Epilepsy is a common neurological disease that manifests itself in the form of seizures. Seizures are expressed in disturbances of consciousness, motor and sensory functions, behavior and emotions. Epilepsy is treatable. But before starting therapy, an accurate diagnosis should be established. A single case of a seizure is not enough to establish the fact of the disease; there must be two or more of them. Electroencephalography is considered one of the most effective examination methods.
At the Yusupov Hospital, this diagnostic method is used to determine epilepsy as one of the main ones.
More about the encephalogram
The essence of the examination is to record the electrical activity of neurons in the structural formations of the brain. An electroencephalogram is a kind of recording of neural activity on a special tape using electrodes. The latter are attached to areas of the head and record the activity of a certain area of the brain.
The activity of the human brain is directly determined by the work of its midline formations - the forebrain and the reticular formation (connecting neural complex), which determine the dynamics, rhythm and construction of the EEG. The connecting function of the formation determines the symmetry and relative identity of signals between all brain structures.
The procedure is prescribed if there are suspicions of various disorders of the structure and activity of the central nervous system (central nervous system) - neuroinfections such as meningitis, encephalitis, poliomyelitis. With these pathologies, the activity of the brain changes, and this can be immediately diagnosed on the EEG, and in addition, the localization of the affected area can be established. An EEG is carried out on the basis of a standard protocol, which records measurements taken while awake or asleep (in infants), as well as using specialized tests.
The main tests include:
- photostimulation - exposure of closed eyes to bright flashes of light;
- hyperventilation - deep, rare breathing for 3-5 minutes;
- opening and closing eyes.
These tests are considered standard and are used for encephalograms of the brain in adults and children of any age, and for various pathologies. There are several additional tests prescribed in individual cases, such as: clenching your fingers into a so-called fist, staying in the dark for 40 minutes, depriving yourself of sleep for a certain period, monitoring night sleep, and passing psychological tests.
Detection methods in adults
How to diagnose epilepsy? Doctors have the right to consider such a diagnosis after two seizures. And most often teenagers or elderly people (60+) are susceptible to the disease.

How to detect epilepsy on EEG?
This is one of the most informative examination methods for this disease.
Its essence lies in the fact that special electrodes are attached to the patient’s head, which record the activity of brain neurons.
There are two types of EEG: regular and video monitoring. During the usual procedure, the patient is laid horizontally, in a dimly lit room, with his eyes closed.
Its duration is no more than 20 minutes. But a single encephalogram may not be effective.
The duration of video monitoring can be from 3 to 10 days, and it is carried out only in a hospital. It can give the most accurate results no later than a day after the next attack.
Video monitoring is carried out by:
- with a single attack of illness;
- in case of repeated night or morning seizures;
- when planning pregnancy;
- before surgery;
- in case of hereditary predisposition.
To identify pathological changes, the patient is asked to quickly open and close his eyes, speed up or slow down his breathing, and turn the lights on and off sharply. All these factors provoke electrical activity in the brain, making it possible to notice possible disturbances.
Is epileptiform activity epilepsy or not?
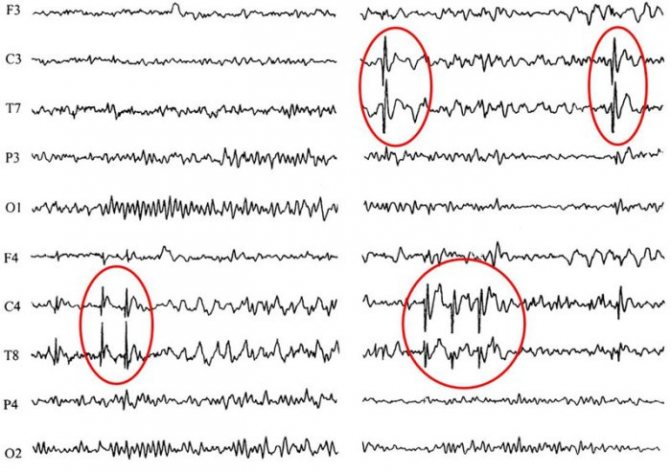
Epileptic activity on the electroencephalogram can be recorded both at the time of a seizure and in a calm state.
It is expressed in the form of single flashes, sharp peaks or waves on the graph. High-amplitude fluctuations in brain activity (150 mKV and above) are signs of epilepsy.
EEG for epilepsy:
Does MRI show epilepsy? What is 3 Tesla MRI for epilepsy?
This procedure appeared later than EEG, but has already gained popularity in the diagnosis of epileptic pathology. It is carried out on devices of different power: 1.5 Tesla and 3 Tesla.
The first of them is considered less powerful and is recommended for examining children and adolescents, but does not always give accurate results.

The second is the most powerful tomograph, which allows you to detect not only neurological abnormalities, but also see metastases in oncology.
Also, such a device will allow you to determine the causes of the pathology and see the localization of brain lesions.
