Patients who call themselves “heart patients” and have symptoms of cardiac neurosis constitute a fairly impressive group among all functional disorders of the nervous system. They often visit doctors, undergo various examinations, and call an ambulance. Such patients willingly try various heart medications on themselves, and the latest innovations found in the virtual space bring considerable income to experts in alternative medicine, and sometimes to simply charlatans. Their suffering is genuine and incomparable.
Why does cardiac neurosis or neurosis in general occur?
In most cases, in the clinic of neuroses of this kind, a pseudoneurotic psychovegetative state called cardiophobia syndrome occurs. This health disorder, which accompanies the symptoms of heart neurosis, is due to many reasons:
- Individual characteristics of the nervous system, which are often characteristic of the asthenic type;
- Neurocirculatory dystonia;
- Arterial hypertension;
- Hormonal changes during certain periods of life (pathological menopause), which often gives three combined symptom complexes:
- autonomic neurosis,
- neuropsychiatric syndrome,
- sexual dysfunction and sexual disorders;
- Negative impact of industrial hazards, environmental factors and alcoholic beverages;
- Chronic infections (otitis media, tonsillitis, etc.).
Meanwhile, the main reason for the formation of cardioneurosis is rightly considered to be a traumatic situation that arises from time to time or is constantly present and, of course, the attitude of the person himself towards it.
When are heartaches directly related to emotions?
Cardioneurosis has a variety of symptoms, but cardialgia and panic attack are the most striking and common manifestations of the disease. They often represent an independent pathology (psychasthenia, neurasthenia, hysteria, obsessive states), which, however, is often attributed simply to character traits, and the patients are not similar to each other.
For example:
- People prone to hysteria are self-centered, mannered, and loud;
- Psychasthenics, on the contrary, are quiet, shy, constantly feeling self-doubt, and therefore cannot solve even simple life problems;
- The most complaints, including cardialgia, are made by neurasthenics. Everything hurts, their sleep is disturbed, their “nerves are shattered,” their appetite is reduced, they are plagued by various autonomic disorders (tachycardia, sweating, decreased ability to work), they are easily excitable, so they often find themselves in the center of a conflict situation.
Signs of obsessive-compulsive neurosis from these groups are most characteristic of psychasthenics, since they are suspicious by nature, they are often tormented by a feeling of their own inferiority, and are visited by unreasonable fears and obsessive thoughts. However, no matter how striking the differences between these psychotypes are, functional disorders of individual organs often arise against their background. Of course, the heart comes to the fore, then the head, gastrointestinal tract, etc. Cardialgia is perhaps the main and most common complaint of patients suffering from neurosis. If the patient primarily focuses on his heart, and other symptoms fade into the background, then it is customary to talk about cardiac neurosis or cardioneurosis. Cardiac neuroses are most common in people with neurasthenia.
Does your heart hurt or just seem so?
Pain in the heart during neuroses can be considered an almost natural phenomenon. Due to the fact that people suffering from neurosis are characterized by pronounced emotional lability, cardialgia in them can be triggered by excitement, expectation, and conflict. In a word, everything is built on emotions, not only negative, but also positive (having learned the good news, a person “grabbed his heart”).
Pain in the heart during neuroses can be fleeting or last for months; sometimes they occur paroxysmally and accompany a panic attack. Thus, the main signs of cardiac neurosis can be considered:
- Dull, stabbing, squeezing pain behind the sternum, in the nipple area, radiating to the neck, shoulder blade, arm, accompanied by shortness of breath, reaching the point of suffocation. Fear, anxiety, fear of death, as a rule, are companions of cardialgia. The ambulance called does not find any signs of heart damage, and the recorded ECG does not register any changes. However, in some cases, neurogenic cardialgia can cause vascular reactions
(cardiovascular neurosis), leading to spasm of the coronary arteries, which, in turn, threatens to impair coronary circulation in patients in the absence of coronary heart disease; - A panic attack that occurs suddenly and manifests itself with excitement incommensurate with ordinary human feelings, which begins “somewhere inside” and quickly covers the entire body. For the patient, this is no longer just fear - it’s horror! A similar condition on the ECG can be recorded as sinus, and sometimes even paroxysmal tachycardia
; - Tachycardia, very characteristic of cardiac neuroses. The frequency and rhythm of heart contractions changes in such patients depending on mood and time of day (waking up is the cause of unexplained tachycardia). The slightest excitement, standing in line (what if I don’t have time?), physical activity can cause a rapid heartbeat. Some patients practically live with tachycardia, since provoking factors are encountered at every step, even if healthy people do not see them;
- Extrasystole, observed in the morning and disappearing if you change the situation or please the person with something;
- Cardiac rhythm disturbances (arrhythmia) , which are more often recorded under strong emotional stress, and patients describe them as stopping and turning over the heart;
- Chills, hot flashes, shortness of breath are symptoms of cardiac neurosis, very reminiscent of a sympathetic-adrenal crisis;
- One of the types of cardiovascular neurosis is vegetative neurosis , often present as one of the symptom complexes in pathological menopause, other hormonal disorders and autonomic disorders ( vegetative-vascular dystonia
).
