Facial hemispasm (hemifacial spasm) is an attack caused by one reason or another, characterized by muscle spasms of one half of the face. Thanks to its pronounced symptoms, recognizing this disease is not particularly difficult: during an attack, the patient’s face becomes asymmetrical. After normalization of the condition, the muscles return to normal. Pathology not only creates a cosmetic defect, but also causes physical problems for the patient. Over time, the patient's visual acuity decreases and general health worsens. In the absence of adequate treatment, the frequency of attacks increases over time.
Features and clinical picture
The disease mainly affects middle-aged people. Only about 30% of cases occur in people under thirty years of age. Women get sick twice as often.
Facial hemispasm is a periodically recurring spasm of the facial muscles.
The possible course of the disease can most often be characterized as follows:
- Typical. Infrequent twitching occurs around the eye. The entire half of the face is gradually affected, and the spasms become more intense. Vision in the affected eye is difficult or disappears.
- Atypical. Ascending contraction of the cheek muscles.
- Post-paralysis. Develops after paralysis from wounds, trauma, neuritis of the facial nerve. In this form, voluntary facial movements lead to involuntary twitching (on any part of the face); it is the most difficult to treat.
The nature of muscle contractions can be either clonic (tension followed by relaxation) or tonic (constant tension).
Spasms are absolutely painless, but can cause significant discomfort. May continue even during sleep.
When there is a pause between seizures, the face is symmetrical in most cases. But some patients experience weakness on the affected side: when smiling, one corner of the mouth is slightly drooping, and the symptom of “eyelashes” is observed (when the eyelids are tightly closed, the eyelashes do not sink into the folds of the skin, but stick out).
Patients often experience emotional swings, depression, and anxiety.
Information
Sources and literature
- Protocols for the diagnosis and treatment of diseases of the Ministry of Health of the Republic of Kazakhstan (Order No. 239 of 04/07/2010) Extrapyramidal disorders. Guide to diagnosis and treatment. Edited by V.N. Stolz. Moscow 2002 Neurology. Edited by M. Samuels. Moscow 1997 D.R. Shtulman. Neurology. Moscow 2005 E.V. Schmidt. Handbook of Neurology. Moscow 1989 L.R. Zenkov, M.A. Ronkin. Functional diagnosis of nervous diseases. Moscow Ya.Yu. Popelyansky. Diseases of the peripheral nervous system. Moscow 1989
Information
List of developers:
| № | Developer | Place of work | Job title |
| 1. | Kadyrzhanova Galiya Baekenovna | RDKB "Aksai", psychoneurological department No. 3 | Head of department |
| 2. | Mukhambetova Gulnara Amerzaevna | Department of Nervous Diseases, KazNMU | Assistant, Candidate of Medical Sciences |
| 3. | Balbaeva Ayim Sergazievna | RDKB "Aksai", psychoneurological department No. 3 | Neuropathologist |
| 4. | Serova Tatyana Konstantinovna | RDKB "Aksai", psychoneurological department No. 1 | Head of department |
Causes
Depending on the causes of occurrence, hemispasm of the facial nerve is divided into:
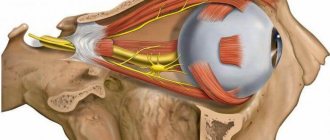
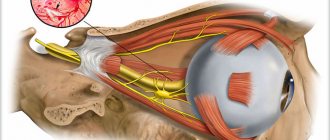
- Primary. It consists of the so-called neuro-vascular conflict. The conflict occurs as a result of the impact of a pulsating vessel on the nerve trunk.
- Secondary. The conflict in this case occurs due to displacement of the vessel under the influence of tumors, aneurysms, vascular malformations (formation of vascular glomeruli).
The disease has clear symptoms: during an attack, the affected part becomes asymmetrical to the healthy part, the frequency of spasms increases over time
Less commonly, the causes of hemispasm are:
- pontine cerebral infarction;
- acute otitis media;
- multiple sclerosis;
- hemangioma of the temporal region;
- injuries to the bones of the brain and facial parts of the skull;
- deformation of bone tissue;
- taking medications, drugs;
A hereditary pattern has not yet been identified.
