Description of the sub-item
Peroneal (peroneal) nerve palsy
Plantar nerve palsy (plantar nerve neuropathy, Morton's metatarsalgia) (G57.6) is a pain syndrome in the forefoot caused by compression of the branches of the plantar nerve by perineural fibroma or other factors.
| 1 - deep transverse metatarsal ligament of the III and IV fingers; 2 - 4th plantar digital nerve; 3 - lateral plantar nerve; 4 - medial plantar nerve |
It is more common in women aged 40–50 years, and has a one-sided pain pattern.
Biomechanical obstacles leading to irritation and compression of the plantar nerve can be caused by foot trauma (30%), wearing tight high-heeled shoes (70%), prolonged squatting (50%), and transverse flat feet (50%).
What is not recommended to do
It is strongly recommended not to delay visiting your doctor if you experience knee pain that you have not experienced before.
Sudden pulsating and shooting pain indicates nerve damage; only a doctor can determine the cause.
With prolonged progression of the pathology, nerve endings atrophy, blood circulation and nerve conduction in the extremities are disrupted, which negatively affects the patient’s ability to work.
Self-medication is prohibited ! In addition to the fact that lotions and anti-inflammatory drugs cannot eliminate pinching, you can harm yourself with them, further increasing the source of inflammation.
You should not exercise until the problem is resolved.
Any load provokes increased production of joint fluid, which will accumulate in the bursa, squeezing the inflamed nerve even more. Reconsider your approach to nutrition: eliminate refined sugar, fatty and fried foods, canned food, processed foods, salty and spicy foods, smoked foods, coffee, tea, and alcohol. All these products contribute to the development of vascular pathologies, degeneration of cartilage and bones, and therefore can provoke neuralgia.
Wear only comfortable shoes and clothing that fits properly . Leave too-tight jeans and high heels in the closet.
It is not recommended to sit in one position for a long time - get up every 40 minutes to warm up.
In bad weather, protect your joints from hypothermia - compression thermal underwear can help with this.
Peroneal nerve neuropathy: causes and consequences
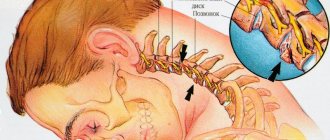
Peroneal neuropathy is damage to the lateral popliteal nerve (peroneal nerve). This is one of the most common neuropathies of the lower extremities. Typically, the cause of the injury is a hip or knee injury.
The peroneal nerve separates from the sciatic nerve at the hip and runs down the entire leg to the outside of the knee where it wraps around the fibular head. At this point, the lateral popliteal nerve is covered only by fascia and skin, and is therefore extremely sensitive to any kind of injury.
In the region of the peroneus longus muscle, it divides into two terminal branches - the superficial and deep peroneal nerves.
The peroneal nerve with all its branches is responsible for the innervation of the muscles that extend the foot and toes, as well as sensitivity along the outer surface of the lower leg, the back of the foot and its toes.
Neuropathy of the lateral popliteal nerve is most common among dancers.
The most common cause of peroneal nerve neuropathy is trauma. The common peroneal nerve can be damaged at any point, but the most common site of nerve damage is the knee.
The nerve can be damaged during a fracture, as well as while wearing a cast.
The second most common cause of peroneal nerve neuropathy is compression. As a rule, this occurs in people who are forced to work in the same position for a long time or make repetitive movements.
- disruption of the blood supply to the nerve - nerve ischemia,
- incorrect position of the leg during surgery,
- entering a nerve with a needle during an intramuscular injection,
- toxic damage to peripheral nerves - as a result of renal failure, diabetes or drug use,
- foot drop - inability to raise the front edge of the foot (where the toes are located),
- loss of ability to walk and stand on your heels,
- when walking, the patient is forced to raise his legs high so as not to cling to the floor with his toes - the so-called “cock gait”,
- severe pain in the foot and lateral surface of the leg, aggravated by squatting,
- the appearance of a horse's foot - the foot hangs down and inward with curled toes that cannot be unclenched,
- with chronic neuropathy, muscle atrophy develops. This is especially noticeable if the nerve is affected in only one leg.
A doctor may diagnose peroneal nerve damage during a physical examination, where he will ask the patient to walk, squat, and stand on his heels.
Additional tests, tests and studies are needed to identify the cause of nerve damage.