With pathological menopause, autonomic neurosis is called vegetative-disharmonic cardiodystrophy
. Clinically, the disease is manifested by cardialgia of a pressing and cutting nature, sometimes the pain radiates to the arm and shoulder blade, and the rhythm may become more frequent. Painful sensations do not depend on physical activity, a state of rest does not bring relief, nitroglycerin has no effect; - Symptoms such as sweating, hot flashes, shortness of breath, dizziness, sympathetic or parasympathetic crisis, tachycardia or bradycardia, trembling, flushing or pallor of the skin, indicating some kind of autonomic problem.
- Other manifestations in the form of increased blood pressure, headache, heart pain, which are often classified as signs of vegetative-vascular dystonia of the hypertensive type
, which, in principle, is synonymous with autonomic neurosis.
It is obvious that with such a variety of clinical manifestations that are sometimes present in one patient, prescribing something to him that will immediately solve all the problems is not an easy task. Patients often go to the doctors, each time presenting new complaints, but rarely follow through, because they want everything at once, and the treatment of cardiac neurosis requires not only the prescription of medications from various groups, but also consultations with other specialists.
Treatment of cardiac neurosis is not an easy task
Before prescribing drugs for the treatment of cardiosclerosis, it is necessary to find out why, for what reason it arose, in order to try, if not eliminate it, then at least reduce the negative impact, that is, one should obey the generally accepted law: treat the cause.
Treatment of cardiac neuroses is fraught with difficulties caused by the patient’s misconceptions about his illness. The word “psycho” simply causes an inadequate reaction in some patients; they refuse to visit a psychotherapist, and the word “neurosis” is perceived as a severe mental disorder that needs to be hidden from strangers. To explain the meaning of the term, to persuade a person to visit other specialists and begin treatment, the doctor may need a lot of patience. True, some patients “recover before our eyes” after a conversation conducted by a skillful and understanding doctor.
It is difficult to name a specific group of drugs for the treatment of cardioneurosis, but most of all they are sought by the patients themselves, since “it takes nothing.” Treatment depends on the symptoms, but the first steps in the fight against this disease are aimed at eliminating anxiety, discomfort, and psychological discomfort:
- A calming, encouraging, encouraging conversation is held. Listening patiently and giving the opportunity to speak out is best done by a psychotherapist, because he is specially taught this;
- Recommendations are given in terms of streamlining the daily routine, work, nutrition and rest and normalizing relationships in the family and at work;
- Drug therapy is prescribed in accordance with the patient’s complaints and well-being, but it begins with light sedatives of herbal origin (this is where there is room for traditional medicine!) and treatment of the cause.
Some specialized psychoneurological clinics (regional and republican subordination) have neurosis departments, where people with various variants of this disease are periodically treated. Most often, patients are brought to such departments by panic attacks, which are often combined with migraines or other pathologies that debilitate the patient.
To relieve attacks of neurosis, the patient is prescribed:
- Mild antidepressants (amitriptyline, Grandaxin, azafen, imizin, nialamide);
- β-blockers in the presence of tachycardia, borderline arterial hypertension (anaprilin, trazikor);
- Light sleeping pills such as zopiclone in case of sleep disturbances, but not for more than 3 weeks, since such drugs are addictive;
- Physiotherapeutic procedures (electric sleep, “comb”, electrophoresis, pine and pearl baths - for increased excitability, Charcot's shower, circular shower - in case of hyposthenic symptoms);
- The patient is taught autogenic training and mental relaxation (breathing exercises).
Patients with any form of neurosis (as it turns out, these are one disease with different names) benefit greatly from sanatorium-resort treatment in neurosomatic institutions. Sometimes, a change of environment, a change in the regime in the right direction, new positive emotions, balneological treatment turn out to be very useful and free the patient from the use of medications for a long time. Such people know: a sanatorium is the best medicine for them.
Video: vegetative-vascular dystonia and its cardiac manifestations
Step 1: pay for the consultation using the form → Step 2: after payment, ask your question in the form below ↓ Step 3: You can additionally thank the specialist with another payment for an arbitrary amount ↑
If there is sudden pain between the ribs that gets worse with movement, a possible cause of discomfort is a pinched nerve in the thoracic region. Symptoms of pinching largely repeat the symptoms of intercostal neuralgia.
Causes
When your back or neck hurts, many people think about a pinched nerve. And often this is exactly the case. But we must not forget about other reasons when other diseases are hidden behind neuralgia. Typically, nerve roots in the cervical or thoracic spine are pinched due to the following conditions:
- Osteochondrosis.
- Deformations: scoliosis, kyphosis, lordosis.
- Intervertebral hernia.
- Spondyloarthritis.
- Tumor processes.
- Injuries.
- Increased physical activity.
- Psycho-emotional stress.
In damage to the nerve roots, a mainly mechanical factor plays a role: compression by vertebrae, spasmed muscles or space-occupying formations. Here we are not talking about the inflammatory process, although to some extent it is also present.