Facial hemispasm can be aggravated by the following factors:
- stress;
- overwork;
- bright light;
- Sometimes aggravation is promoted by: intensive chewing of food, touching, speech activity (conversation).
Trigeminal neuralgia :: Symptoms, causes, treatment and code according to ICD-10
Trigeminal neuralgia.
Trigeminal neuralgia
The disease is characterized by short paroxysms of unilateral intense excruciating shooting pain in the innervation zone of one or all branches of the trigeminal nerve, often provoked by touching the skin of the trigger zone. Trigger zones - areas of the skin of the lips, nasolabial folds, wings of the nose, eyebrows. Frequency: 6-8 per 100,000 population (women get sick more often, the disease develops over the age of 40 years.
Neuralgia is divided into two forms: primary (essential, idiopathic, typical) and secondary (symptomatic).
Attacks of excruciating pain occur, localized in the area of innervation of one or more branches of the trigeminal nerve. Painful paroxysms last from several seconds to several minutes. They stop suddenly. There is no pain during the interictal period. An attack of pain is usually accompanied by vegetative manifestations (facial hyperemia, lacrimation, increased salivation), as well as reflex contractions of the facial and masticatory muscles. During an attack, the patient freezes in a suffering pose and is afraid to move. Sometimes patients take peculiar positions, hold their breath or, conversely, breathe heavily, squeeze the painful area or rub it with their fingers. On the skin of the face, mucous membranes and even teeth, mainly around the mouth and in the gum area, there are often small areas, mechanical or thermal irritation of which provokes the occurrence of painful paroxysm (trigger, trigger or algogenic zones). Most often, pain with trigeminal neuralgia occurs in the area of the II or III branches, or in the area of both branches. Neuralgia of the first branch is rare, so when diagnosing it, it should be remembered that this usually happens when the superior orbital fissure is affected (frontitis, local inflammatory process, etc.). When examined during or after an attack, it is possible to identify pain points at the exit site of the branches of the trigeminal nerve, as well as hyperesthesia in the corresponding areas. The pain with neuralgia has a different character, most often it is burning, shooting, tearing, cutting, stabbing, “electric shock”. Sometimes painful attacks follow each other with an interval of several minutes. Remissions occur during treatment and, less commonly, spontaneously. Their duration ranges from several months to several years. Remission occurs quickly after alcoholization of the peripheral branches of the trigeminal nerve, however, with each subsequent alcoholization, the duration of remission is shortened, and the therapeutic effectiveness of the method decreases. As a result of alcoholization, destructive changes develop in the nerve and the phenomena of iatrogenic neuritis (neuropathy) of the trigeminal nerve are added to neuralgia. In addition to unilateral ones, there are also bilateral trigeminal neuralgia.
Trigeminal neuralgia with a predominance of the peripheral component of pathogenesis includes odontogenic neuralgia of the trigeminal nerve, dental plexalgia, postherpetic neuralgia, neuralgia with damage to the semilunar ganglion, neuralgia of individual nerves of the main branches of the trigeminal nerve and Odontogenic neuralgia is more often manifested by pain in the innervation zones of the 2nd and 3rd ver. vey of the trigeminal nerve.
The course of odontogenic lesions of the trigeminal nerve is characterized by persistence and significant severity of both pain and autonomic components. A feature of odontogenic neuralgia is that they can continue for a long time, despite the elimination of the main disease process that led to the development of neuralgia.
Dental plexalgia should be distinguished from such neuralgia, which is manifested by pain in the upper and lower jaws, and pain in the upper jaw occurs 2 times more often than in the lower jaw, since in approximately 50% of people the lower dental plexus is absent. In addition, trigeminal neuralgia should be differentiated from arthrosis of the temporomandibular joint, phantom toothache, multiple sclerosis, and glossopharyngeal neuralgia.
The most common cause is compression of the trigeminal nerve by the arteries or veins of the posterior cranial fossa, or by a vascular loop in the presence of a vascular anomaly. The branches of the trigeminal nerve may also be compressed in the bony canals of the skull base through which they pass.
Narrowing of bone canals can be congenital or acquired during chronic inflammatory processes in adjacent areas (sinusitis, caries). Less commonly, the trigeminal nerve is compressed by a tumor of the cerebellopontine region. The process usually begins with a peripheral source of pain impulses.