The study is very simple and has virtually no contraindications. Before the procedure, the patient must remove all metal jewelry and change into special clothing.
The doctor talks with the patient and then escorts him to a separate room where the device is located. The patient is placed on a pull-out couch and secured with straps.
The doctor goes into the adjacent room, and the couch moves inside the device. The brain scan lasts about 40 minutes, after which the resulting images are printed and analyzed.
What can be assessed with an EEG?
This type of examination allows you to determine the functioning of parts of the brain in different states of the body - sleep, wakefulness, active physical, mental activity and others. EEG is a simple, absolutely harmless and safe method that does not require disruption of the skin and mucous membrane of the organ.
Currently, it is widely in demand in neurological practice, since it makes it possible to diagnose epilepsy and highly identify inflammatory, degenerative and vascular disorders in the brain. The procedure also provides identification of the specific location of tumors, cystic growths and structural damage as a result of trauma.
EEG using light and sound stimuli makes it possible to distinguish hysterical pathologies from true ones, or to identify simulation of the latter. The procedure has become almost indispensable for intensive care units, providing dynamic monitoring of comatose patients.
What is EEG: the essence of the method
An EEG or electroencephalogram is an effective diagnostic method for patients with signs of epilepsy and other various brain injuries. This method is often prescribed to patients who do not need it at all.
The essence of the technique is that it records electrical signals sent by neurons - nerve cells of the brain. In fact, many pathologies are manifested by severe disturbances in the electrical activity of the brain. Most often this is epilepsy, during which a group of neurons exhibits serious activity, and structural changes in the brain are detected: tumors, cysts, consequences of stroke and hemorrhages.
This technique is considered to be as accurate as possible, and all because it can fully show the entire clinical picture of the disease:
- how far the inflammation has spread and its level;
- what changes have occurred in the vessels;
- early signs of epilepsy;
- neoplasms and stages of their development;
- how much brain function is impaired due to an illness affecting the nervous system;
- what are the consequences of a stroke, hemorrhage or surgery.
According to ICD-10, epilepsy is assigned code G40; a detailed description of the EEG for this pathology allows you to track what changes have occurred in the brain, especially if this study was not carried out for the first time. Thus, the doctor has the opportunity to monitor brain activity during treatment and adjust it at any time. Almost always, after diagnosis, the doctor can accurately determine where exactly the source of excitation is localized.
Process of studying the results
The analysis of the results obtained is carried out in parallel during the procedure, and during the recording of indicators, and continues after its completion. When recording, the presence of artifacts is taken into account - mechanical movement of electrodes, electrocardiograms, electromyograms, and induction of mains current fields. The amplitude and frequency are assessed, the most characteristic graphic elements are identified, and their temporal and spatial distribution is determined.
The transcript of the EEG conclusion is formed on the basis of a set of rules and consists of three sections:
- Description of the leading types of activity and graphic elements.
- Conclusion after description with interpreted pathophysiological materials.
- Correlation of indicators of the first two parts with clinical materials.
Types of human brain activity recorded during EEG recording
The main types of activity that are recorded during the procedure and subsequently subjected to interpretation and further study are wave frequency, amplitude and phase.
The indicator is estimated by the number of wave oscillations per second, recorded in numbers, and expressed in a unit of measurement - hertz (Hz). The description indicates the average frequency of the activity being studied. As a rule, 4-5 recording sections with a duration of 1 s are taken, and the number of waves in each time interval is calculated.
This indicator is the range of wave oscillations of the eclectic potential. It is measured by the distance between the peaks of waves in opposite phases and is expressed in microvolts (µV). A calibration signal is used to measure the amplitude. If, for example, a calibration signal at a voltage of 50 µV is determined on a record with a height of 10 mm, then 1 mm will correspond to 5 µV. In deciphering the results, interpretations are given to the most common meanings, completely excluding rare ones.
The value of this indicator evaluates the current state of the process and determines its vector changes. On the electroencephalogram, some phenomena are assessed by the number of phases they contain. Oscillations are divided into monophasic, biphasic and polyphasic (containing more than two phases).
Rhythms of a waking person
Brain activity recorded on the EEG in an adult has several types of rhythms, characterized by certain indicators and states of the body.
- Alpha rhythm. Its frequency remains in the range of 8–14 Hz and is present in most healthy individuals – more than 90%. The highest amplitude values are observed when the subject is at rest, in a dark room with his eyes closed. It is best identified in the occipital region. It is fragmentarily blocked or completely subsides during mental activity or visual attention.
- Beta rhythm. Its wave frequency fluctuates in the range of 13–30 Hz, and the main changes are observed when the subject is active. Pronounced fluctuations can be diagnosed in the frontal lobes under the obligatory condition of active activity, for example, mental or emotional arousal and others. The amplitude of beta oscillations is much less than alpha.
- Gamma rhythm. The oscillation interval is from 30, can reach 120–180 Hz and is characterized by a rather reduced amplitude - less than 10 μV. Exceeding the limit of 15 μV is considered a pathology causing a decrease in intellectual abilities. Rhythm is determined when solving problems and situations that require increased attention and concentration.