To understand the origin of neuralgia, it is necessary to establish the most important factors in its development in a particular person.
Features of the cervical spine
Despite the importance of the cervical spine, the cervical vertebrae cannot afford to be as massive and inactive, since the neck is the most mobile part of the spine.
It is between such compromises, between grace, mobility and the performance of an important supporting function, that the seven cervical vertebrae exist. Their excessive mobility quite often leads to pinched nerves in the cervical spine.
In fact, symptoms often indicate not a pinched nerve in the cervical spine, but a pathology of the roots. After all, nerve roots emerge from the spine, the anterior branches of which form the cervical plexus. Pinching of a separate nerve in the cervical spine can also occur, but this is less common than radicular symptoms. What symptoms arise and what nerves are affected?
Symptoms
A pinched nerve leads to the formation of so-called radiculopathy – a non-inflammatory radicular lesion. The symptoms of the disease are quite diverse and are determined by damage to nerve fibers of different functions: motor, sensory and autonomic. They all come as part of one root, extending from the spinal cord. The localization of pathological changes will depend on in which part the pinched root is located: in the cervical or thoracic.
The most common complaints when visiting a doctor are:
Cough and shortness of breath.
In the early stages, the disease occurs with symptoms of irritation of nerve fibers, when sensitivity and reflex processes increase. As the pathology progresses, there is a loss of sensory and motor functions up to paresis and paralysis.
When the cervical spine is affected, the symptoms will spread to the head, and if the thoracic root is pinched, dysfunction of the heart, bronchi or diaphragm can be noticed. Therefore, the disease must be differentiated from the pathology of these organs.
The clinical picture of a pinched nerve in the thoracic or cervical spine has pronounced symptoms. Their identification will make it possible to make a preliminary diagnosis.
Medicine of the world
12/25/2019 admin Comments No comments
The cervical spine is unique in many ways. Firstly, damage to the spinal cord in this section, at the level of the cervical enlargement, is the most serious, since the entire torso, arms and legs are paralyzed. Therefore, the vertebrae of this department must reliably protect the underlying structures of the central nervous system - the spinal cord. In addition, this department is entrusted with the function of carrying the head, which is quite heavy.
Diagnostics
To clarify the diagnosis of neuralgia, it is necessary to undergo additional examination and consult with related specialists. A neurologist and a traumatologist will help the general practitioner with this. And the complex of instrumental methods includes:
- Radiography.
- CT scan.
- Magnetic resonance imaging.
- Electromyography.
- ECG.
The need for certain medications is determined by the clinical situation. Some of them are needed to exclude other diseases that have similar symptoms.
Treatment
To cure a pinched nerve in the thoracic region, you must first eliminate the cause of the disease. This will be possible with an integrated approach to therapy. Treatment of neuralgia should be determined by the degree of its development, the characteristics of the patient’s body and concomitant diseases. In this case, conservative and surgical techniques are used.
The central link of conservative treatment is the use of medications. They allow you to relieve acute manifestations of the disease and influence the etiological factors of the pathology. Most often, complex treatment includes the following groups of drugs:
- Painkillers and anti-inflammatory.
- Muscle relaxants.
- B vitamins.
- Improving microcirculation.
- Chondroprotectors.
After the acute effects have subsided, you can use drugs in the form of an ointment, gel or patch. They have a local effect without systemic side effects.
Treatment of neuralgia with medications should be carried out according to the doctor’s recommendations.
Physiotherapy can improve the condition of the nerve, its blood supply, eliminate muscle spasms and reduce symptoms. They have a good effect in combination with medications. As a rule, the following methods are recommended:
- Electrophoresis of drugs.
- Magnetotherapy.
- Laser treatment.
- UHF therapy.
- Balneotherapy.
An experienced physiotherapist will advise which procedures are best for a particular patient.
To strengthen the spine, improve its function, relieve muscle tension and increase the overall fitness of the body, you need to pay attention to therapeutic exercises. Movement is the basis of therapy for most skeletal pathologies, and this case is no exception. Various exercises are used to strengthen the muscular corset and reduce compression of the vertebrae.
The gymnastics complex is selected by the doctor individually. At first, the exercises are performed under the supervision of an instructor, and as you learn, you can practice at home. Pain syndrome should not be allowed to appear - it indicates incorrect performance of gymnastics.
Movements are made smoothly, without jerking. You need to master the exercises gradually and regularly. This is the only way to achieve a good effect.
When conservative treatment does not bring the expected result or there are causes that cannot be eliminated by other methods, surgical intervention is used. Most often this is necessary for injuries, tumors, intervertebral hernias, severe osteochondrosis or persistent spinal deformities. Depending on the situation, the following techniques can be used:
- Discectomy is the removal of a protruding section of an intervertebral disc.
- Laminectomy – removal of a vertebral arch.
- Spondylodesis – stabilization of the vertebrae.
- Tumor resection.
It is necessary to take a responsible approach to pinched nerve roots. To get rid of symptoms, it is not enough to suppress them, you need to eliminate the cause of the compression.