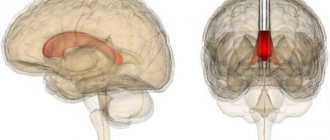
Irritation of various levels of the trigeminal nerve system and peripheral vegetative formations of the face, overirritation of the pontobulbospinal pain conductors and reticular formation with the formation of a multineuronal neuralgia reflex, as well as the involvement of suprasegmental formations of the brain with the development of a dominant in the thalamus and cerebral cortex play a role.
First of all, the anticonvulsant drug carbamazepine (finlepsin, tegretol) is prescribed in individually selected doses. Use internally, starting with 1 tablet. (0.2 g) 1-2 times a day daily, gradually increasing the dose by 1/2 table. Or a whole tablet. Or use phenytoin 300-600 mg/day.
To enhance the effect of the anticonvulsant, antihistamines are used - intramuscularly 2 ml of a 2.5% solution of diprazine (pipolfen) or 1 ml of a 1% solution of diphenhydramine at night. Antispasmodics and vasodilators are indicated.
Physiotherapeutic methods include ionogalvanization with novocaine, amidopyrine, diadynamic currents, and ultraphonophoresis with hydrocortisone.
If drug therapy is ineffective, surgical intervention is resorted to: microsurgical decompression of the branches of the trigeminal nerve at their exit from the brain stem or transection of the branches of the nerve proximal to the Gasserian ganglion. For dental plexalgia, treatment should begin with the prescription of general and local anesthetics.
First of all, non-narcotic analgesics are used. All patients are prescribed local anesthetics: 5-10% anesthetic or lidocaine ointment, which is lightly rubbed into the pre-dried mucous membrane of the gums at the site of pain. The analgesic effect occurs immediately when rubbing the ointment in and lasts 15-30 minutes. Repeated rubbing is carried out according to indications up to 3-10 times a day.
| Selected clinics | Phones | City (metro) | Price of services |
| Family Clinic on Bolshaya Serpukhovskaya | +7(495) 662..show Recording +7(495) 662-58-85 | Moscow (metro station Serpukhovskaya) | 29945ք(90%*) |
+7(495) 662-58-85Moscow (metro station Ilyich Square)29945ք(90%*)Family Clinic on Hospital Square+7(495) 662..showRecord
+7(495) 662-58-85Moscow (metro station Baumanskaya)29945ք(90%*)Family Clinic on Festivalnaya +7(495) 662..showRecord
+7(495) 662-58-85Moscow (metro station Rechnoy Vokzal)29945ք(90%*)Family Clinic on Yaroslavskoye Highway+7(499) 519..showRecord
+7(499) 519-36-68+7(499) 969-20-02+7(495) 662-58-85Moscow (m. VDNKh)29945ք(90%*)Family Clinic on Pervomaiskaya +7(495) 662..showRecord
+7(495) 662-58-85Moscow (metro station Izmailovskaya)29945ք(90%*)Family Clinic on Kashirskoe Highway+7(495) 662..showRecord
+7(495) 662-58-85Moscow (m. Kashirskaya)29945ք(90%*)Family Clinic in Pokrovsky+7(499) 519..showRecord
+7(499) 519-35-86+7(499) 969-20-02+7(495) 662-58-85Moscow region29945ք(90%*)Family Clinic on Universitetsky Prospekt+7(495) 662..showRecord
+7(495) 662-58-85Moscow (m. University)29945ք(90%*)Family Clinic on Heroev Panfilovtsev+7(495) 662..showRecord
+7(495) 662-58-85Moscow (metro station Skhodnenskaya)29945ք(90%*)* – the clinic does not provide 100% of the selected services. More details by clicking on the price.
42a96bb5c8a2ac07fc866444b97bf1 Content moderator: Vasin A.S.
Source: //kiberis.ru/?p=30822
Consequences
Complications arise if help is not provided in a timely manner:
- The occurrence of blepharophimosis (reduction in the size of the palpebral fissure) occurs due to constant tension of the orbicularis oculi muscle.
- Partial hearing loss.
- Ataxia (random contraction of different muscle groups with complete preservation of muscle strength).
- Since the pathology mainly affects middle-aged people, they are at risk of maintaining symptoms for life.