- Kappa rhythm. It is characterized by an interval of 8–12 Hz, and is observed in the temporal part of the brain during mental processes by suppressing alpha waves in other areas.
- Lambda rhythm. It has a small range - 4–5 Hz, and is triggered in the occipital region when it is necessary to make visual decisions, for example, when searching for something with open eyes. The vibrations disappear completely after concentrating your gaze on one point.
- Mu rhythm. Defined by the interval 8–13 Hz. It starts in the back of the head, and is best observed in a calm state. Suppressed when starting any activity, not excluding mental activity.
Epiactivity on EEG
Epilepsy is a disease that is difficult to diagnose in children. A characteristic symptom of the disease is an epileptic seizure. It is not always possible to observe it in a clinical setting.
In order to confirm or exclude the diagnosis of epilepsy, pediatric neurologists recommend doing electroencephalography (EEG).
If epiactivity on the EEG can be recorded during examination, the diagnosis is considered confirmed.
Preparation and carrying out the procedure
Preparation is carried out as follows:
- Before the EEG, you need to inform the specialist about the medications you are taking. Anticonvulsants and tranquilizers are canceled 2-3 days before the procedure, as they can affect its result.
- The day before and on the day of electroencephalography, it is prohibited to drink alcohol, drink coffee, tea, cocoa, or eat chocolate products.
- Before performing the manipulation, you will need to remove metal jewelry (earrings, hair clips, piercings).
- Hair must be washed, skin must be clean and intact. It is advisable to loosen dreadlocks and braids. It is better not to use hairspray and styling foam.
- You need to eat a hearty meal before the procedure.
- If electroencephalography is performed in the sleep phase, then it is advisable for the patient to remain awake for 1-1.5 days before the procedure.
Options for conducting an EEG: during wakefulness, sleep, and also with deprivation of sleep at night. Diagnostics are usually performed during the day. The examination lasts about an hour. A person enters a dark, soundproof room. He is put on a cap with attached sensors or electrodes (about 21) are fixed on the scalp.
The patient sits on a chair or sits down on the couch. The examinee can remain alone in the room, and communication with the doctor will be carried out through a microphone and camera. The electrodes are filled with an electrically conductive substance and connected to an electroencephalograph. The received signal is reflected as wavy lines.
Several times at the beginning of the manipulation, the patient is asked to blink in order to monitor the nature of the changes in the electroencephalogram. The rest of the time the eyes are closed. The recorded vibrations are brain waves. They come in different frequencies and amplitudes, and differ in shape. Doctors distinguish several types of waves. Each of them is associated with the state in which a person is:
- beta waves are recorded in an awake patient;
- during rest, alpha waves are taken into account;
- delta waves are recorded in sleep,
- Theta waves occur during sleep.
To detect hidden pathologies, hyperventilation and stroboscopic stimulation are prescribed. If there is a need to leave for natural needs or to change body position, the person reports this and the diagnosis is suspended.
Confirmation of epilepsy using EEG
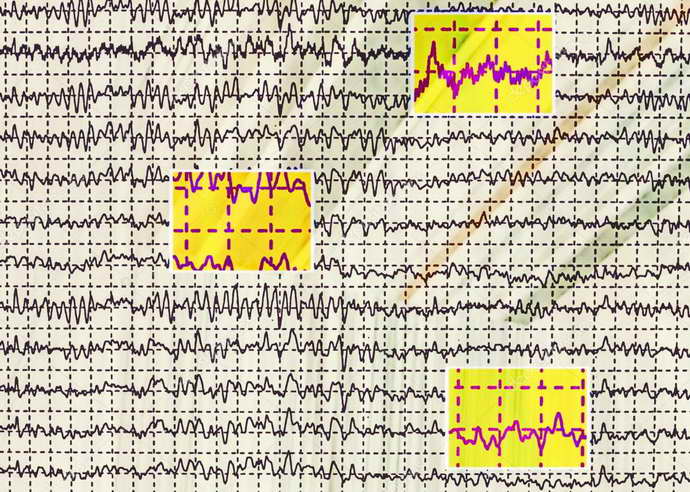
The only reliable EEG signs of the disease are epileptiform activity and epileptic seizure patterns. At the same time, high-amplitude bursts of brain waves can be recorded on the electroencephalogram.
They are not accurate signs of pathology, since epileptic discharges in children can be recorded outside of a seizure.
An EEG study allows you to accurately determine the form of the disease, which helps pediatric neurologists prescribe adequate therapy.
Epiactivity on EEG – what does it mean? A disease that manifests itself as petit mal seizures or epileptic seizures is called “epilepsy.” Epiactivity is a term used colloquially by specialists who perform electroencephalography. It indicates the presence of brain activity on the EEG that is characteristic of epilepsy.