The human spine performs not only a musculoskeletal, but also a protective function. Each segment contains a pair of nerve processes that are responsible for the functioning of one or more organs. A pinched nerve is a complication that can occur with osteochondrosis. It is accompanied by unbearable pain, and also leads to disruption of the functioning of certain organs. This condition requires immediate treatment. Let's consider the types of pinching, the reasons for their occurrence, and methods of treatment.
First aid
Pinching of the thoracic nerve occurs suddenly. Sharp pain appears very quickly. In this case, you need to lie on a hard surface in a position in which the least pain is felt.
The patient must take an analgesic to relieve pain. Since trouble can occur suddenly and cause a feeling of fear for one's own life due to symptoms similar to a heart attack, the patient can be asked to take a sedative.
With severe pinching, excruciating pain is observed, which cannot be tolerated, since it is harmful to the health of the nervous system as a whole. The most correct action in such a situation would be to call emergency help at home.
Upon arrival, the doctor must be informed of all medications taken before the ambulance arrived.
Types of pinching
According to the place of occurrence, pinching in osteochondrosis is divided into the following types:
- cervical;
- in the thoracic region;
- in the lumbosacral region.
Most often, symptoms manifest as pain, but sometimes the patient may experience loss of sensitivity or numbness in the affected area. It all depends on which nerve is being compressed:
- sensitive;
- motor;
- vegetative.
The main sign of a pinched sensory nerve is acute pain. Then the person immediately seeks help from a doctor. Damage to the autonomic and motor nerves does not always have pronounced symptoms, as a result of which the patient ignores the pathology for a long time, which is fraught with serious complications.
In what cases can exercises help with thoracic osteochondrosis?
It is important to know! Doctors are shocked: “An effective and affordable remedy for joint pain exists. " Read more.
Neurologists and vertebrologists refer patients with thoracic osteochondrosis to a physical therapy doctor immediately after eliminating severe pain. The stage of the pathology does not matter. But it must be taken into account by the physical therapy doctor when compiling a set of exercises. The more pronounced the damage to the intervertebral discs and vertebrae, the more carefully the physical activity is dosed.
Diagnostics
To establish an accurate diagnosis, you should contact a neurologist. He will conduct an initial examination and also ask in detail about the signs of the disease:
- how long ago the pain began;
- the nature of the discomfort;
- localization.
MRI fully reveals the development of osteochondrosis at any stage of development. The tomograph reveals even minimal changes in the structure of the spine.
To clarify the data, the doctor will refer the patient to the following hardware tests:
- Magnetic resonance imaging (MRI). The images clearly show soft tissues, including the spinal cord and nerve endings. This type of diagnosis helps to determine the exact cause of compression, including intervertebral disc herniation and protrusion.
- Electromyography (EMG). Determines the degree of functioning of nerves and muscles.
Based on the results of the studies, an accurate diagnosis is established and the most effective treatment is prescribed.
Pathogenesis
A pinched thoracic nerve is not the most common disease. This is due to the fact that the thoracic spine does not experience as much stress as other parts. But he is also susceptible to pathological processes. The spinal cord has nerve branches that run between the vertebrae of the chest. Inflammation or displacement of cartilage discs, adjacent muscles, damage or deformation of the vertebrae can lead to pinching of the roots of autonomic, motor or sensory nerve fibers. Blood circulation in the affected area becomes difficult and tissue swelling occurs. As a result, nerve cells are damaged, causing pain.
The nature and intensity of pain may vary. Gradual compression of nerve fibers is usually accompanied by a dull aching, and in the acute stage of nerve entrapment, sharp and acute pain. It can be mistaken for a heart attack, or an attack of intercostal neuralgia. Unpleasant sensations occur not only in the sternum, but also in the ribs. Symptoms of strangulation are also often confused with manifestations of diseases such as gastritis or stomach ulcers.
Symptoms
Signs of pathology depend on the following factors:
- type of pinching;
- presence/absence of inflammation;
- degree of nerve compression;
- reasons for appearance.
There are 8 nerves in this section. Pinching any of them provokes discomfort, tingling or numbness in the affected area. Depending on which nerve is being compressed, the following symptoms are observed:
- Compression of the nerve located in the C5 vertebra leads to pain in the shoulder area, muscle weakness and numbness in the shoulder area.
- When the C6 vertebra is injured, pain and numbness are observed along the entire arm, especially in the wrist and thumb area.
- Pinching of the C7 vertebra is accompanied by painful sensations along the upper limb to the middle finger, and sometimes there is a loss of sensitivity in the hand and tingling.
- If the C8 vertebra is pinched, the patient feels a significant limitation in the motor function of the arm.
Important! A pinched nerve in the cervical spine with osteochondrosis leads to a deterioration in local blood circulation. A person may complain of tinnitus, frequent headaches, deterioration of hearing, vision, and memory.
Pinched nerves in this area are quite rare due to the insignificant mobility of the chest area. Usually the sensory or autonomic nerve is compressed.
Pinching in the thoracic region is quite rare. More often, the cervical and lumbar regions are susceptible to destructive changes.