In particular, we are talking about nerve conduction studies, which can show where exactly the nerve is damaged and whether other branches are involved in this process.
Electromyography allows you to assess the extent of nerve damage, as well as make a prognosis for the injury.
Treatment depends on the cause of the nerve damage. If the cause is injury, then over time all the symptoms will subside on their own. Drug treatment for traumatic and compressive nerve damage includes the use of non-steroidal anti-inflammatory drugs and B vitamins.
Physiotherapy can speed up nerve recovery and also get rid of unpleasant symptoms. The use of orthoses - special fixing brackets - allows you to correct the cock's gait, fixing the foot in the correct position and not allowing it to sag.
Before purchasing orthoses, you should consult your doctor.
In complex cases, treatment of peroneal nerve neuropathy includes surgery, during which the anatomical integrity of the nerve is restored or the cause of its compression is eliminated.
If the cause of nerve damage is renal failure or diabetes mellitus, you should focus on treating these diseases with parallel therapy for neuropathy.
The prognosis for patients with peroneal nerve injury is generally good.
- Causes of hip pain: meralgia paresthetica - Bernhardt-Roth syndrome. Causes and symptoms of meralgia paresthetica. Risk factors. Diagnosis and treatment of meralgia paresthetica.
- Damage to the sciatic nerve - causes, main symptoms, methods of diagnosis and treatment.
- Trigeminal nerve lesions and neuralgia are a chronic pain disorder affecting the trigeminal nerve. Diagnosis and treatment methods for trigeminal neuralgia.
Treatment
Treatment methods directly depend on the cause of neuropathy.
If the cause is mechanical damage (from shoes, bandages, etc.), it is enough to simply eliminate this factor. If the cause lies in another disease, then treatment is aimed primarily at it. The following measures are used to eliminate neuropathy:
- non-steroidal anti-inflammatory drugs;
- B vitamins;
- medications that improve nerve conduction;
- stimulating blood circulation;
- antioxidants;
- amplipulse;
- magnetic therapy;
- ultrasound;
- electrical stimulation;
- massage;
- acupuncture.
However, we would like to remind you that only your attending physician can identify the true cause of the disease. Therefore, under no circumstances self-medicate, but trust the professionals.
Treatment of plantar nerve damage
The disease manifests itself as a sharp shooting pain in the area of the sole (90%), radiating to the 3rd interdigital space. In 50% of cases, patients are bothered by aching, paroxysmal pain in the sole area. At the beginning of the disease, pain in the sole area appears when walking, then occurs spontaneously at night.
An objective examination of the patient reveals pain on the sole of the foot in the area of the 3rd interdigital space at the base of the III and IV fingers (90%), hypoesthesia of the fingertips in the zone of innervation of the plantar nerve, paresthesia in the foot (60%). A characteristic click is noted with simultaneous pressure on the interdigital spaces, and increased pain when squeezing the foot in the transverse direction.
Treatment is prescribed only after confirmation of the diagnosis by a medical specialist. Symptomatic treatment is carried out (decongestants, analgesics). Physiotherapy, massage, novocaine and hydrocortisone blockades, orthopedic correction are indicated. Surgical intervention is required if conservative treatment is ineffective.
There are contraindications. Specialist consultation is required.
- Tramadol (analgesic). Dosage regimen: IV, IM, SC in a single dose of 50-100 mg, possible repeated administration of the drug after 4-6 hours. The maximum daily dose is 400 mg.
- Voltaren (non-steroidal anti-inflammatory drug). Dosage regimen: IM at a dose of 75 mg (contents of 1 ampoule) 1 time/day.
- Ketoprofen (non-steroidal anti-inflammatory drug). Dosage regimen: IM: 100 mg 1-2 times a day; after pain relief, it is prescribed orally in a daily dose of 300 mg in 2-3 doses, a maintenance dose of 150-200 mg/day.
- Diacarb (diuretic). Dosage regimen: 0.25 g orally 2 times a day (morning, afternoon) for 5-7 days.
- Milgamma (B complex of vitamins). Dosage regimen: therapy begins with 2 ml intramuscularly 1 time per day for 5-10 days. Maintenance therapy - 2 ml IM two or three times a week.
How and with what to treat
Before a patient is prescribed treatment for a pinched nerve in the knee joint at home, confirmation of the diagnosis is required. Diagnosis is carried out using X-rays, ultrasound of soft tissues, and in some cases MRI and CT are required.
