Causes and mechanisms of development
Smoking is one of the causes of neuritis
Neuritis of the hypoglossal nerve can develop for many reasons. There is a list of factors that contribute to inflammation of the hypoglossal nerve. These include:
- operations performed in the oral cavity;
- angina;
- tuberculosis;
- chronic alcoholism;
- lack of B vitamins in the body;
- malignant or benign tumors in the oral cavity;
- smoking;
- oral cysts;
- lack of B vitamins;
- hyperchromic B12 deficiency anemia;
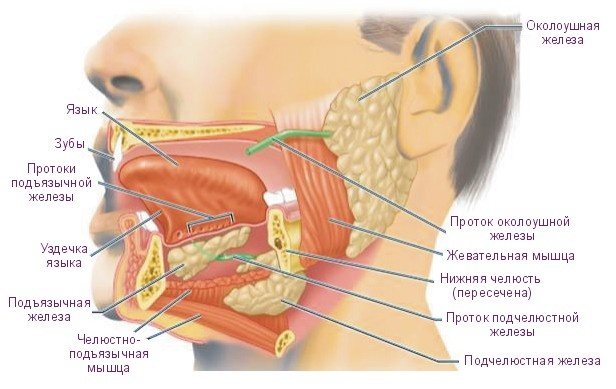
- inflammation of the submandibular salivary glands.
Inflammation may involve the fiber itself, or only the canal of the hypoglossal nerve. It can be one-sided or two-sided.
Symptoms of neuritis
Neuritis of the submandibular nerve is manifested by special symptoms that are specific specifically for inflammation of the hypoglossal nerve. The main symptoms are presented in the table:
| The main symptoms of neuritis of the hypoglossal nerve | |
| Symptom name | Characteristic |
| Impaired motor function of the hypoglossal nerve | When the tongue sticks out of the mouth, it deviates in the direction of the lesion. The patient may also experience speech impairment and dysarthria. Speech impairment occurs during an exacerbation of inflammation in the hypoglossal nerve canal, or in the nerve fiber itself. |
| Tongue pain | As a rule, the patient experiences attacks of pain in the tongue, they are more pronounced on the affected side. |
| Headache | It is a very common symptom of inflammation of the hypoglossal nerve. It usually goes away as soon as the pain in the tongue ends. |
| Type of tongue | The tip of the tongue is extended to the healthy side, and the root of the tongue, during an attack of pain, rises on the affected side. |
The clinical picture has a paroxysmal course. The duration of the attack can vary from several seconds to several hours. Most often, the tongue hurts on the affected side, and headaches are also observed on the same side. It is because of the unilateral pain that this disease is sometimes confused with migraine.
In rare cases, the inflammatory process is bilateral. In this case, pain is observed not on the affected side, but on the entire surface of the tongue.
Nature of the clinical picture
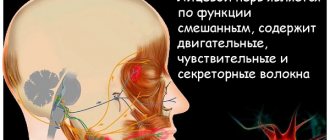
The pathological condition occurs with acute pain symptoms, which are observed in the subradicular lingual region or in the area of one tonsil. The pain syndrome in neuralgia is based not only in the area of the glossopharyngeal nerve, it radiates to the soft palate, pharyngeal region, ear, and sometimes the symptom radiates to the eyes, jaw, and neck.
The syndrome is unilateral. Duration – no more than 2-3 minutes. The symptom intensifies when the tongue moves, for example, while eating or speaking loudly.
The work and rest schedule is disrupted: night insomnia occurs due to severe pain. A person sleeps on one side, on the side with no unpleasant sensations.
Other characteristic symptoms include increased dryness of the oral mucosa, and after the attack ends, on the contrary, increased salivation. The produced liquid has a viscous consistency.
Sometimes glossopharyngeal neuralgia can provoke general symptoms:
- dizziness;
- the appearance of “goosebumps” in the eyes;
- hypotension (low blood pressure);
- rarely - fainting.
The latter symptoms appear due to irritation of a branch in the glossopharyngeal nerve, which depresses the vasomotor center of the brain and causes a drop in pressure.
Neurological pathology is characterized by exacerbation and remission. The remission stage can last quite a long time, sometimes reaching 1 year.
As the pathology develops, periods of exacerbation of symptoms become more frequent, and pain symptoms intensify.
The sensitivity of those areas that participate in the innervation of the glossopharyngeal nerve is impaired: the tongue (posterior third), tonsil, pharynx on one side, soft palate, ear. Taste perception is also lost.
Principles of disease diagnosis and diagnosis
Since neuritis of the hypoglossal nerve has a specific and special clinical picture, a neurologist can assume inflammation of this nerve just by the symptoms. To choose a treatment method, it is also necessary to identify the very cause of nerve inflammation. For this purpose, it is necessary to conduct a number of laboratory and instrumental studies. Their list is presented in the table below:
| Investigations for neuritis of the hypoglossal nerve | ||
| Name of research method | What diseases causing neuritis of the hypoglossal nerve can be identified with its help? | Characteristics and interpretation of the results obtained |
| General blood analysis | It is possible to detect the presence of a bacterial or viral inflammatory process in the body, anemia, and allergies. | With a bacterial infection, an increase in the level of neutrophils and a shift in the leukocyte formula to the left will be observed. With an infection of viral etiology, lymphocytes will be increased in the blood. High eosinophils in the blood will speak in favor of allergies. With anemia, there will be a decrease in the number of red blood cells and hemoglobin. |
| Head computed tomography (CT) | CT scans can visualize bone changes in the bone tissue that could lead to nerve compression, such as trauma to the lower jaw. | In layer-by-layer tomography images you can see changes in the bone structure. |
| Magnetic resonance imaging of the head (MRI) | MRI is used to detect malignant or benign tumors and cysts. | You can visualize tumors and cysts, determine their size, wall thickness and exact location. |
| Oropharyngeal culture | Used when a sore throat or other bacterial disease is suspected. | A swab from the oropharynx is sown on various nutrient media. And therefore, as colonies grow on these media, the presence or absence of certain bacteria in the oropharynx is assessed. |
| X-ray of the chest organs | Used to detect tuberculosis. Since in some cases, neuritis of the hypoglossal nerve is a symptom of tuberculosis. | In case of tuberculosis, without a plain X-ray of the chest organs, you can see foci of dissemination, cavities, and cavities. |
Bulbar and pseudobulbar syndrome
The cause of the first disease is degenerative degeneration of tissue in the cerebral cortex, impaired blood flow to the medulla oblongata, the appearance of stem tumors, polyencephalomyelitis, structural pathologies, and injuries to the base of the skull.
