Find out more about diseases starting with the letter “G”: Ganglioneuritis, Ganglioneuroblastoma, Ganglionitis of the pterygopalatine ganglion, Soft tissue hematoma, Hematomyelia, Hemiballism, Hemorrhagic stroke, Ganglioneuroma, Hemangioblastoma, Hemifacial spasm, Generalized epilepsy, Germinoma of the brain, Hydrocephalus, Hyperventilation syndrome, Hypercine PS, Hypersomnia, Hypertensive cerebral crisis, Hypertensive encephalopathy, Hypnic headache, Brain glioma
Hemangioblastoma or hemangioma is a benign neoplasm that is localized in the central nervous system, mainly in the body of the cerebellum and has its origin from the blood vessels of the main parts of the brain.
Magnetic resonance imaging (MRI) and histological examination are the main methods for diagnosing hemangioblastoma, because the clinical signs of the disease are very diverse. Manifestations of the tumor depend on its location and occur in the form of dizziness, headache, asthenia, nausea, motor and sensory disturbances, cerebellar syndrome and disruption of the activity of the cranial nerves and pelvic organs. Complete tumor resection is considered the most effective and preferred treatment option.
general information
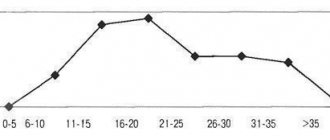
Among all brain tumors, hemangioblastoma accounts for about 2%. Mostly, the incidence of this type of tumor develops in patients in the age group of 40-60 years. Hemagangioblastoma can be inherited due to phakomatosis (Hippel-Landau disease).
Phakomatosis throughout the patient’s life entails the formation of new tumors in the body - pheochromocytoma, retinal angioma, pancreatic cysts and others. With such signs, a conclusion about hemangioma is made in a person aged 20-30 years.
General information about the disease
Hemangioblastoma is formed from blood vessels located in the brain. Although the primary location is the cerebellar tissue, hemangioblastoma can also arise in the brain stem or spinal cord. This tumor is characterized by the presence of cystic and solid components.
About one tenth of cases of hemangioblastoma are a feature of hereditary Hippel-Lindau anomaly or phakomatosis. In this case, the rapid development of multiple intraorganic tumors (pancreatic cysts, pheochromocytoma, renal cell carcinoma, retinal angioma, etc.) is characteristic and in this form the disease is typical for 20-30 year old patients.
Etiology of the disease
If hemangioblastoma develops in conditions of Hippel-Landau disease, then we should talk about genetic inheritance of its occurrence. It is the result of a genetic mutation on the third chromosome and a defect in the production of tumor growth inhibitors. This mutation is transmitted as an autosomal dominant trait.
When it comes to other carcinogenic factors for the occurrence of hemangioblastoma, they are the same as for other tumors of the central nervous system. This is, first of all, the influence of radioactive radiation, as well as excessive exposure to the sun and tanning, exposure to harmful substances at work (benzene, petroleum and coal tars, asbestos, phenol-pharmamaldehyde, vinyl chloride), various oncogenic viruses (herpes, adenovirus, retrovirus) .
Classification of the disease
In neurology, there are 3 categories of disease based on a visual macroscopic assessment of the structure of the tumor:
- Solid hemangioblastoma is a nodule of soft tissue of tumor cells, which is enclosed in a capsule and, when cut, has a soft, spongy consistency of a dark cherry color. This type of hemangiomas accounts for 65% of all hemanglioblastomas.
- Cystic hemangioblastoma is a cystic formation consisting of smooth cells and with liquid, yellowish, transparent contents, on the wall of which there is a small nodule.
- In addition to these, there are also mixed hemangioblastomas. A solid node is visualized in the formation, which contains numerous cysts. The detection rate of such tumors is about 4-5%.
Based on their cellular structure, hemangioblastomas are divided into juvenile, transitional and pure cell. Juvenile hemangioma is a plexus of particularly thin-walled capillaries.