The pathology is accompanied by acute pain in the left side of the chest and has a tingling, pulsating character. Such sensations can be confused with heart pain - when you try to take a deep breath, the discomfort intensifies, and a heartbeat may be disrupted. Then there is a feeling of tightness in the chest, which increases with movement. The pain gradually spreads along the ribs.
With severe pinching, a person may feel unpleasant discomfort in the stomach area. They are similar to the symptoms of ulcers, gastroenteritis, and colitis. You can distinguish nerve compression from gastric diseases with the help of antispasmodics: if you have problems with the digestive system, taking them makes you feel better, but if you have neuralgia, such drugs are useless.
Important! When a nerve is pinched in the thoracic region, pain is not constantly felt. It can bother you periodically, changing its character and duration. Most often, an attack occurs during sleep at the moment of complete muscle relaxation.
With osteochondrosis of the lumbar region, the sciatic nerve is affected, which is accompanied by inflammation. Painful sensations have varying degrees of severity - from mild to acute attack. There may be a burning sensation. In some cases, discomfort spreads from the lumbar area to the fingers of the lower extremities.
Neuralgia without pain manifests itself in the form of numbness, loss of sensitivity in the toes and calf muscles, as a result of which the gait changes - a person may limp on one leg.
The severity of symptoms when a nerve is pinched in the lumbar region depends on the presence/absence of a hernia, the size of the protrusion, and radiculitis.
Note! People who are overweight are more susceptible to compression of the sciatic nerve due to osteochondrosis, since the lumbosacral region bears the maximum load.
A set of exercises for osteochondrosis of the thoracic region
The first classes do not last longer than 15-20 minutes. The back muscles must adapt to the loads that arise, so first you need to perform the simplest exercises. If there is no discomfort and increased mobility of the thoracic region, you can increase the training time to 30-40 minutes. And the exercise therapy doctor will include complex exercises in the treatment complex, but also more effective for osteochondrosis.
Patients with thoracic osteochondrosis will need a chair, not a stool. When performing some exercises, you need to focus on its back:
- sit in such a way that your shoulders and upper back are pressed tightly against the back of the chair. Try to bend back, arching your lower back, and then slightly lean forward;
- sit up straight, put your hands on your shoulders. Try to lift them, resisting with your palms.
The number of approaches is from 5 to 10. Such exercises are often used for combined cervicothoracic osteochondrosis.
Even “advanced” joint problems can be cured at home! Just remember to apply this once a day.
For thoracic osteochondrosis of 2-3 degrees of severity, you will need a small pillow for exercise, which should be placed slightly above the lower back. What exercises are most effective:
- Bend your legs at the knees, rest your feet on the floor. Raise your shoulders, trying to keep your neck motionless;
- straighten your legs, spread your arms to the side. Raise one hand, place it behind the chest, trying to bring it as close as possible to the floor surface;
- straighten your legs, place your arms arbitrarily and, without using them, try to roll over first on one side, then on the other.
Repeat the exercises 10-15 times. As your muscles strengthen, you should stop using the pillow.
It is convenient to do therapeutic exercises in a standing position on all fours on a thick gymnastics mat. For thoracic osteochondrosis, the following exercises are usually included in the complex:
- round your back, lowering your chin, and then bend it, raising your head up;
- sit down without lifting your hands from the floor, stretch your lower back, and take the starting position of your body. Then straighten your legs, focusing on your hands, and bend well again.
Perform exercises 7-10 times. Hold in the position of maximum tension of the back muscles for 10-20 seconds.
Paired gymnastic exercises are convenient to perform during training sessions conducted by a physical therapy doctor. At home, you should use the help of a family member. What exercises are most useful for damage to the thoracic discs and vertebrae:
- sit down, spread your legs wide, rest your feet on the ground. Hold hands, bend forward and backward in turn;
- press your backs together, grab with your elbows. Perform shallow bends without straining your back muscles too much;
- stand with your backs to each other. Pass an object, such as a ball, first from the right and then from the left.
Repeat exercises 10 times. The effect of training is greater if the partner is approximately the same height and weight.
After completing the main complex, you must definitely do stretching exercises to strengthen, increase muscle elasticity, and adapt to subsequent loads:
- sit on a chair, or better yet, on a stool, wrap your arms around your chest, as if hugging yourself. Try to continue placing your hands behind your back;
- stand up, press your legs together, bend over, trying to touch your forehead to your knees;
- lie down, bend one leg and cross it behind the other, trying to touch the floor with your knee. Repeat the exercise in the opposite direction.
The number of approaches is arbitrary. When performing stretches, only pleasant sensations usually arise, so you can repeat them up to 20 times.
Patients with thoracic osteochondrosis often breathe shallowly, which reduces the mobility of the costovertebral and sternocostal joints. The following exercises will help increase the volume of air when inhaling:
- sit up straight and wrap a narrow towel or scarf around your lower chest. While stretching the fabric with your hands, take deep breaths. At the maximum point of tension, hold your breath for 5 seconds;
- sit down, raise your hands, clasping your fingers. Inhale deeply to tighten your abdominal muscles. As you exhale, bend first to one side, then to the other. Inhale again and stretch upward.