Epiactivity on the EEG in a child without seizures is determined in various ways. Most often, functional diagnostic doctors use light rhythmic provocation to stimulate epiactivity. Hyperventilation or other additional tests may be used.
Sometimes cases of epiactivity can only be detected during long-term EEG recording, which is carried out during night sleep with deprivation (preliminary deprivation of sleep to the child).
Only in a small proportion of small patients is it not possible to confirm the diagnosis with such a study.
CHARACTERISTIC
An indicator of epileptic activity on the EEG is recorded in the form of certain waves, or peaks of an acute nature. Their difference lies in their high amplitude; these are typical graph elements and patterns. They differ depending on the specific form of epilepsy.
When the disease manifests itself in the form of foci, then such changes are characterized by:
- Rolandic epilepsy. In this situation, a wave of sharp peaks is visible. They are collectively called the “Rolandic complex.” They are most often formed in the area of the central temporal leads, face, lips, tongue;
- The focus of nocturnal or frontal epilepsy is localized in the frontal lobes.
Generalized epilepsy, when diagnosed on an EEG, manifests itself in the form of a whole complex of waves throughout the entire region of the brain.
Subclinical patterns are distinguished - these are cases of epilepsy when there are no symptoms as such. This condition is rare and occurs in a small number of patients.
With the help of the procedure, the doctor, in combination with the main methods of treatment, will see the complete clinical picture and make a diagnosis based on this. A neurologist or epileptologist takes into account the patient’s complaints and, if the diagnosis is confirmed, is able to determine the exact form of development of the disease.
Sometimes repeated procedures are performed to confirm a previously made diagnosis. The body is examined using functional tests and loads. The procedure continues for several hours or a day. All results are recorded using video monitoring.
Note! The patient should not self-diagnose. This is done exclusively by the doctor. Self-medication in this case is unacceptable.
VARIETIES
There are the following types of EEG for epilepsy:
- A routine examination is a “routine procedure”. In this case, the doctor registers and records the biopotential in the brain area. This procedure is necessary for detailed registration and recording of biopotentials in the brain area.
- The following types of procedure are the use of functional tests, standard activation procedures:
- In this case, two types of stimulation are used. This is the use of reading, music. This feature is explained by the fact that reflex attacks of the disease are possible during reading or music;
- when irritated, with the help of rhythmic flashing LEDs, an attack is possible;
- the procedure is also performed with hyperventilation.
- A variation using video monitoring.
- Prolonged epileptiform activity in the diagnosis of EEG, night and day sleep.
- EEG recording occurs during the patient's night sleep.
- The next option is to completely deprive the patient of sleep. Another option for sleep deprivation is to wake the patient several hours earlier.
- Use of additional electrodes.
Rhythms in sleep
A separate category of types of rhythms that manifest themselves either in sleep conditions or in pathological conditions includes three varieties of this indicator.
- Delta rhythm. Characteristic of the deep sleep phase and for comatose patients. It is also recorded when recording signals from areas of the cerebral cortex located on the border with areas affected by oncological processes. Sometimes it can be recorded in children 4–6 years old.
- Theta rhythm. The frequency interval is within 4–8 Hz. These waves are triggered by the hippocampus (information filter) and appear during sleep. Responsible for high-quality assimilation of information and forms the basis of self-learning.
- Sigma rhythm. It has a frequency of 10–16 Hz, and is considered one of the main and noticeable oscillations of the spontaneous electroencephalogram, which occurs during natural sleep at its initial stage.
EEG rhythms
During an EGG, the device detects four main types of rhythms:
- Alpha waves are the main element in the diagnosis of a healthy adult patient and are recorded in 90% of people. These waves have a frequency of around 13 hertz per second and are fundamental during wakefulness, when the patient simply lies with his eyes closed. The maximum activity of alpha waves is observed in the area of the back of the head and crown.
- Beta, like alpha waves, are considered normal manifestations in the body of a healthy adult. But the number of their oscillations reaches 35 hertz per second, they are recorded mainly over the frontal part. The beta rhythm appears if the sensory organs are irritated: by touching the patient, when stimulated by light or sound.
- Delta waves with a frequency of up to 3 hertz during decoding of an EEG for epilepsy can mean normal in a baby up to one year old. The indicator partially persists for up to 7 years. In adults, they are recorded during sleep.
- The theta rhythm with a frequency of up to 7 oscillations per second is normally found in children from one to 6 years of age, gradually being replaced by alpha waves as they grow older. In adults they are observed during sleep.
Decoding of electroencephalogram indicators
In order to decipher the EEG and not miss any of the smallest manifestations in the recording, the specialist needs to take into account all the important points that may affect the indicators being studied. These include age, the presence of certain diseases, possible contraindications and other factors.
Upon completion of the collection of all data from the procedure and their processing, the analysis is completed and then a final conclusion is formed, which will be provided for making a further decision on the choice of therapy method. Any disturbance in activity may be a symptom of diseases caused by certain factors.