Transitional - has in its structure an equal number of thin-walled stretched capillaries and stromal cells, some of which are filled with fatty contents.
Pure cell hemangioblastoma in its structure contains pathologically altered vessels with numerous yellowish (xanthochromic) cells.
Clinical symptoms
The manifestations of hemangioma are directly determined by its location. Its location in the cerebral hemispheres is extremely rare. Spinal cord hemangioma is diagnosed in 3-13% of patients, medulla oblongata - in 2-3% of patients.
Damage to the cerebellum is expressed in cerebral, cerebellar and distant symptoms. The clinical picture of cerebral symptoms occurs due to the pathological outflow of cerebrospinal fluid and its progressive and excessive concentration in the ventricles of the brain.
Headache with this pathology is not relieved by antispasmodics and painkillers; it spreads to the frontal region, but most often affects the back of the head. Additional studies reveal congestion of the optic discs and inflammation of the inner ear (labyrinthitis). In this case, the patient complains of nausea, vomiting, intense and frequent dizziness. Vomiting indicates direct irritation of the vomiting center by the tumor. Such symptoms require a mandatory differential diagnosis that can exclude otitis media, ear cholesteatoma, Menter's disease and brain nutritional deficiency.
General cerebral clinical manifestations are expressed so strongly and clearly that it is difficult to differentiate damage to the cerebellum. Long-term symptoms are expressed in:
- cranial nerve palsy;
- convulsive muscle contractions that last for 2-3 minutes;
- pyramidal disorders;
- lack of sensitivity.
Damage to the hemispheric structures of the cerebellum is expressed by disturbances in the performance of voluntary movements. These qualitative deviations are determined during the implementation of finger-nose and knee-heel tests.
Cerebellar hemangioma manifests itself in disturbances and disorders of gait, stability and posture. For such patients, instability in the Romberg position, a wobbly “drunk” gait, a forced position of the head tilted to the side, and impaired synchronization of movements are typical.
In addition, the clinical picture of cerebellar damage is manifested in a significant decrease in muscle tone, instantaneous tremor, disproportionately sweeping movements (dysmetria), disproportionately large letters when writing (myelography), inhibited scanned (repetitive) speech, spontaneous oscillatory movements of both eyes - nystagmus. The death of the patient can occur from paralysis of the respiratory center.
In the early stages of a tumor in the cerebellum, symptoms are noted from the location of the tumor. Over time, the tumor compresses the entire body of the cerebellum and the process becomes active on both sides. Global cerebellar syndrome develops with an increase in the process and damage to the cerebellum.
Hemangioblastoma is accompanied by mental disorders in the form of depression, disturbances of consciousness, neurasthenia, and asthenia. Sensory and motor disturbances are complicated by dysfunction of the bladder, large and small intestines when hemangioblastoma is dislocated in the spinal cord and cerebral hemispheres. Involuntary urination and tongue biting, as a rule, do not occur.
Symptoms of hemangioblastoma of the brain and spinal cord
The clinical picture of such tumors depends on their specific location, which can be inside the brain tissue (rarely), in the medulla oblongata (≈2%) or spinal cord (≈4-12%) and the cerebellum (about 85%).
For a clearer picture of the pathology, all signs are divided into several groups: distant, cerebellar and cerebral.
Long-term manifestations include:
- Sensitivity disorders;
- Convulsions;
- Paralysis;
- Disorders of bladder and intestinal activity;
- Movement disorders, etc.
Cerebellar symptoms most often manifest themselves as ataxia, i.e., various walking disorders such as unsteadiness, lack of motor synchronization, and body deviation. The symptoms are supplemented by signs of coordination disorders, handwriting becomes larger, movements are sweeping, speech is slow, pronounced disturbances appear with a sharp change in movement.
Cerebellar symptoms are also characterized by other manifestations such as nystagmus, tremor, muscle hypotonia, etc.