At the initial stage of training, you need to do the exercises about 5 times due to the high likelihood of dizziness. Gradually the number of approaches should be increased to 10-15.
During a relapse of thoracic osteochondrosis, acute pain occurs in the area of damaged discs. Any sudden, awkward movement can intensify it. Therefore, doctors often do not recommend exercising during the acute period. If the pain is moderate, then the following exercises are allowed:
- Lie on your stomach, stretch your arms to the side. Take a deep breath, slightly raise your head and arms. Stay in this position for 5 seconds, exhale, take the starting position;
- turn on your back, put your hands behind your head, stretch, straining the muscles of your back, neck, and shoulder girdle;
- lie on your stomach, stretch your arms along your body, relax. Try to bring your shoulder blades together only by tensing your muscles, and not by moving your arms or shoulders.
If osteochondrosis worsens, you can repeat the exercises no more than 5 times. In this case, movements should be smooth, slightly slow, without jerking.
Causes
Osteochondrosis is pathological changes in the intervertebral discs, that is, their gradual destruction. During the process of such degenerative transformations, the discs sag and the distance between the vertebrae decreases. Pinched nerve processes can occur for the following reasons:
- Exacerbation of osteochondrosis with hypertonicity of muscle tissue. The nerve roots are compressed by the vertebrae.
- Muscle spasm. Blood vessels are pinched, the blood supply to vital organs and systems, and the brain is disrupted. Prolonged compression of nerve endings causes tissue death and improved sensitivity.
- Hernia or protrusion. The nerve processes are compressed by the intervertebral disc.
- Displacement or subluxation of the vertebrae.
Long-term pinching of a nerve root can cause loss of sensitivity of the skin in the neck area.
Factors that increase the risk of pinched nerves in osteochondrosis are:
- spinal injury as a result of a fall or blow, leading to subluxation or displacement of discs;
- infectious diseases of the genitourinary system of a chronic nature, including sexually transmitted diseases;
- blood clots, neoplasms, abscess - provoke a reduction in the distance between the vertebrae;
- diseases associated with metabolic disorders;
- excess weight, obesity - provokes excessive stress on the spine;
- poor posture - causes uneven distribution of the load on the spine;
- pregnancy, especially in the later stages - the fetus gradually increases in size and begins to put pressure on the spine;
- hypothermia of the body;
- prolonged exposure to stress;
- excessive physical activity, especially sudden movements.
Treatment
The selection of a specific treatment regimen directly depends on the cause, location, and severity of symptoms of pinching:
- If the nerve is pinched due to subluxation, then massage and manual therapy will have a good therapeutic effect. They will help reduce pain, the patient will feel relief after the first session.
- Protrusion requires long-term complex therapy, which involves restoring the anatomically correct position of the discs.
- If there are growths or an abscess, it is necessary to eliminate them.
Important! If a hernia is present, surgery may be required.
One of the main goals of therapy for a pinched nerve is to relieve pain for the patient. For this, the following drugs are prescribed:
- Non-steroidal anti-inflammatory drugs. They relieve inflammation and relieve pain. These medications include: Ibuprofen, Ibufen, Diclofenac, Movalis.
- Strong analgesics. They are used only in extreme cases under the supervision of the attending physician, so that drug addiction does not develop. These drugs include: Ketanov, Spazmalgon.
- Muscle relaxants. The mechanism of their action is to reduce spasm and relax muscle fibers. As a result of this, the nerve roots are released and pain is eliminated. Muscle relaxants are prescribed for a short period, since they adversely affect other organs and systems. The most common drugs in this group are: Sirdalud, Mydocalm, Tizanidine, Methocarbamol, Baclofen.
- Corticosteroids. They are used in extremely rare cases when other therapeutic methods do not produce results.
Used only with a doctor's prescription. It has serious pharmacological effects.
Manual therapy is aimed at achieving the following goals:
- restoration of proper transmission of nerve impulses;
- elimination of muscle spasm;
- increasing the distance between the vertebrae;
- improving blood circulation at the local level.
REFERENCE. With the help of manual therapy, you can not only relieve pain, but also achieve final restoration of the affected nerve.
Physiotherapeutic procedures are aimed at strengthening muscle tissue, thereby reducing the load on the pinched nerve. In addition, they contribute to:
- warming up the affected area, resulting in a decrease in pain;
- eliminating swelling;
- improving local blood circulation.
To treat a compressed nerve due to osteochondrosis, the following physiotherapy procedures are used:
- paraffin applications;
- magnetic therapy;
- electrophoresis;
- phonophoresis.
Manual therapy will help relieve the pinched nerve and you will be able to move freely within a few days of visiting the doctor's office. It is worth remembering that this is a temporary measure and complex treatment is necessary.
Massage procedures help improve blood circulation and metabolic processes at the local level, and increase the mobility of the damaged spine. The effectiveness of the massage increases if the patient performs special exercises immediately after it. As a result of the complex effect, the back muscles will be strengthened and the load on the spine will be reduced.
