the nerve);
- partial (blanching of one area of the optic disc);
- complete subatrophy (thinning and complete blanching of the optic disc, vasoconstriction).
Depending on the location of the lesion:
- ascending atrophy: the retina is damaged;
- descending: destruction of nerve fibers.
The disease can be unilateral or bilateral.
Diagnosis of pathological changes in the optic nerve
To make an accurate diagnosis, an anamnesis of the disease is initially collected; it is very important to determine the presence of diseases present in the body, the use of medications, and the influence of toxic substances.
Further diagnostics consists of:
- testing visual acuity;
- computer perimetry (visual field examination);
- diagnostics of color perception using polychromatic tables;
- fundus ophthalmoscopy;
- ocular tonometry (determination of IOP);
- radiography of the orbit;
- fluorescein angiography;
- Doppler ultrasound;
- MRI and CT of the brain.
Diagnostic measures
The first step to treatment is a full examination with consultation of a neurologist, neurosurgeon, therapist, endocrinologist, rheumatologist, cardiologist. To make a diagnosis, an examination of the fundus of the eye is performed, determining the degree of acuity and visual fields. Subsequently, the atrophied area is studied using computer perimetry, the localization of affected cells is revealed by assessing color perception, and the nature of the damage is assessed using a video ophthalmograph.
An X-ray of the skull in the area of the sella turcica is also performed. If necessary, they additionally resort to magnetic resonance and computed tomography, laser Dopplerography.
How is the treatment carried out?
Subatrophy of the optic nerve is a severe pathology that cannot be treated; after the death of the nerve fibers, their restoration is impossible. Treatment is aimed at eliminating the underlying disease that caused damage and death of the optic nerve. In case of tumor processes and cerebral aneurysms, surgical intervention is necessary.
Conservative therapy is carried out to preserve vision, reduce swelling and inflammatory processes (dexamethasone injections are administered through the skin of the lower eyelid under the eyeball, glucose and calcium chloride are given intravenously, and furosemide is administered intramuscularly).
In the complex of therapy, drugs are prescribed to improve blood circulation, a complex of B vitamins. To reduce intraocular pressure, instillations of pilocarpine hydrochloride are performed on the conjunctiva, and diuretics are used.
In some cases, physiotherapeutic procedures are used: acupuncture, electrophoresis, laser radiation, ultrasound, magnetic therapy.
To prevent damage to the optic nerve, it is recommended to carry out timely treatment of infectious and inflammatory diseases of internal organs, as well as promptly seek qualified medical help if characteristic visual symptoms develop.
Optic nerve atrophy (optic neuropathy) is partial or complete destruction of the nerve fibers that transmit visual stimuli from the retina to the brain. Optic nerve atrophy leads to decreased or complete loss of vision, narrowing of visual fields, impaired color vision, and pallor of the optic disc. The diagnosis of optic nerve atrophy is made by identifying characteristic signs of the disease using ophthalmoscopy, perimetry, color testing, determination of visual acuity, craniography, CT and MRI of the brain, B-scanning ultrasound of the eye, angiography of retinal vessels, studies of visual VP, etc. With optic atrophy nerve treatment is aimed at eliminating the pathology that led to this complication.
Types and characteristics of diseases
Diseases of this organ are divided into congenital anomalies and acquired ailments. Thus, some people from birth suffer from a pathology in the development of the system, there is a fossa in the disc or megalopopilla. At a conscious age, atrophy of the optic nerve or neuritis may develop due to injuries. All these deviations lead to complete or partial loss of vision, as well as deterioration in color perception.
The following violations are distinguished:
- increase in the diameter of the DNZ (megalopopilla);
- aplasia;
- hypoplasia;
- neuritis;
- atrophy;
- drusen DNZ;
- dilatation or constriction of blood vessels.
All pathologies of this part of the visual apparatus are divided into two large categories:
- congenital,
- acquired.
According to the etiology, clinical picture and nature of the course of the disease, there may be:
- allergic,
- inflammatory,
- dystrophic.
Tumors and developmental abnormalities are also identified. It is worth considering in more detail the most common groups of pathologies.
Neuritis
By neuritis we mean an inflammatory process on any part of the optic nerve. The causative agents can be microbes or viruses, which, as a rule, have spread to the optic nerve from another inflamed organ - the eyeball, cerebral cortex, paranasal sinuses, etc. Sometimes such a complication is caused by influenza suffered in severe form.