At the initial stage of development, cerebellar hemangioblastoma is localized on the side where clinical disorders appear; however, cerebellar formations are prone to rapid growth, during which the formation of a bilateral formation occurs.
With advanced hemangioblastoma of the cerebellum of the brain, asthenia, neuroses, neurasthenia, stupor with impaired consciousness and other mental disorders develop.
General cerebral manifestations include pronounced hydrocephalus; the patient’s condition is regarded as deteriorated; taking medications does not provide an analgesic effect. The patient complains of constant headaches and dizziness, nausea and vomiting syndrome. Ophthalmoscopy reveals disturbances in the activity of the optic nerves.
Diagnostics
Making a diagnosis of hemangioblastoma is difficult, since its clinical picture is very nonspecific and is camouflaged by neurological and pronounced cerebral manifestations. To clarify the diagnosis, the following is prescribed:
Ophthalmoscopy, EEG, REG and, without fail, magnetic resonance imaging.
- Horizontal and sagittal sections during magnetic resonance imaging differentiate hemangioma from brain abscess, multiple sclerosis, metastases from other affected organs and allows one to determine the exact localization of the process.
- An angiogram with the introduction of a contrast agent shows large and small veins that have pathological changes.
- Histological examination determines the type of tumor and establishes the final diagnosis.
Key characteristics of hemangioblastoma
Unlike cancerous tumors, hemangioblastomas do not invade nearby tissues and are mostly characterized by slow growth, so they leave the opportunity for treatment before any serious complications arise.
According to the World Health Organization (WHO) system of tumors of the nervous system, hemangioblastomas are classified as meningeal neoplasms of undetermined origin. Since their initial study, hemangioblastomas have been found in many areas of the central nervous system. Predominant involvement of the cerebellum and spinal cord has been noted, but the true incidence of this tumor was not discovered until noninvasive diagnostic imaging techniques, particularly magnetic resonance imaging, became available. Together with significant improvements in surgical approaches and microsurgical techniques, this made hemangioblastoma, although dangerous, a potentially curable disease.
Hemangioblastoma has a grade 1 aggressiveness according to the WHO classification and refers to tumors that can arise in the central nervous system or in other parts of the body (kidneys, liver and pancreas). These tumors are usually visualized as sharply demarcated homogeneous masses.
The most common localization sites in percentage terms
Intracranial localization accounts for 87-97% of all cases of hemangioblastoma:
- 95% - in the posterior fossa;
- 85% - in the cerebellar hemisphere;
- 5% - in the medulla oblongata;
- only in rare cases does the pathology extend beyond the cerebellum and cerebellopontine angle;
- 5% - in the supratentorial (usually in the optic rays);
- cerebral hemangioblastomas are observed only in patients with von Hippel-Lindau disease.
Localization in the spine is only 3-13%.
Treatment
Complete removal of the hemangioblastoma is the only treatment. The operation is performed using craniotomy with resection of a section of the occipital bone in the area of the greater occipital fossa and the arch of the first cervical vertebra.
After this, an ectomy of the solid hemangioblastoma node is performed. Partial resection of hemangioblastoma is not allowed, since uncontrolled bleeding may develop during the operation. If the tumor is cystic in nature, it is not completely removed; the contents are aspirated and the dura mater is sutured.
When a tumor wedges into the foramen magnum and compresses the brain stem, the tumor is urgently removed. To reduce the pressure inside the skull, a puncture of the lateral ventricle is first performed. Ventriculostomy, external ventricular drainage, or shunting may be performed as additional measures. These measures normalize the outflow of cerebrospinal fluid in the cranial cavity.
Irradiation of a hemangioma is carried out when it is impossible to remove it, when the inoperable formation is localized in the spinal cord trunk, and as a comprehensive measure after operations. Radiation therapy does not guarantee relapses if the tumor is not completely removed.