Important! Massage and exercise therapy for pinched nerves should be performed on a regular basis.
Surgical intervention is required only in extreme cases when the patient's condition is critical:
- Loss of control over urination and bowel movements.
- Cauda equina syndrome. The cauda equina is a nerve ending located in the lower part of the spinal cord. If they are severely pinched, the patient experiences unbearable pain, serious neurological disorders and problems with the pelvic organs appear. Cauda equina syndrome is an indication for urgent surgery.
During the operation, the cause of pain is first eliminated, after which the spinal column is stabilized.
Video about pinched nerves in cervical osteochondrosis
Osteochondrosis, which is practically untreatable, can cause serious health problems. To avoid pinched nerves, it is necessary to correctly distribute the load on the spine, lead an active lifestyle, eat right, and also regularly visit a neurologist for preventive purposes.
- 04/14/2019 Exercise therapy for cervical osteochondrosis
- 04/14/2019Injections for cervical osteochondrosis
- 04/06/2019 Tinnitus with cervical osteochondrosis
- 04/06/2019 Fear and depression in cervical osteochondrosis
The phrenic nerve (N. phrenicus) is a mixed innervating trunk that is part of the cervical plexus. Here both the spinal roots and the tissues coming from the cervical nodes located in the lower part come together. If dysfunction occurs in the phrenic nerve for any reason, you need to know how to diagnose it in yourself, which specialist to contact and what treatment methods to use to relieve spasticity or eliminate more severe pathologies.
You can make an appointment with a doctor in the “Doctors and appointments” section.
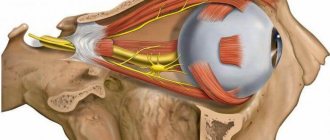
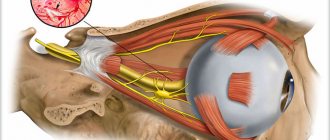
Anatomy of the phrenic nerves
The phrenic nerve is a mixture of spinal branches as well as cervical ganglion structures. They are all intertwined together and form part of the cervical plexus. If we talk about its localization, then it passes in the neck along the anterior surface, in the chest, and phrenic-abdominal branches are formed in the abdominal cavity.
To understand how the phrenic nerve functions, you need to understand what its anatomy is.
First of all, you need to understand that it is paired and is divided into right and left. But both of them depart from the area where the 3rd, 4th and 5th roots of the cervical spine are localized. Then they go down along the spinal cord. The center of the phrenic nerve is located in the anterior part of the cervical spine.
They then pass from the first scalene muscle along the subclavian artery with its further intersection.
When considering the phrenic nerve, it is necessary to take into account its topography in the neck:
- The left process, reaching the chest, crosses the carotid artery, respectively the left subclavian, aorta, and intercostal vein. After this it passes through the pericardium.
- The right one is also located in the chest and runs directly parallel to the brachiocephalic vein. It goes around the right atrium, and before that the superior and inferior vena cava. But, with all this, it should be noted that in some people the position of the right phrenic nerve may be slightly different. In some cases it passes directly through the diaphragmatic opening. In another embodiment, its lateral direction relative to the diaphragm is allowed. It is also worth noting that along the right side of this phrenic nerve the mediastinal pleura runs along its entire length.
If the heart is compressed
This effect on the muscles of the organ is caused by a lack of oxygen. This phenomenon is characteristic of all forms of cardiac ischemia. If the pain is in the area of the heart and radiates to the left side of the body, it means that the person has angina pectoris. Most often it occurs during unusual physical activity and goes away after a double dose of nitroglycerin.
In addition to angina, squeezing pain in the heart can signal the following diseases:
- ventricular fibrillation;
- regular extrasystoles;
- atrial fibrillation;
- intracardiac blockades;
Blockade of pathways
Important! The squeezing pain may occur early in the morning or during rest.
Functions of the phrenic nerves
After it becomes clear what the phrenic nerve is and what its topography is, you should study what functions it performs in the human body:
- Realizes the function of innervation in the occipital region, or more precisely, the epidermis in this area and is partially responsible for the concha.
- It also provides a level of sensitivity in the outer ear along the osteochondral canal.
- Responsible for the area of functioning of the subclavian and supraclavicular parts.
- Controls the level of sensitivity in the area of the shoulder blades.
- In the abdomen and diaphragm, it is responsible for the innervation of the peritoneum and diaphragm, pericardial and pleural tissue.
Symptoms
When, for some reason, an irritant occurs in this part of the body, the phrenic nerve exhibits symptoms such as:
- The pain is similar to angina pectoris due to the fact that it is localized in the left side of the thoracic region.
- Pain may radiate to the neck area. Because of this symptom, this condition is similar to osteochondrosis.
- Most often, discomfort occurs when a person makes sudden breathing movements, sneezes or coughs. This condition can also worsen during sudden bends or turns.
- If neuralgia occurs on the right side, then, most often, the symptoms resemble liver problems, in particular colic. In some cases, a condition of hiccups may occur.