Pathologies associated with lesions of the nervous system, which may be accompanied by neuritis:
- encephalitis;
- meningitis;
- brain abscess;
- inflammation of the membranes of blood vessels;
- pathologies of the nervous system of a demyelinating nature.
Diseases not associated with pathologies of the nervous system and brain, which can also provoke neuritis:
- sinusitis;
- otitis;
- caries;
- viral infections;
- bacterial infections of any internal organs.
There are two types of neuritis:
- Papillary - inflammation is localized in the area of the optic disc.
- Retrobulbar - the focus of inflammation is localized in the area between the disc and the chiasm of the optic tract.
Main signs of neuritis:
- deterioration of vision to its complete loss;
- narrowing of visual fields or their partial loss;
- impaired color vision;
- spots, dots, fog before the eyes;
- headache;
- pain behind the eye of an intermittent nature, intensifying with eye movement.
Diagnosis is carried out by examining the fundus of the eye based on changes in the structure of nerve fibers characteristic of the inflammatory process. An encephalogram and MRI may also be performed.
Treatment involves antibiotic therapy if the neuritis is caused by a bacterial infection. To stop the inflammatory process, glucocorticoids are prescribed; for concomitant glaucoma and increased intraocular and intracranial pressure, diuretics are used. To strengthen nerve tissue and prevent dystrophy, a course of nootropic therapy is indicated.
For information: if there are symptoms of optic neuritis, the patient should first be taken to an ophthalmologist for examination, and then admitted to a hospital for further treatment. You cannot treat neuritis on your own at home.
Atrophy
Atrophy refers to the slow death of nerve fiber cells that occurs as a result of congestive or inflammatory processes in the optic nerve. Atrophy can be congenital or acquired. Causes of acquired pathology:
- diseases of the nervous system, including optic neuritis;
- brain abscess;
- tumors, resulting in compression of the nerve;
- disturbance of blood supply;
- encephalitis;
- traumatic brain injuries;
- intoxication, including alcohol poisoning.
Atrophy can develop with retinal diseases, uevitis, vitamin deficiencies, and starvation. The main symptom of the pathology is blurred vision, narrowing or loss of some fields. The following signs of optic nerve destruction are also observed:
- impaired color vision;
- loss of twilight vision;
- dilation of the pupil with reduced or completely absent reaction to light;
- inability to follow an object with your eyes or focus your gaze.
To accurately diagnose the disease, the first step is to examine the fundus. With this pathology, the disc will have blurred boundaries; instead of pink, it will become pale. A CT scan or MRI may be performed to determine the extent of damage to blood vessels and nerve fibers. Computer perimetry is required to identify affected areas of the visual pathway.
Treatment is primarily aimed at eliminating the root cause - the underlying disease that provoked the disorder. Next, you need to stop the atrophic process. In case of partial atrophy, treatment is aimed at restoring those fibers that have not yet been completely destroyed. The following methods are used:
- Drug therapy - drugs to dilate blood vessels and normalize blood circulation, vitamins to nourish nerve fiber cells, ATP drugs.
- Physiotherapy – electromagnetic stimulation of the optic nerve, light, laser stimulation.
- Surgical treatment – revascularization of nerves, implantation of electrodes to the disc, vasoreconstruction.
This diagnosis implies a circulatory disorder, as a result of which optic nerve ischemia develops. As a rule, the disease develops in men over 60 years of age who also suffer from atherosclerosis, hypertension, and arteritis. Main symptoms of the pathology:
- sudden deterioration of vision in one eye;
- scotomas;
- with ophthalmoscopy - swelling of the disc.
Treatment is aimed primarily at removing excess fluid from the body; diuretics are used for this. Corticosteroids and vasodilators are also used. With such a diagnosis, it is important to start treatment on time and carry it out to the end, otherwise atrophy will develop.
Coloboma is a congenital pathology of a non-progressive nature. It appears as a depression of varying diameters in different areas in the area of the optic disc. The cavity is filled with retinal cells. Excavation can be localized on the iris, retina, or optic nerve due to incomplete or improper closure of the embryonic fissure. Normally, it should close in the 4th – 5th week of pregnancy.
The reasons may be a genetic predisposition or a cytomegalovirus infection suffered during gestation. Lesions can be unilateral or bilateral; in newborns they are detected during ophthalmoscopy as a round depression of a silvery hue, larger in size than the optic disc itself. In this case, coloboma is accompanied by:
- myopia;
- myopic astigmatism;
- squint.