Signs: immobility of the epiglottis, larynx and soft palate, change in voice, loss of intelligible speech, difficulty swallowing (liquid food can flow into the nose), difficulty breathing. The vocal cords are in a “cadaverous position”, the tongue twitches fibrillarly. If the facial and trigeminal nerves are additionally affected, the masticatory muscles atrophy and the lower jaw sag.
Pseudobulbar syndrome is very similar to bulbar syndrome, but it is a lesion of the corticonuclear connections on both sides. A larger number of cranial nerves are affected, including the hypoglossal nerve, and cerebral ischemia occurs. Symptoms include drooling, reflex movements of the eyeballs, bouts of crying or laughing, dementia and decreased intelligence.
Basic principles of treatment
Neuritis of the hypoglossal nerve is treated, as a rule, by a neurologist. After identifying the cause of nerve inflammation, etiological and symptomatic treatment is prescribed.
Principles of etiological treatment
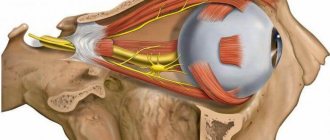
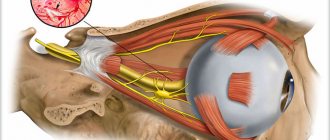
Hypoglossal nerve
This treatment should be aimed specifically at the very cause of the inflammatory process in the nerve fiber. Depending on the reason, it may consist of the following parts:
- If the cause of the disease is any neoplasm or cyst, treatment should be surgical. First, tissue outgrowths are removed, and then their histological examination is carried out. Usually, the symptoms of neuritis disappear immediately after surgery.
- If a patient is diagnosed with tuberculosis, further treatment is carried out exclusively in specialized tuberculosis medical institutions. There therapy consists of anti-tuberculosis drugs.
- For a sore throat, the patient is prescribed a course of antibiotics.
- For B12 deficiency anemia, medications with vitamin B12 are prescribed.
Symptomatic therapy

Nonsteroidal anti-inflammatory drugs
Symptomatic treatment is aimed at relieving pain and impaired tongue mobility. For this purpose, the following drugs can be used:
- Non-steroidal anti-inflammatory drugs:
- with a pronounced analgesic effect: Ketorolac, Analgin, Baralgin, Ketanov;
- with a pronounced anti-inflammatory effect: Diclofenac, Mefenamic acid, Indomethacin;
- with antipyretic effect: Paracetamol, Ibuprofen.
- Antispasmodics: No-shpa, Spazmalgon.
- Diuretics: Furosemide, Torasemide, Lasix.
All these drugs should be taken only after consultation with the treating doctor. You can add multivitamin preparations to the treatment regimen, which include B vitamins. These substances take part in the restoration of nerve bundles. Sometimes the cause of inflammation lies precisely in the lack of these vitamins.
Neuritis of the submandibular nerve is a very unpleasant disease. During his attacks, the patient experiences severe pain in the tongue and speech impairment. Sometimes the pain can cover part of the head, and this disease is mistaken for migraine. A neurologist treats this condition. After making a diagnosis and identifying the cause of pain and inflammation, he prescribes etiological and symptomatic treatment. Symptomatic therapy consists of anti-inflammatory drugs, antispasmodics and diuretics. Sometimes B vitamins are included in the treatment regimen.
Function
The nucleus of the hypoglossal nerve (lat. Nucleus n.hypoglossi) is motor, located in the middle parts of the posterior part of the medulla oblongata. From the side of the rhomboid fossa, it is projected into the region of the triangle of the hypoglossal nerve (lat. trigonum n.hypoglossi). The nucleus of the hypoglossal nerve consists of large multipolar cells and a large number of fibers located between them, with which it is divided into three more or less separate cell groups. Each of these groups innervates its own tongue muscle. In evolutionary terms, these neurons are identical to the motor neurons of the anterior horns of the spinal cord.
The hypoglossal nerve innervates the muscles of the tongue: styloglossus (lat. m.styloglossus), hyoglossus (lat. m.hyoglossus) and genioglossus (lat. m.genioglossus), as well as the transverse and rectus muscles of the tongue. Innervation of voluntary movements is carried out along the corticonuclear pathways, which begin in the precentral gyrus of the cerebral cortex. The nucleus of the hypoglossal nerve receives impulses primarily through the contralateral corticonuclear pathway. In addition, information is carried to it by afferent fibers from the reticular formation, the nucleus of the solitary tract (lat. nucleus tractus solitarii) (receiving taste fibers from the facial and glossopharyngeal nerves), from the midbrain and from the nuclei of the trigeminal nerve. Accordingly, the nucleus of the hypoglossal nerve and the nerve itself are components of reflex arcs that provide swallowing, chewing, sucking and licking.