Naturally, how much the phrenic nerve innervates and how severe the pain is depends on what disease or disorder provoked this condition.
Another point that needs to be paid close attention to is the similarity of symptoms with other pathological conditions of the human body. Therefore, before determining why the pain occurs and applying this or that treatment, it is necessary to undergo a comprehensive examination, and the specialist must make a final verdict on what is bothering his patient.
Contraindications for implementation
Acute, piercing pain in the back, radiating to the hips and shoulder blades, is an absolute contraindication for exercising. You should not perform exercises in the following pathological conditions:
- tachycardia, bradycardia;
- severe dizziness, loss of coordination of movements;
- high or low blood pressure;
- respiratory, intestinal infections;
- elevated body temperature.
Training should be postponed in case of exacerbation of other chronic diseases. If you have recently undergone surgery, then performing exercises is strictly prohibited.
Causes
Irritation of the phrenic nerve can occur for a number of reasons:
- Severe intoxication of the body.
- Various infections.
- Concomitant diseases of the spinal column, including spondyloarthrosis and spondylosis.
- Cardiovascular diseases.
- Hypertension.
- Pachymeningitis.
- Tumors in the cervical or thoracic spine.
But, there is a whole group of reasons that lead to pain and inflammation of the left and/or right phrenic nerve.
In some cases, when a person places too intense stress on the muscular system, paresis of the phrenic nerve may occur due to intense spasm of the muscle fibers. A kind of pinching occurs, which, with prolonged exposure, can cause inflammation of the nerve fibers.
Due to the development of a hiatal hernia, an increase in these structures is formed. As a result, the phrenic nerve may be affected.
But it is worth noting that this situation occurs quite rarely and is most often associated with birth defects in the development of this part of the human body. The xiphoid process appears on the diaphragm. Although, defects in the structure may be present in the stomach and colon in the anterior or posterior mediastinum. In this case, the phrenic nerve may also be most negatively affected.
With this process of the disease, the patient complains of reflex angina, which occurs due to the fact that the vagus nerve is irritated. Coronary spasm may also occur.
The sufferer may experience a condition where the stomach protrudes above the diaphragm.
When paralysis occurs, the diaphragm is characterized by a high state. At the same time, when you inhale, it does not bulge as it should. And the epigastric region does not descend to the liver. When a person begins to worry or during intense physical work and stress, he or she experiences shortness of breath. During the act of defecation, tension is released. If a person experiences a full stage of paralysis, then the minimal symptoms can become more severe, even leading to fatal asphyxia.
When a state of irritation of these nerve fibers is formed, a person experiences pain of varying intensity, which affects not only the directly affected area, but also radiates to the area of the shoulder girdle, part of the neck and to the area of the shoulder joint. Hiccups may also develop.
Symptoms of damage to the plexus and individual nerves
The cervical (cervical) plexus itself is quite well protected, so signs of damage to the plexus are practically non-existent. The nerves of the cervical plexus cause the muscles of the neck to work, for example, the sternocleidomastoid, as well as the deep muscles. Similarly, a pinched nerve in the cervical spine in an adult or child can cause disruption of the diaphragm and scalene muscles. What are the symptoms of these motor lesions in this region?
- impairment of flexion, extension, tilt and rotation of the neck due to muscle weakness;
- weakening of the rise of the chest, weakening of inspiration;
- impaired movement of the diaphragm, or hiccups due to excessive irritation of the phrenic nerve.
It must be said that much more often there are signs of pinched nerves in the cervical spine, which are associated with pain syndromes, as well as in connection with impaired sensitivity.
Sensory disorders
When the cervical plexus is damaged, sensitivity disorders of various types (paresthesia, numbness, crawling sensation) occur:
- in the area behind the ear and on the back of the head;
- on the skin of the auricle;
- in the area of the shoulder girdle and in the area of the shoulder joint;
- in the supraclavicular and subclavian region to the first intercostal space.
Thus, if a decrease in sensitivity occurs in these areas, then you also need to pay attention to possible problems with the cervical plexus.
In addition, you need to consider the symptoms associated with cervical osteochondrosis (when a pinched nerve and root occurs due to protrusion or disc herniation), this process is called vertebrogenic nerve damage.
Diagnostics
In order for a specialist to clearly determine whether there is pinching of the phrenic nerve or inflammation, it is necessary to conduct a comprehensive examination. But, before conducting hardware diagnostics, the doctor will perform a complete external examination.
He will palpate the painful areas to see how severe the symptoms are. This is done by ordinary pressure on the muscle parts adjacent to the nerve fibers. And only after he makes a preliminary diagnosis of neuropathy or neuralgia of the phrenic nerve, will he prescribe various types of hardware diagnostics to clarify the condition.
Necessities include:
- X-ray image.
- Carrying out ultrasound examination.
- Carrying out an ECG to make sure that the problem is in the nerve fibers and not in the pathology of the cardiovascular system.
- Magnetic resonance therapy, which allows you to clearly localize where the pathological process is located in the body.
- CT scan.
- Myelography.