In children, the pathology often occurs against the background of focal skin hypoplasia, epidermal nevus syndrome, Down, Warburg and Edwards syndromes. If left untreated, macular edema first develops, then a macular hole occurs, resulting in detachment of the inner and outer layers of the retina.
Treatment of pathology during the formation of a subretinal neovascular membrane is carried out through laser coagulation. If macular detachment occurs, surgical treatment is indicated. Mainly two methods are used:
- vitrectomy, after which a special gas is injected into the cavity of the affected eye;
- laser coagulation of the retina with krypton.
MORE ABOUT: Sciatic nerve pain: what to do?
Causes, symptoms and treatment for sciatica The congenital form of the disease rarely develops in isolation; as a rule, it is accompanied by a number of other ophthalmological pathologies and disorders of the nervous system, and therefore requires complex and consistent treatment.
Hypoplasia is a reduction in the diameter of the optic disc by 30–50%; it can be unilateral or bilateral. Visual acuity in this case varies from 1.0 to complete absence of light perception; it can be manifested by the loss of certain sections of the fields, impaired peripheral or central vision. The pathology is also non-progressive. Its most severe form is aplasia, that is, the complete absence of optic nerve fibers.
This pathology, like many other congenital ones, rarely occurs in isolation; as a rule, it is accompanied by other defects of the eyes, brain, and central nervous system. Reasons for development:
- lack of prevention of abnormalities in fetal development in the first trimester of pregnancy (taking vitamins, folic acid);
- maternal drug addiction and alcoholism;
- chronic diseases associated with metabolic disorders - for example, diabetes;
- taking medications - anticonvulsants, steroids, diuretics;
- quinine poisoning during pregnancy.
Symptoms of MN hypoplasia:
- decrease in visual acuity to 1.0 or lower;
- lack of twilight vision and color perception;
- loss of some visual fields;
- afferent pupillary disorder;
- aniridia;
- strabismus.
On ophthalmoscopy, the disc is reduced in size, gray in color, surrounded by chorioretinal atrophy, and the vessels have a tortuous shape. To make an accurate diagnosis, MRI and computed tomography are also performed; in some cases, additional studies will be required. It is important to carry out a differential diagnosis with MN aplasia. To do this, the vessels of the nerve are examined. In case of aplasia, they are not visible, but in case of hypoplasia, vessels of normal shape with a corkscrew-like course are determined.
Treatment makes sense only in early childhood. The following methods are used:
- eliminating the influence of ocular deprivation on the visual system that has not yet been fully formed. It is important to prevent the development of amblyopia, and if it has already been identified, then promptly carry out adequate treatment;
- early correction of contact ametropia;
- dosed occlusion of a healthy eye;
- laser pleoptics.
Thus, treatment is based more on preventing complications and preserving vision in the healthy eye.
General information
Various diseases of the optic nerve in ophthalmology occur in 1-1.5% of cases; of these, 19 to 26% lead to complete atrophy of the optic nerve and incurable blindness. Pathomorphological changes in optic nerve atrophy are characterized by destruction of axons of retinal ganglion cells with their glial-connective tissue transformation, obliteration of the capillary network of the optic nerve and its thinning. Optic nerve atrophy can be a consequence of a large number of diseases that occur with inflammation, compression, swelling, damage to nerve fibers or damage to the blood vessels of the eye.
Traditional medicine recipes
1. Place 5 tbsp in a saucepan. l. pine or Christmas tree, 2 tbsp. l. chopped rose hips, pour 700 ml of water and boil for 10 minutes over low heat. This should be done in the evening, after which the pan should be wrapped in something warm and left to steep overnight until the morning.
In the morning, strain and drink the entire portion little by little throughout the day. Drink every day (at least 3-4 months). You can add honey.
In addition, apply eyebright tea compresses to your eyes 7-8 times a day. Eyebright is sold at the market by herbalists.
2. Apply 2-3 drops of fresh butter to your eyes 3 times a day.
3. Take 100 pieces of small unripe pine cones, lemon and 25 g of rue herb during the flowering period. Cut the lemon into several parts and mix everything. Pour 2.5 liters of water, add ½ cup of sugar and cook for 30 minutes.
Take 1 tbsp. spoon 3 times a day before meals. The course of treatment for optic nerve atrophy is 25-30 days.