The normal frequency is determined in the range of 8–13 Hz, and its amplitude does not go beyond 100 μV. Such characteristics indicate a healthy state of a person and the absence of any pathologies. The following are considered violations:
- constant fixation of the alpha rhythm in the frontal lobe;
- exceeding the difference between the hemispheres by up to 35%;
- constant violation of wave sinusoidality;
- presence of frequency dispersion;
- amplitude below 25 μV and above 95 μV.
The presence of disturbances in this indicator indicates a possible asymmetry of the hemispheres, which may be the result of oncological tumors or pathologies of cerebral circulation, for example, stroke or hemorrhage. A high frequency indicates brain damage or TBI (traumatic brain injury).
A complete absence of the alpha rhythm is often observed in dementia, and in children, deviations from the norm are directly related to mental retardation (MDD). Such a delay in children is evidenced by: disorganization of alpha waves, shift of focus from the occipital region, increased synchrony, short activation reaction, overreaction to intense breathing.
In the accepted norm, these waves are clearly detected in the frontal lobes of the brain with a symmetrical amplitude in the range of 3–5 μV, recorded in both hemispheres. A high amplitude leads doctors to think about the presence of a concussion, and when short spindles appear, to the occurrence of encephalitis. An increase in the frequency and duration of spindles indicates the development of inflammation.
In children, the pathological manifestations of beta oscillations are considered to be a frequency of 15-16 Hz and a high amplitude present - 40-50 µV, and if its localization is the central or anterior part of the brain, then this should alert the doctor. Such characteristics indicate a high probability of delayed development of the baby.
An increase in the amplitude of these indicators above 45 μV on a constant basis is characteristic of functional brain disorders. If the indicators are increased in all brain regions, then this may indicate severe dysfunction of the central nervous system.
If a high amplitude of the delta rhythm is detected, a tumor is suspected. Inflated values of the theta and delta rhythm recorded in the occipital region indicate a child’s lethargy and a delay in his development, as well as impaired circulatory function.
Epiactivity on the EEG in a child - what to do?
The only reliable signs of the disease are epileptiform activity on the EEG and seizure patterns.
As a rule, high-amplitude bursts of brain waves are recorded at the same time, but they cannot accurately indicate pathology.
An EEG is necessarily prescribed to confirm the diagnosis, since epileptic discharges can be recorded outside of a seizure. In addition, the study allows you to accurately determine the form of the disease, which helps prescribe adequate treatment.
Epiactivity on the EEG in a child without seizures can be determined in various ways.
Most often, rhythmic light provocation is used to stimulate epiactivity, but hyperventilation or other additional techniques can be used.
Sometimes cases of epiactivity can be detected only during prolonged EEG recording, often performed during night deprivation sleep. Only a small proportion of patients cannot confirm the diagnosis with such a study.
No one will diagnose a child based on EEG alone. These studies may require confirmation or refutation using other methods, including MRI, CT, ultrasound.
The results of electroencephalography can only suggest the presence of a porencephalic cyst in a child, epileptic activity without seizures, paroxysmal activity, tumors, and mental disorders.
Let's consider what doctors may mean when indicating certain pathologies in the EEG conclusion.
- If it is indicated that dysfunction of the middle parts of the brain has been detected, it is worth assuming that the child was simply stressed, that he did not get enough sleep, is often nervous, and therefore it will be enough for him to study with a psychologist, create a favorable environment in the family, reduce psychological stress and light sedatives of plant origin. This is not considered a disease.
- If the electroencephalogram says that interhemispheric asymmetry has been detected, this is not always a sign of pathology in childhood. The child will be recommended for dynamic observation by a neurologist.
- Diffuse changes in the alpha rhythm in conclusion may also be a variant of the norm. The child is prescribed additional tests.
- More dangerous is the detection of a focus of pathological activity, which in most cases indicates the development of epilepsy or an increased tendency to seizures.
- The wording “irritation of brain structures” indicates impaired blood circulation in the brain, the presence of traumatic lesions after blows, falls, as well as high intracranial pressure.
- The detection of paroxysms may be a sign of epilepsy in the initial stages, but this is not always the case. More often, the detection of paroxysms indicates a tendency, possibly hereditary, to epileptic seizures. Increased tone of synchronizing structures cannot be considered a pathology at all. But according to established practice, the child is still referred to a neurologist for observation.
Only a doctor can give an accurate answer to the question of whether everything is okay with the baby. Attempting to draw conclusions on their own can lead parents into such a jungle from which it is very difficult to find a reasonable and logical way out.
Is it only epilepsy that can cause seizures?
No. If your child has a seizure, don't panic. Children often experience seizures due to high fever, so-called febrile seizures.
In order to avoid convulsions due to high temperature, it must be brought down in time.
Above 38 degrees should not be ignored, but immediately reduced with the help of rectal paracetamol suppositories or a lytic mixture.
Not only high temperature, but also a lack of calcium, magnesium, vitamin B6, decreased glucose levels, as well as traumatic brain injury can cause seizures in children.