The onset of facial nerve disease is accompanied by rare but periodic contractions of the circular muscles of one of the eyes
Diagnostics
To make a diagnosis, a collected history of the disease and examination of the cranial (cranial) nerves are usually sufficient.
Additional examinations:
- MRI with contrast may show facial nerve entrapment (by a mass or blood vessel) as the obvious cause of hemispasm, but in most cases the examination is normal.
- Electromyography will help to trace neuromuscular transmission, the conduction of excitation along the nerve. This test is rarely used for diagnosis.
Differential diagnosis is carried out in patients with:
- nervous tics;
- tetany - involuntary painful muscle spasms. May be a symptom of parathyroid dysfunction, calcium deficiency and excess phosphate;
- focal epileptic seizures;
- myokymia of the facial nerves;
- tardive dyskinesia.
There are several treatment methods in which hemifacial spasm was eliminated completely or partially blocked
Rules for hospitalization in the NCDR
The indication for hospitalization of a patient is the need to provide qualified, specialized and high-tech medical care with round-the-clock medical supervision.
Hospitalization of patients at the NCDR is carried out in accordance with the List of medical services provided by the NCDR.
Hospitalization of a patient to a hospital within the framework of the Statewide Volume of Medical Care is carried out as planned - by referral from primary health care specialists (polyclinics) or a medical organization through the Hospitalization Bureau Portal.
List of diseases
subject to rehabilitation treatment at the NCDR
| № | Nosology name | ICD – 10 |
| 1. | Cerebral palsy-Spastic cerebral palsy-Spastic diplegia-Infantile hemiplegia-Dyskinetic cerebral palsy-Atactic cerebral palsy | G 80G 80.0G 80.1G 80.2G 80.3G 80.4 |
| 2. | Consequences of intracranial injury | T 90.5 |
| 3 | Consequences of a spinal cord injuryConsequences of a nerve injury of the upper limbConsequences of a nerve injury of the upper limb | Т 91.3Т 93.4Т 92.4 |
| 4 | Damage to individual nerves, nerve roots and plexuses, polyneuropathy: - Neuralgia after herpes zoster - Other lesions of the facial nerve Damage to nerve roots and plexuses - Damage to the brachial plexus - Damage to the lumbosacral plexus - Other lesions to the nerve roots and plexuses Mononeuropathies of the upper limb - Carpal tunnel syndrome - Others lesions of the median nerve - Damage to the ulnar nerve - Damage to the radial nerve - Other mononeuropathies of the upper limb Mononeuropathies of the lower limb - Damage to the sciatic nerve - Damage to the femoral nerve Polyneuropathies and other lesions of the peripheral nervous system - Hereditary and idiopathic neuropathy - Hereditary motor and sensory neuropathy - Neuropathy in combination with hereditary ataxia -Other hereditary and idiopathic neuropathiesInflammatory polyneuropathy:-Guillain-Baré syndrome-Other inflammatory polyneuropathies-Other polyneuropathies:-Drug-induced polyneuropathy-Polyneuropathy caused by other toxic substances | G 53.0G 51.8G 54G 54.0G 54.1G 54.8G 56G56.0G56.1G56.2G56.3G56.8G57G57.0G57.2 G 60G 60.0G 60.2G 60.8G 61.0G 61.G 62G 62.0G 62. 2 |
| 5 | Consequences of inflammatory diseases of the central nervous system | G 09 |
| 6. | -Hemiplegia-Flaccid hemiplegia-Spastic hemiplegia-Hemiplegia unspecified-Paraplegia and tetraplegia-Flaccid paraplegia-Spastic paraplegia-Flaccid tetraplegia-Spastic tetraplegia-Other paralytic syndromes-Diplegia of the upper limbs-Monoplegia of the lower limb-Monoplegia of the upper limb-Cauda equina syndrome | G81G81.0G81.1G81.9G82G82.0G82.1G82.3G82.4G83G83.0G83.1G83.2G83.4 |