Further, based on individual indications, medications and physical therapy are prescribed.
Medicines and procedures
First of all, treatment aims to eliminate pain, inflammation and swelling in the knee. For this purpose, non-steroidal drugs with anti-inflammatory and analgesic properties are used: Movalis, Diclofenac, Ibuprofen. They should be consumed in precisely prescribed dosages, otherwise side effects are possible . Local NSAIDs are applied in the form of an ointment or gel.
To reduce pain, the patient is advised to follow a gentle daily routine and not subject the sore leg to unnecessary stress.
If the nerve is compressed as a result of muscle spasms, the problem is eliminated with the help of muscle relaxants and antispasmodics.
Excessively severe pain is eliminated by injections of drugs that block the transmission of nerve impulses.
Physiotherapy is a mandatory part of the treatment of a damaged nerve .
They allow you to quickly restore nerve conduction, relieve swelling and inflammation, and relieve pain.
A patient with neuralgia is prescribed electrical stimulation of soft tissues, paraffin and ozokerite applications, magnetic therapy, UHF, laser therapy, massage, reflexology or acupuncture.
Exercise therapy
To restore the functionality of the joint, it is recommended to perform exercises when a nerve is pinched in the knee. It is important to monitor the technique of performing movements and measure the load without overloading the leg.
During the period of exacerbation of the inflammatory process, gymnastics is prohibited!
Don't forget to keep your knees toned and slightly tucked to avoid injury. Perform 5 laps:
- walking in place with knees up - 30 seconds;
- rotation of the pelvis - 20 times;
- abduction of each hip to the side - 20 times;
- sitting on a chair, flexion and extension at the knee - 25 times;
- standing a meter from the wall, lean forward and rest your palms on it, put one leg forward and bend at the knee, stretching your back thigh - 30 seconds;
- squats to parallel with the floor - 50 times;
- in a standing position, legs together, slightly bend your knees and place your palms on them, rotate 30 times to the right, then 30 times to the left.
To complete the light gymnastics, stand up straight with your feet shoulder-width apart. Hold your elbows with your palms and bend forward completely, hanging parallel to your straight legs. This relaxes the lower back and stretches the hamstrings. Stay in this position for 30-60 seconds.
Folk remedies
Various compresses, lotions, and ointments are also effective to relieve swelling and inflammation.
You should definitely warn your doctor about their use and consult for contraindications.
It is important to remember that folk remedies do not eliminate pinching, but only relieve symptoms of inflammation and pain.
Without medical help, treating neuralgia exclusively with traditional methods is ineffective.
Traditional medicine offers the following as symptomatic remedies:
- make an ointment from butter (1 tablespoon) and ammonia (1 teaspoon), apply to the joint, wrapping it in a warm cloth overnight;
- another ointment recipe: mix 200 g of honey with aspirin powder (pre-grind 10 tablets), apply to the sore joint and wrap in cling film for several hours;
- a compress of grated raw horseradish quickly relieves pain: just put the pulp in gauze and apply it to the knee for 30 minutes;
- prepare a decoction of wormwood (1 tablespoon of the plant in 2 cups of boiling water), wipe the joint for pain twice a day;
- Vodka (0.5 l) mixed with 1 tbsp is also effective as a rub. a spoonful of grated garlic or garlic oil;
- infusion of lingonberry leaves (1 teaspoon of the plant in 2 cups of boiling water) take 100 ml three times a day.
Popliteal syndrome
This syndrome usually develops in middle-aged people who have been suffering from vertebrogenic chronically recurrent dorsalgia for a long time with frequent exacerbations, usually with lumbosacral radiculopathy. Conditions for neuromyoosteofibrosis in the muscles of the popliteal region in most cases are caused by a violation of the configuration of the spine (with a violation of the motor stereotype) and/or vertebrogenic compression-ischemic radiculopathy, caudopathy and/or [.