If your child has a seizure for the first time, you must call an ambulance for hospitalization for the purpose of examining and treating the child.
What should you do if your child has a seizure?
- First, place him on the bed or on the floor away from sharp objects so that the child does not get hurt.
- Secondly, lay him on his side so that the child does not suffocate.
- Third, do not put anything in the child's mouth, do not hold the tongue
If it is an epileptic seizure, it can last up to 2-3 minutes.
After an attack, check your breathing; if there is no breathing, start mouth-to-mouth breathing. Artificial respiration can be performed only after an attack.
You definitely need to be close to the child and not give him anything to drink or medicine until he comes to his senses.
If your child has a fever, be sure to give him a rectal suppository for fever.
What can be seen on the EEG with different forms of epilepsy?
Each type of this pathology is characterized by its own clinical symptoms. In addition, epilepsy looks different on the EEG.
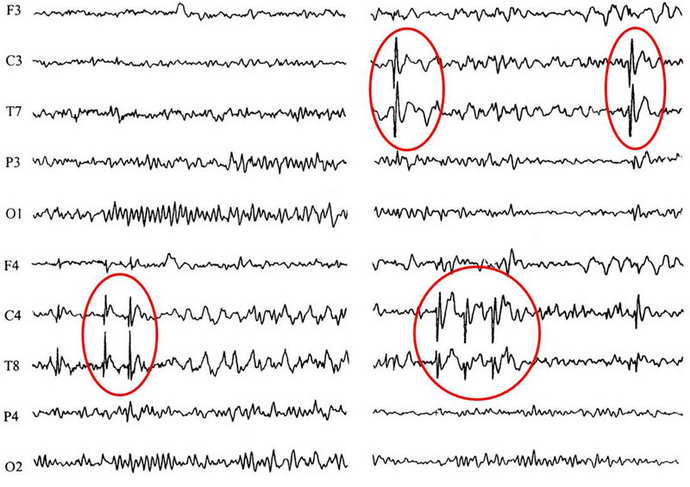
Benign rolandic epilepsy:
- During an attack (exacerbation), a focal epileptic discharge is noted in the middle temporal and central leads. It looks like high-amplitude spikes, in addition to which a combination of sharp and slow waves is observed. Exit beyond the boundaries of the original location is noted.
- In the absence of an attack, focal spikes are often recorded, combining waves that arise simultaneously in several leads. Often, epileptic activity on the EEG does not manifest itself in any way during the daytime while the person is awake. In this case, it necessarily appears as soon as the person falls asleep.
Rolandic epilepsy is the most common form of childhood epilepsy
Epilepsy form Panagiotopoulos:
- During an exacerbation, an epi-discharge is recorded - high-amplitude spikes, combined with slow and sharp waves that rarely remain within the initial localization.
- At rest, multifocal low- or high-amplitude complexes can most often be seen. It is characteristic that the complexes arise serially - at the moment of closing the eyes, and at the moment of opening they are blocked. An attack can be triggered by photostimulation.
Generalized idiopathic epilepsies
EEG patterns can be more often observed in a child and in juvenile epilepsy with absence seizures:
- During an exacerbation, the equipment can show an extensive discharge in the form of rhythmic activity in excess of 10 Hz with a steadily increasing character, as well as sharp waves and high-amplitude delta and theta waves. They are unstable and asymmetrical.
- Outside of an exacerbation, the EEG picture may remain standard, with uncharacteristic activity occasionally present.
Typical absence seizures are short, generalized epileptic seizures with sudden onset and termination.
Early infantile epileptic encephalopathy:
- An exacerbation causes an increase in the number and amplitudes of the spike in combination with sharp waves.
- Outside the exacerbation, there is extensive activity, where the outbreak is followed by its disappearance. Possible hypsarrhythmia.
Lennox-Gastaut syndrome:
- An exacerbation is characterized by the occurrence of numerous spikes and sharp waves; a “spike-slow wave” combination can be recorded. Desynchronization develops.
- Outside of exacerbation - hypersynchronous activity accompanied by sharp waves, spike-slow wave complexes, focal disorders.
Lennox-Gastaut syndrome is a severe form of epilepsy that begins in childhood
Factors that provoke epilepsy attacks
Major attacks begin with convulsions of the whole body, so-called convulsions, and are accompanied by loss of consciousness, severe tension of the muscles of the whole body, flexion/extension of the arms and legs, contraction of the facial muscles, and rolling of the eyes. A major attack may result in involuntary urination and defecation. After an attack, the child experiences post-epileptic sleep.
In addition to major attacks, there may be so-called minor attacks.
Minor seizures include absence seizures, atonic seizures and infantile spasms. Absence seizures are freezing, or short-term loss of consciousness. Atonic attacks are similar to fainting, the child falls, and his muscles are extremely flaccid or atonic during the attack. An infantile spasm occurs in the morning, the child brings his arms to his chest, nods his head and straightens his legs.