4. Take 100 g of wheatgrass and calamus roots, 150 g of rose hips and mix. 3 tbsp. Put the mixture in a thermos in the evening, pour three glasses of boiling water, strain in the morning and take 150 g 4 times a day an hour before meals.
5. This folk remedy for treating optic nerve atrophy also helps: pour 50 g of lily of the valley flowers into 0.5 liters of vodka and leave it in a warm place to brew for 10 days.
Strain and take 7 drops 3 times a day.
6. Place 100 g of maple leaves in an enamel pan, pour in 1 liter of white grape wine and let it boil for 5 minutes under a closed lid. Remove from heat, let it brew for half an hour, strain and apply as a compress to your eyes.
These are the folk remedies for treating optic nerve atrophy at home.
Causes of optic nerve atrophy
Factors leading to optic nerve atrophy may include eye diseases, central nervous system lesions, mechanical damage, intoxication, general, infectious, autoimmune diseases, etc.
The causes of damage and subsequent atrophy of the optic nerve are often various ophthalmopathologies: glaucoma, retinal pigmentary dystrophy, occlusion of the central retinal artery, myopia, uveitis, retinitis, optic neuritis, etc. The danger of damage to the optic nerve may be associated with tumors and diseases of the orbit: meningioma and optic nerve glioma, neuroma, neurofibroma, primary orbital cancer, osteosarcoma, local orbital vasculitis, sarcoidosis, etc.
Among the diseases of the central nervous system, the leading role is played by tumors of the pituitary gland and posterior cranial fossa, compression of the area of the optic chiasm, purulent-inflammatory diseases (brain abscess, encephalitis, meningitis), multiple sclerosis, traumatic brain injury and damage to the facial skeleton accompanied by injury optic nerve.
Classification
Optic nerve atrophy can be hereditary or non-hereditary (acquired). Hereditary forms of optic atrophy include autosomal dominant, autosomal recessive and mitochondrial. The autosomal dominant form can have a severe or mild course, and is sometimes combined with congenital deafness. An autosomal recessive form of optic nerve atrophy occurs in patients with Wehr, Wolfram, Bourneville, Jensen, Rosenberg-Chattorian, and Kenny-Coffey syndromes. The mitochondrial form is observed when there is a mutation in mitochondrial DNA and accompanies Leber's disease.
Acquired atrophy of the optic nerve, depending on the etiological factors, can be primary, secondary and glaucomatous in nature. The mechanism of development of primary atrophy is associated with compression of peripheral neurons of the visual pathway; The optic disc is not changed, its boundaries remain clear. In the pathogenesis of secondary atrophy, swelling of the optic disc occurs, caused by a pathological process in the retina or the optic nerve itself. The replacement of nerve fibers by neuroglia is more pronounced; The optic disc increases in diameter and loses its clear boundaries. The development of glaucomatous optic atrophy is caused by the collapse of the lamina cribrosa of the sclera against the background of increased intraocular pressure.
Based on the degree of color change of the optic nerve head, initial, partial (incomplete) and complete atrophy are distinguished. The initial degree of atrophy is characterized by slight blanching of the optic disc while maintaining the normal color of the optic nerve. With partial atrophy, disc blanching in one of the segments is noted. Complete atrophy is manifested by uniform pallor and thinning of the entire optic nerve head, and narrowing of the fundus vessels.
Based on localization, ascending (if retinal cells are damaged) and descending (if optic nerve fibers are damaged) atrophy is distinguished; by localization - unilateral and bilateral; according to the degree of progression - stationary and progressive (determined during dynamic observation by an ophthalmologist).
↑ Material and methods
We examined 132 patients (188 eyes) aged from 16 to 87 years (median 48 years) with an established diagnosis of ON of various non-glaucomatous origins, including 23% of eyes with non-arteritic anterior ischemic ON, 10% with posterior ischemic ON, 22% with ON inflammatory origin (with demyelinating diseases, autoimmune, infectious, sarcoid etiology), 10% with compression ON in tumors of the optic nerve, orbit, chiasmatic-sellar region and base of the anterior cranial fossa, 12% with ON in drusen of the optic nerve head, 8% with traumatic ON, 7% with endocrine neuroophthalmopathy, 6% with hereditary Leber ON, 2% with toxic ON. In 43% of cases (58 patients), ON was bilateral. All patients did not have any other ophthalmopathology affecting the functions and structures of the optic nerve.