] multilevel compression-ischemic radiculoneuropathy (double and even triple crash syndrome). In particular, with spondylolisthesis (which is caused by degenerative-dystrophic pathology of the spinal column), with hyperlordosis, when the posterior edge of the pelvis rises, and therefore the ischial tubercle, i.e.
where the hamstring muscles begin, there is an inevitable stretching of the ischiocrural muscles that form the popliteal fossa. G. Gill (1951), Z. Harnach (1966) and others believe that in cases of spondylolisthesis, shortening of the posterior muscles of the thigh occurs only due to impulses from the roots of the compressed cauda equina, because
after laminectomy this shortening disappears. It is also necessary to consider the readiness of the ischiocrural muscles for tonic tension, taking into account not only peripheral, but also central influences: this is an element of the protective reflex, which, similar to the adductor one, requires strengthening of extrapyramidal and inhibition of pyramidal activity.
Initially, constant pain appears in the popliteal fossa, in the lower leg, painful cramps in the calf muscles occur at rest or when walking. Soon, paresthesia appears along the posterior surface of the leg and on the foot, and paresis of the foot and diffuse wasting of the leg muscles develop. On the affected side, the Achilles reflex is reduced and the knee reflex is increased.
Examination reveals tissue swelling in the popliteal fossa. By palpation, painful areas of compaction are determined in the biceps, semimembranosus, semitendinosus and triceps muscles, in the places of attachment of their tendons in the popliteal fossa. Pain points are determined in the projection of the sciatic nerve in the upper corner, the peroneal nerve in the lateral corner, or the tibial nerve in the lower corner or in the center of the popliteal fossa.
A positive Tinel sign indicates the location of nerve compression. Reduced pulse in the artery of the dorsum of the foot. The patient cannot fully straighten his leg due to the presence of partial contracture due to damage to the popliteal muscles. A positive muscle-trunk sign of Lassegue is revealed. When walking, the patient limps on the leg as a result of its pseudo-shortening or due to weakness of the foot.
In the area of the popliteal fossa, the peroneal and tibial nerves can be compressed together or separately, by an accumulation of adipose tissue, a Becker cyst, a popliteal artery aneurysm, varicose vein, or fibroma. Clinical manifestations are minimal for a long time. Patients complain of pain in the leg (mainly along the back of the thigh and lower leg), which intensifies when walking.
In most cases, the diagnosis is made several years after the first symptoms appear. Vertebrogenic pathology is assumed, repeated radiographs of the spine and knee joint are taken. Often, patients themselves feel a “tumor” in the popliteal fossa, pressure on which causes pain in the leg.
Treatment is aimed at compensating the underlying vertebral pathological process (syndrome) using medication (NSAIDs, analgesics, muscle relaxants, etc.) and non-drug treatment (PTL, exercise therapy, acupuncture, post-isometric relaxation, manual therapy and various traction techniques).
Popliteal syndrome is a symptom complex that includes signs of vertebrogenic neuromyoosteofibrosis in the popliteal fossa, compression of the sciatic nerve or its main branches (tibial or peroneal) and/or popliteal vessels.
This syndrome usually develops in middle-aged people who have been suffering from vertebrogenic chronically recurrent dorsalgia for a long time with frequent exacerbations, usually with lumbosacral radiculopathy. The conditions for neuromyoosteofibrosis in the muscles of the popliteal region are in most cases caused by a violation of the configuration of the spine (with a violation of the motor stereotype) and vertebrogenic compression-ischemic radiculopathy, caudopathy or multi-level compression-ischemic radiculoneuropathy (double and even triple crash syndrome)).
In particular, with spondylolisthesis (caused by degenerative-dystrophic pathology of the spinal column), with hyperlordosis, when the posterior edge of the pelvis rises, and therefore the ischial tubercle, i.e. where the hamstring muscles begin, there is an inevitable stretching of the ischiocrural muscles that form the popliteal fossa. G.
Gill (1951), Z. Harnach (1966) and others believe that in cases of spondylolisthesis, shortening of the posterior thigh muscles occurs only due to impulses from the roots of the compressed cauda equina, because after laminectomy this shortening disappears. It is also necessary to consider the readiness of the ischiocrural muscles for tonic tension, taking into account not only peripheral, but also central influences: this is an element of the protective reflex, which, similar to the adductor one, requires strengthening of extrapyramidal and inhibition of pyramidal activity.
Treatment is aimed at compensating the underlying vertebral pathological process (syndrome) using medication (NSAIDs, analgesics, muscle relaxants, etc.) and non-drug treatment (PTL, exercise therapy, acupuncture, post-isometric relaxation, manual therapy and various traction techniques).