Epilepsy can be true and symptomatic, that is, it can be a symptom of a brain tumor. This needs to be dealt with immediately after the diagnosis of epilepsy.
The diagnosis itself is made after an electroencephalogram, on which, in the case of epilepsy, epileptic activity will be observed.
An hour-long EEG is also performed for a more detailed examination.
To rule out a brain tumor, the child undergoes magnetic resonance imaging of the brain.
Epilepsy can be suspected if the child has freezing, or absence seizures, short-term loss of consciousness, in which the child seems to switch off for a few seconds. At the same time, there is precisely absence epilepsy, which occurs without seizures. Sometimes absence precedes an attack. In any case, it is necessary to send the child for an EEG.
Source: https://nevrolog-info.ru/epiaktivnost-na-eeg/
Decoding values in different age intervals
An EEG recording of a premature baby at 25–28 gestational weeks looks like a curve in the form of slow flashes of delta and theta rhythms, periodically combined with sharp wave peaks 3–15 seconds long with a decrease in amplitude to 25 μV. In full-term infants, these values are clearly divided into three types of indicators. During wakefulness (with a periodic frequency of 5 Hz and an amplitude of 55–60 Hz), the active phase of sleep (with a stable frequency of 5–7 Hz and a fast low amplitude) and quiet sleep with flashes of delta oscillations at a high amplitude.
Over the course of 3-6 months of a child’s life, the number of theta oscillations is constantly growing, while the delta rhythm, on the contrary, is characterized by a decline. Further, from 7 months to a year, the child develops alpha waves, and delta and theta gradually fade away. Over the next 8 years, the EEG shows a gradual replacement of slow waves with fast ones - alpha and beta oscillations.
Until the age of 15, alpha waves predominate, and by the age of 18, the BEA transformation is complete. Over the period from 21 to 50 years, stable indicators remain almost unchanged. And from 50, the next phase of rhythmicity restructuring begins, which is characterized by a decrease in the amplitude of alpha oscillations and an increase in beta and delta.
The most common diagnosed pathologies
Thanks to the electroencephalogram, diseases such as epilepsy or various types of traumatic brain injury (TBI) are quite easily diagnosed.
The study allows you to determine the localization of the pathological area, as well as the specific type of epileptic disease. At the time of a convulsive syndrome, the EEG recording has a number of specific manifestations:
- pointed waves (peaks) - suddenly rising and falling can appear in one or several areas;
- the combination of slow pointed waves during an attack becomes even more pronounced;
- sudden increase in amplitude in the form of flashes.
The use of stimulating artificial signals helps in determining the form of epileptic disease, since they provide visibility of hidden activity that is difficult to diagnose with EEG. For example, intense breathing, requiring hyperventilation, leads to a decrease in the lumen of blood vessels.
Photostimulation is also used, carried out using a strobe (a powerful light source), and if there is no reaction to the stimulus, then most likely there is a pathology associated with the conduction of visual impulses. The appearance of non-standard vibrations indicates pathological changes in the brain. The doctor should not forget that exposure to powerful light can lead to an epileptic seizure.
If it is necessary to establish a diagnosis of TBI or concussion with all its inherent pathological features, EEG is often used, especially in cases where it is necessary to establish the location of the injury. If the TBI is mild, then the recording will record insignificant deviations from the norm - asymmetry and instability of rhythms.
If the lesion turns out to be serious, then, accordingly, deviations in the EEG will be pronounced. Atypical changes in recordings that worsen over the first 7 days indicate extensive brain damage. Epidural hematomas are most often not accompanied by a special clinical picture; they can only be identified by a slowdown in alpha oscillations.
But subdural hemorrhages look completely different - with them, specific delta waves are formed with bursts of slow oscillations, and at the same time alpha is upset. Even after the disappearance of clinical manifestations, general cerebral pathological changes due to TBI may still be observed on the recording for some time.
Restoration of brain function directly depends on the type and extent of the lesion, as well as its location. In areas exposed to disturbances or injuries, pathological activity may occur, which is dangerous for the development of epilepsy, therefore, in order to avoid complications of injuries, you should regularly undergo an EEG and monitor the status of the indicators.
Despite the fact that EEG is a fairly simple research method that does not require intervention in the patient’s body, it has a fairly high diagnostic ability. Detection of even the smallest disturbances in brain activity ensures a quick decision on the choice of therapy and gives the patient a chance for a productive and healthy life!
Many EEG changes are not specific, but some of them are quite clearly associated with specific diseases, such as epilepsy, herpetic encephalitis and metabolic encephalopathies. In general, neuronal damage or dysfunction can be judged by the presence of slow waves (theta or delta rhythm) recorded diffusely or over a specific brain region, while diffuse or focal sharp waves or spikes (epileptiform activity) indicate a tendency to development of convulsive seizures.