To determine the specificity of morphofunctional methods for studying the optic nerve, 52 patients (75 eyes) without optic nerve pathology were examined.
All patients underwent traditional ophthalmological functional studies: determination of maximum visual acuity, assessment of color vision according to Rabkin tables, study of pupillary reactions with determination of the relative afferent pupillary defect (RAPD), kinetic perimetry with object III4e; biomicro- and ophthalmoscopy.
In-depth functional studies were also performed: computer perimetry using a static neurological N1 program (perimeter Octopus 900, Interzeag AG, Switzerland), general and multifocal electro-retinography (MF-ERG), study of VEP for flash and pattern (Tomeu) , EP-1000 Multifocal, Germany).
A study of the structure of the optic nerve head with determination of the average thickness of the retinal nerve fiber layer (RNFL) in the peripapillary zone (diameter 3.4 mm) and separately in 4 quadrants (upper, lower, nasal, temporal) was performed using OCT on an OCT Stratus 3000 retinotomograph ( "Carl Zeiss")
Criteria for determining indicators of research methods with deviations from the norm
Static perimetry.
The results were considered abnormal if the perimetry indices MD (mean defect) - more than 2 decibels and/or sLV (loss variance) - more than 2.5 decibels. All static perimetry results included in this study were reliable, since the RF (reliability factor) index, calculated from false-positive and false-negative responses from patients, was in all cases less than 15%.
OCT.
Results were considered abnormal if the average RNFL thickness or the RNFL thickness in one of the quadrants was significantly decreased or increased compared to normal, p < 0.05.
ZVP.
The results were considered abnormal if the latency of the P100 peak exceeded the upper limits of normal, as well as in the presence of significant (more than 5 ms) interocular asymmetry of this parameter. The analysis also took into account the violation of the P100 peak configuration.
Some patients underwent fluorescein angiography and magnetic resonance imaging of the brain according to indications.
Symptoms of optic atrophy
The main sign of optic nerve atrophy is a decrease in visual acuity that cannot be corrected with glasses and lenses. With progressive atrophy, a decrease in visual function develops over a period of several days to several months and can result in complete blindness. In the case of incomplete atrophy of the optic nerve, pathological changes reach a certain point and do not develop further, and therefore vision is partially lost.
Objective signs of optic nerve atrophy are revealed during an ophthalmological examination.
Symptoms
The main sign of the onset of pathology can be a steadily progressive deterioration of vision in one or both eyes, and it cannot be corrected by conventional methods.
Visual functions are gradually lost:
- Disappearance of lateral vision (narrowing of visual fields);
- The appearance of “tunnel” vision;
- Formation of scotomas (dark spots) in various parts of the visual field;
- Decreased pupillary reaction to light while maintaining the friendly reaction.
The onset of symptoms may last several days or months, depending on the severity of the lesions, but without a timely response it invariably leads to complete blindness.
Diagnostics
When examining patients with optic nerve atrophy, it is necessary to find out the presence of concomitant diseases, the fact of taking medications and contact with chemicals, the presence of bad habits, as well as complaints indicating possible intracranial lesions.
During a physical examination, the ophthalmologist determines the absence or presence of exophthalmos, examines the mobility of the eyeballs, checks the reaction of the pupils to light, and the corneal reflex. Visual acuity testing, perimetry, and color vision testing are required.
Basic information about the presence and degree of optic nerve atrophy is obtained using ophthalmoscopy. Depending on the cause and form of optic neuropathy, the ophthalmoscopic picture will differ, but there are typical characteristics found in various types of optic atrophy. These include: pallor of the optic disc of varying degrees and prevalence, changes in its contours and color (from grayish to waxy), excavation of the disc surface, a decrease in the number of small vessels on the disc (Kestenbaum’s symptom), narrowing of the caliber of the retinal arteries, changes in the veins, etc. Condition The optic disc is clarified using tomography (optical coherence, laser scanning).
Treatment of optic atrophy
Since optic nerve atrophy in most cases is not an independent disease, but is a consequence of other pathological processes, its treatment must begin with eliminating the cause. Neurosurgical surgery is indicated for patients with intracranial tumors, intracranial hypertension, cerebral aneurysms, etc.