Causes
Nerve root entrapment is mechanical compression that causes inflammation, swelling and pain of the nerve trunk along its entire length.
The danger of pinching lies in muscle atrophy, complete or partial loss of sensation in the limb. The rest of the time the person suffers from shooting pain in the leg.
Experts answer negatively to the question of whether a nerve in the knee can suddenly become pinched.
This is explained by the fact that mechanical pressure on the nerve is exerted by injured periarticular tissues damaged for the following reasons:
- diseases of the musculoskeletal system that provoke swelling of the joint (arthritis, arthrosis, coxarthrosis, polyarthritis, bursitis, etc.);
- intervertebral disc deformation (osteochondrosis, spondylosis, protrusion, hernia);
- excess weight;
- soft tissue injuries (torn meniscus, tendons, ligaments);
- deformation of bones or cartilage due to injury (fracture, dislocation);
- formation of osteophytes;
- hormonal disorders;
- muscle spasm;
- wearing uncomfortable shoes and too tight jeans;
- staying in a sitting position for a long time, crossing your legs;
- increased physical activity;
- autoimmune reaction of the body;
- taking drugs;
- long-term immobilization of the joint after surgery or fracture;
- vascular diseases.
All these reasons are similar in one thing - they provoke swelling in the knee, as a result of which the nerve is damaged.
After the initial diagnosis has been established, the patient is provided with assistance in the form of symptomatic therapy with medications, physiotherapy and exercises. How to treat a pinched nerve in the knee joint will be discussed below.
G57.3 Damage to the lateral popliteal nerve
Health disorder related to the group of damage to individual nerves, nerve roots and plexuses
262,347 people diagnosed with damage to the lateral popliteal nerve
0 died with a diagnosis of Lesion of the lateral popliteal nerve
0% mortality for the disease Damage to the lateral popliteal nerve
Men are diagnosed with Damage to the lateral popliteal nerve. No deaths were identified.
mortality in men with the disease Damage to the lateral popliteal nerve
women are diagnosed with Damage to the lateral popliteal nerve. No cases of death have been identified.
mortality in women due to the disease Damage to the lateral popliteal nerve
The disease most often occurs in men aged 55-59
In men, the disease is least common at the age of 0-1.95
In women, the disease is least common at the age of 0-1.95
The disease most often occurs in women aged 55-59
Absence or low individual and social danger
* — Medical statistics for the entire group of diseases G57 Mononeuropathies of the lower extremity
The causes of disease and damage to the nerve plexuses and roots can be varied. They have both external and internal genetic significance, while sometimes being some kind of disease. the fundamental reason is the inflammatory processes of neighboring zones. This can be either muscle damage or bone damage.
Inflammation spreads very quickly throughout the body and can lead to irreversible consequences. genetic predisposition. The presence of certain genotypic or phenotypic characteristics in our genes does not depend on us at all, it depends on heredity and our ancestors, but if there is something wrong in the genes, then the disease is practically unavoidable.
Be careful. Get tested more often to identify your hereditary diseases at an early stage and prevent their development. wrong lifestyle. This is exactly what is completely up to us! Excessive addiction to alcohol, nicotine addiction, extra pounds - these are many, many health problems. It seems that if you just start eating right and running in the morning, everything will get better and any illness will subside.
Clinical picture
The early stages of the disease are characterized by a number of pronounced symptoms, such as: revitalization of reflexes (tendon and periosteal) paresthesia hyperesthesia pain and the appearance of pain points anesthesia of certain types of sensitivity Lasegue's symptom Bechterev's symptom Neri's symptom Dzheren's symptom changes in the composition of the periarticular fluid swelling of the radicular nerve
Sciatic nerve and intramuscular injections
The buttocks are often chosen as a site for intramuscular injections due to their large muscle mass. When performing intramuscular injections in this area, it is very important to know the location and path of the sciatic nerve. If the injection site hits the sciatic nerve, there is a high risk of damage to it, which could have serious consequences for the functioning of the leg in the future.
If the buttocks are divided into four squares, then it is clear that the sciatic nerve passes through the lower quadrants. Therefore, the only safe place for intramuscular injections into the buttocks is the upper outer quadrant.
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 |
| Number of sick people | 0 | 0 | 0.1 | 8 | 8 | 10 | 10 | 0 | 0 | 0.1 | 8 | 8 | 10 | 10 |