| 7 | Consequences of cerebrovascular diseases; - Consequences of subarachnoid hemorrhage - Consequences of intracranial hemorrhage - Consequences of other non-traumatic intracranial hemorrhage - Consequences of cerebral infarction | I 69I 69.0I 69.1I 69.2 I 69.3 |
| 8 | Congenital malformations of the nervous system: - Microcephaly - Congenital hydrocephalus - Congenital anomaly of the corpus callosum - Arynencephaly - Holoprosencephaly - Other reduction deformations of the brain - Septoptic dysplasia - Megalencephaly - Congenital cerebral cysts Spina bifida - Hypoplasia and dysplasia of the spinal cord - Other specified malformations of the spinal cord - Syndrome Arnold-Chiari | Q 02Q 03Q 04.0Q 04.1Q 04.2Q 04.3Q 04.4Q 04.5Q 04.6Q 05Q 06.1Q 06.8Q 07.0 |
| 9 | Other developmental speech and language disorders | F 80.8 |
| 10 | Psychological developmental disorder-Childhood autism-Atypical autism-Rett syndromeAsperger syndrome | F 84.0F 84.1F 84.2F 84.5 |
| 11 | Sensorineural hearing loss bilateral (after cochlear implantation from 1-1.5 months after surgical treatment) | H 90.3 |
| 12 | Down's disease | Q 90 |
| 13 | Diseases of the neuromuscular junction and muscles: - Muscular dystrophy - Myotonic disorders - Drug myopathy | G 71G 71.0G 71.1G 72.0 |
| 14 | -Hydrocephalus-Communicating hydrocephalus-Other brain lesions-Cerebral cyst-Anoxic brain lesion, not elsewhere classified-Other spinal cord diseases | G 91G 91.0G 93G 93.0G 93.1 G 95 |
| 15 | Rarely occurring diseases: - Hereditary ataxia - Congenital non-progressive ataxia - Early cerebellar ataxia - Late cerebellar ataxia - Cerebellar ataxia with DNA repair disorder - Hereditary spastic paraplegia - Other hereditary ataxia - Other degenerative diseases of the basal ganglia - Dystonia - Multiple sclerosis - Other demyelinating diseases of the central nervous system | G 11G 11.0G 11.1G 11.2G 11.3G 11.4G 11.8G 23G 24G 35G 37 |
List of contraindications
to rehabilitation treatment at the NCDR
Frequently recurring or heavy bleeding of various origins, severe anemia with a hemoglobin level of less than 80 g/l; generalized, frequently recurring seizures of various etiologies (with remission for 6 months);
Acute infectious diseases;
Active stage of all forms of tuberculosis (A 15.0–1; A 15.5; A 15.7–9);
Malignant neoplasms (III-IV stages);
Insufficiency of respiratory function more than III degree;
Febrile fever or low-grade fever of unknown origin;
The presence of complex, severe concomitant diseases (including protein-energy malnutrition of the 3rd degree, anemia of the 3rd degree);
Diseases in the stage of decompensation, including uncorrectable metabolic diseases (diabetes mellitus, myxedema, thyrotoxicosis and others).
Purulent skin diseases, contagious skin diseases (scabies, fungal diseases and others), trophic changes (bedsores);
Activity of the rheumatic process of degree 2 or higher, the presence of hormonal therapy;
Ankyloses and persistent irreversible contractures;
Mental illnesses with personality desocialization (F 00; F 02; F 03; F 05; F 10–F 29; F 63; F 65; F 70–F 79);
Vegetative state, apallic syndrome
If there are other concomitant diseases that prevent active participation in the rehabilitation program for 2-3 hours a day.
Note:
— patients in a vegetative state are prescribed palliative care services. In cases where rehabilitation potential arises, patients, in accordance with international criteria, are sent to the stages of medical rehabilitation;
— patients diagnosed with emotional and behavioral disorders with aggression towards themselves and others are sent to psychiatric hospitals (dispensaries).