Nonspecific conservative treatment of optic nerve atrophy is aimed at preserving visual function as much as possible. In order to reduce inflammatory infiltration and swelling of the optic nerve, para- and retrobulbar injections of dexamethasone solution, intravenous infusions of glucose and calcium chloride solutions, and intramuscular administration of diuretics (furosemide) are performed.
To improve blood circulation and trophism of the optic nerve, injections of pentoxifylline, xanthinol nicotinate, atropine (parabulbar and retrobulbar) are indicated; intravenous administration of nicotinic acid, aminophylline; vitamin therapy (B2, B6, B12), injections of aloe or vitreous extract; taking cinnarizine, piracetam, riboxin, ATP, etc. In order to maintain a low level of intraocular pressure, pilocarpine is instilled and diuretics are prescribed.
In the absence of contraindications for optic nerve atrophy, acupuncture and physiotherapy (electrophoresis, ultrasound, laser or electrical stimulation of the optic nerve, magnetic therapy, endonasal electrophoresis, etc.) are prescribed. If visual acuity decreases below 0.01, any treatment provided is not effective.
Diagnosis and treatment
The optic nerve is treated in such branches of medicine as ophthalmology or neurology. Atrophy is only a symptom of other inflammatory diseases. Therefore, people who have intrathecal hemorrhage, aneurysm, hypertension and tumors need to consult a neurosurgeon. To improve blood circulation, Atropine, Pentoxifylline, and Xanthinol Nicotinate are prescribed.
For neuritis, the ophthalmologist prescribes treatment with antibiotics and anti-inflammatory drugs. Be sure to detoxify. To maintain the health and development of the optic nerve, it is recommended to consume vitamins B and C. If you do not seek help from a doctor in time, the axon cells die, which leads to atrophy.
Treatment of optic atrophy is a very difficult task for doctors. You need to know that destroyed nerve fibers cannot be restored. One can hope for some effect from treatment only by restoring the functioning of nerve fibers that are in the process of destruction, which still retain their vital functions. If this moment is missed, then vision in the affected eye can be lost forever.
When treating atrophy, it is necessary to keep in mind that this is often not an independent disease, but a consequence of other pathological processes affecting various parts of the visual pathway. Therefore, treatment of optic nerve atrophy must be combined with elimination of the cause that caused it. If the cause is eliminated in a timely manner and if atrophy has not yet developed, normalization of the fundus picture and restoration of visual functions occurs within 2-3 weeks to 1-2 months.
Treatment is aimed at eliminating edema and inflammation in the optic nerve, improving its blood circulation and trophism (nutrition), restoring the conductivity of not completely destroyed nerve fibers.
But it should be noted that the treatment of optic nerve atrophy is long-term, its effect is weak, and sometimes completely absent, especially in advanced cases. Therefore it should be started as early as possible.
As mentioned above, the main thing is the treatment of the underlying disease, against the background of which complex treatment of optic nerve atrophy is carried out. For this, various forms of drugs are prescribed: eye drops, injections, both general and local; tablets, electrophoresis. Treatment is aimed at
- improvement of blood circulation in the vessels supplying the nerve - vasodilators (complamin, nicotinic acid, no-spa, papaverine, dibazol, aminophylline, trental, halidor, sermion), anticoagulants (heparin, ticlid);
- to improve metabolic processes in nerve tissue and stimulate the restoration of altered tissue - biogenic stimulants (aloe extract, peat, vitreous, etc.), vitamins (ascorutin, B1, B2, B6), enzymes (fibrinolysin, lidase), amino acids (glutamic acid ), immunostimulants (ginseng, eleuthorococcus);
- to resolve pathological processes and stimulate metabolism (phosphaden, preductal, pyrogenal); to relieve the inflammatory process - hormonal drugs (prednisolone, dexamethasone); to improve the functioning of the central nervous system (emoxipin, Cerebrolysin, Fezam, nootropil, Cavinton).
Medicines must be taken as prescribed by a doctor after diagnosis. The doctor will select the optimal treatment, taking into account concomitant diseases. In the absence of concomitant somatic pathology, you can independently take no-shpa, papaverine, vitamin preparations, amino acids, emoxypine, nootropil, fesam.
But you should not self-medicate for this serious pathology. Physiotherapeutic treatment and acupuncture are also used; methods of magnetic, laser and electrical stimulation of the optic nerve have been developed.
MORE ABOUT: Epilepsy and partial optic atrophy
The course of treatment is repeated after several months.
Nutrition for optic nerve atrophy should be complete, varied and rich in vitamins. You need to eat as much fresh vegetables and fruits as possible, meat, liver, dairy products, cereals, etc.
If vision is significantly reduced, the issue of assigning a disability group is decided.
The visually impaired and the blind are prescribed a course of rehabilitation aimed at eliminating or compensating for the limitations in life that have arisen as a result of vision loss.
Treatment with folk remedies is dangerous because precious time is lost when it is still possible to cure atrophy and restore vision. It should be noted that for this disease, folk remedies are ineffective.
As medical practice shows, it is not possible to completely restore the optic nerve in glaucoma, since the destroyed nerve fibers will never return to their previous state.
In order to at least partially cure optic nerve atrophy, therapeutic measures should be started as early as possible. You need to know that this dystrophy can be an independent disease, or it can only be a consequence of other certain processes of a pathological nature. In the case of the latter option, treatment will be aimed at identifying and stopping these pathologies. Complex therapy includes a whole course of drugs in the form of tablets, injections, and eye drops.
Therapeutic restoration of the optic nerve consists of the following stages:
- Taking medications to improve the flow and circulation of blood entering the vessels. The so-called vasodilator medications include No-shpu, Eufillin, Papaverine, Sermion, and nicotinic acid-based tablets. Anticoagulants (Heparin, Tiklid) showed excellent results.
- The use of agents that stimulate the regeneration of atrophied tissues and metabolic processes in them. This type of preparation includes biostimulants (aloe extract, peat, vitreous), vitamin complexes (Ascorutin, group B1, B2, B6), specific enzymes (Lidase), immunostimulants (ginseng, tincture of Eleutherococcus), amino acids in the form of glutamic acid.
- Atrophy of the optic nerve may be preceded by some kind of inflammatory process. It can be stopped with the help of hormonal drugs (Dexamethasone, Prednisolone).
- An obligatory stage of treatment is to improve the functioning of the patient’s central nervous system. This can be achieved with the help of the following drugs: Cerebrolysin, Phezam, Nootropil. These medications should never be prescribed independently. Get recommendations from a specialist.
- Physiotherapeutic procedures. For patients with partial or complete atrophy, stimulation of the optic nerve using a magnetic or laser device is indicated. Electrophoresis and ultrasound will help in treatment.
Statistics show that treatment with folk remedies is ineffective and can cause irreparable harm, as a person wastes time and the disease gradually progresses.
In particularly severe and advanced cases, the patient will be prescribed surgical treatment. It involves eliminating tumors that compress areas of the optic nerve. It is possible to introduce biomaterials that will stimulate blood flow to the atrophied nerve.
If, even after therapy, vision continues to decline, then the person is assigned a disability of the corresponding group.
In addition to the diagnostic examination performed by an ophthalmologist, an examination by a neurologist or neurosurgeon may be required. Unfortunately, there are no methods that could quickly and completely cure even partial atrophy of the optic nerve.
For this purpose, different methods of stimulating the ocular apparatus are used. A magnetic field, electric current or laser can be used. The sooner a disorder is identified and a diagnosis is made, the greater the chances for positive dynamics for the patient.
Magnetic stimulation is most often used. Thanks to a special device, metabolic processes begin to accelerate and the optic nerve heals faster. If the patient did not delay treatment, but immediately turned to an ophthalmologist, then only 15 sessions will be enough.
In addition, a person with atrophy is prescribed a course of vasodilating medications, vitamins, and, if necessary, a blood transfusion is performed. In some cases, surgical treatment is prescribed.
Treatment of optic nerve atrophy with folk remedies can be carried out only at the initial stage of the disorder and after consultation with a specialist. A decoction of lemon, rue or pine cones is considered effective. The mixture is consumed 1 tbsp. before meals no more than 3 times a day.
The disease can be cured within a few weeks or months. If you follow all the specialist’s recommendations, you can avoid negative consequences and maintain the health of your eyes.
Prognosis and prevention
If optic nerve atrophy was diagnosed and treated at an early stage, vision may be preserved and even slightly improved, but visual function will not be fully restored. With progressive optic nerve atrophy and untreated, complete blindness can develop.
To prevent optic nerve atrophy, timely treatment of eye, neurological, rheumatological, endocrine, and infectious diseases is necessary; prevention of intoxication, timely blood transfusion in case of profuse bleeding. At the first signs of visual impairment, consultation with an ophthalmologist is necessary.