List of documents required for hospitalization at the NCDR
Parent's passport or ID card, child's birth certificate (original and photocopy)
Power of attorney for the child, notarized (if the caretaker is not a parent)
Referral for hospitalization, planned hospitalization coupon
Detailed extract from the child's development history
Laboratory tests and necessary medical documents for the child:
a) General analysis of urine and blood (period of 10 days);
b) BL swab from the throat and nose (diphtheria), valid from the date of issue of the test result for 10 days;
c) Bacteriological analysis of stool for salmonellosis (only children under 2 years of age), valid from the date of issue of the analysis result for 10 days;
d) Scraping for pinworm eggs/enterobiasis (valid from the date of issue of the analysis result for 10 days).
e) Feces for worm eggs (valid for 10 days from the date the test result is issued);
f) Conclusion of a phthisiatrician for children under 14 years of age. For children over 15 years of age, fluorography/image (copy) of the chest organs with a radiologist’s report or a phthisiatrician’s report;
g) Pediatrician’s conclusion on the absence of contraindications to rehabilitation treatment due to concomitant pathology (acute/chronic, indicating the period, based on the conclusion of specialized specialists and “D” registration);
h) Data on preventive vaccinations (copy);
i) Certificate of epidemiological environment (valid for 3 days);
j) Laboratory tests necessary for parents to care for the child;
k) BL swab from the throat and nose (diphtheria), valid from the date of issue of the test result for 10 days;
l) Bacteriological analysis of stool for salmonellosis (valid from the date of issue of the analysis result for 10 days);
m) Feces for worm eggs (valid for 10 days from the date the test result is issued);
n) Fluorography/image (copy) of the chest organs with a radiologist’s report or a phthisiatrician’s report;
o) Blood for microreaction (period of 10 days);
p) A certificate from a physician stating that there are no contraindications to hospitalization for care for concomitant pathologies.
Note:
Repeated rehabilitation is carried out once a year.
In case of concomitant chronic pathology, it is necessary to carry out
consultations with a specialized specialist, which should indicate the stage of chronic pathology, recommendations and the absence of contraindications for rehabilitation treatment.
If X-rays, CT, MRI, EEG and other studies are available, provide the doctor upon admission.
The child and accompanying person must be provided with shoes and clothing for the season, replaceable non-slip shoes (closed), 4-5 changes of underwear, handkerchiefs, sportswear, a swimsuit for the child, toiletries (soap, toothbrush, toothpaste, shampoo, comb, etc.).
List of documents
for hospitalization of the adult population in a paid day and 24-hour hospital of the NCDR
Patient's identification document (passport or identity card) (original and photocopy);
A detailed extract from the history of the development of all past diseases, special reactions of the body;
Laboratory tests and necessary medical documents for the patient:
a) General blood test;
b) General urine test;
c) Throat and nasal swab for BL (diphtheria);
d) Feces on worm eggs;
e) Fluorography/image (copy) of the chest organs with a radiologist’s report or a phthisiatrician’s report;
f) Blood for microreaction;
g) ECG
h) For patients after a stroke, consultation with a cardiologist.
Note:
If there is a concomitant chronic pathology, it is necessary to consult a specialized specialist, which should indicate the stage of the chronic pathology, recommendations and the absence of contraindications for rehabilitation treatment.
If available, X-rays, CT, MRI images, EEG and other studies should be provided to the doctor upon admission.
The patient should be provided with shoes and clothing for the season, replaceable non-slip shoes (closed), a change of underwear, handkerchiefs, sportswear, swimsuit, toiletries (soap, toothbrush, paste, shampoo, comb, etc.).
Source: //umc.org.kz/?gospitalization=pravila-gospitalizaczii-v-nczdr
Treatment
- Conservative (drug) therapy: Baclofen, Clonazepam, Gabapentin, Levetirace, Carbamazepine. The disadvantage of conservative treatment is that all the necessary drugs have a strong sedative (calming) side effect.
- Botox, or botulinum toxin. A purified form of a neurotoxin produced by Clostridium botulinum, the causative agent of botulism. Injections are made into the affected muscles, causing temporary weakness or paralysis at the injection site, thereby blocking spasms. The effect lasts for several months, then the injections are repeated. Effective in the initial stages, when only small muscles are subject to involuntary contractions. Repeated injections of botulinum toxins are less effective.
- Microvascular decompression. A surgical operation during which a protector is installed through a small incision in the bone. Thus, neurovascular compression is reduced, the vessels are constantly held in a new position away from the facial nerve. The material for the protectors is Teflon. At the moment, this method is optimal in the treatment of primary hemispasm of the facial nerve. In 89-93% of patients after surgery, all manifestations of hemicial spasm disappear.