Consequences of epileptiform activity
EEG patterns of epileptiform activity in children with a family history are associated with epileptic seizures. With some specific combinations, various epileptic syndromes may develop. Important signs of the presence of epilepsy are the presence of epileptiform activity and epileptic seizure patterns on the EEG, as well as high-amplitude bursts of activity (more than 150 μV). Focal benign sharp waves are recorded in children aged 4-10 years, and 4 and 10 years, and a photoparoxysmal reaction - in children under 15-16 years.
With focal benign acute waves, the following negative deviations are observed:
- mental retardation;
- development of Rolandic epilepsy;
- partial epilepsy;
- febrile seizures;
- speech disorders;
- mental disorders;
- various functional disorders.
In the presence of a photoparoxysmal reaction, neurologists identify photogenic epilepsy, symptomatic partial epilepsy, idiopathic partial epilepsy, and febrile convulsions. This pattern is observed with dizziness, migraine, and anorexia. Generalized spike waves are often observed in children under 16 years of age. They are associated with primary generalized idiopathic epileptic conditions: Govers-Hopkins or Herpin-Jantz syndrome, Culp's picnolepsy.
You can perform an EEG at an affordable price to detect epileptiform activity by calling the Yusupov Hospital. An appointment with a neurologist-neurophysiologist is made 24 hours a day, 7 days a week. The results of the study are given to parents after decoding the EEG. The clinic accepts adult patients.

Almost a century and a half ago, in May 1873, the discoverer of the alpha rhythm of the human brain and the creator of the electroencephalography method, Hans Berger, was born in Germany. It should be noted that the very fact of the brain generating electric current was discovered by the Englishman Richard Cato. But it was Berger who, in 1924, was the first to register on paper tape using a galvanometer electrical signals taken from the surface of the head without penetrating the brain. And after he presented the first description of the encephalogram in 1929, a new era began in epileptology.
Pre-surgical examination
The main role in the study during or before surgery is given to the ictal or interictal electroencephalogram. The role of the examination is determined by which surgical intervention should be used in a particular situation. With the help of such an examination, the confirmation and presence of epileptic seizures in people is confirmed. Such an examination provides an opportunity to determine probable epileptogenic foci.
An electroencephalogram allows one to analyze the functioning of the cerebral cortex and confirm the epileptogenicity of supposed painful substances in a situation where a person is diagnosed with refractory epilepsy. This method makes it possible to characterize seizures and determine their consistency with various clinical studies, such as examinations by a neuropsychologist.
Invasive neurophysiological procedures may be performed on patients to confirm the diagnosis. Performing such an electroencephalogram requires the use of coarse electrodes, the implantation of which is performed only under stereotactic observation using MRI equipment. To identify superficial cortical lesions, it is necessary to use subdural electrodes, for the use of which special holes will be needed.
A helmet is placed on a person's head, through which small electrodes are attached to him. They need to be connected to wiring and an electroencephalograph. This technical device allows you to enhance the biopotentials directed to the sensors.
The concept of paroxysmal activity
Paroxysmal states in neurology are the process of an increase in the amplitude of brain activity on the electroencephalogram. An interesting fact is that the amplitude of the waves not only increases sharply, but also does not appear chaotically. In addition to the waves themselves, the source of their origin is also recorded. Sometimes some doctors deliberately narrow paroxysmal activity to epileptic seizures , however, this is not true.
In fact, the concept of paroxysmal activity is much broader; it includes various pathological conditions, in addition to the most well-known disorder - epilepsy. For example, typical wave rises with a center of origin of activity are recorded both in neuroses and in acquired dementia.

An interesting fact is that a child may have paroxysms as a variant of the norm, since paroxysmal activity of the brain will not be supported by pathological changes in the structures of the brain.
Even in the presence of diagnosed foci of paroxysms, doctors believe that before the age of 21 it is too early to sound the alarm - at this time the bioelectrical activity of the brain may not be synchronous and a paroxysmal case is precisely such confirmation.
For adults, it makes sense to talk about paroxysms as a pathological process occurring in the cerebral cortex. If we talk about paroxysm, as the most general concept, we can summarize the following: paroxysm is an intensified attack, occurring at the maximum of its tension and repeating a certain number of times.

Thus, the paroxysmal state will have the following characteristics:
- in the cerebral cortex there is an area with excitation processes that prevail over inhibition processes;
- excitation of the cortex is characterized by a sudden onset and an equally unexpected decline in activity;
- When studying brain impulses, a characteristic pattern is noticeable on the electroencephalogram, in which one can trace the waves reaching their highest amplitude.
Features of the study
Before the procedure, the patient must be prepared, the hair is washed so that there is no residue on it. This will ensure the best interaction between the skin and the electrodes, but the use of styling fixing substances is not permitted. During the diagnosis, a person should not feel hungry. You need to eat food 2 hours before the procedure. Before fixing the sensors, all metal devices, jewelry, gadgets, etc. are removed from the body.
Such a solution can be used after agreement with the therapist, since stopping medications is not always considered possible. An appropriate note is created in the patient’s medical record so that when determining the electroencephalogram, the doctor can determine the effect of such drugs on a positive result.
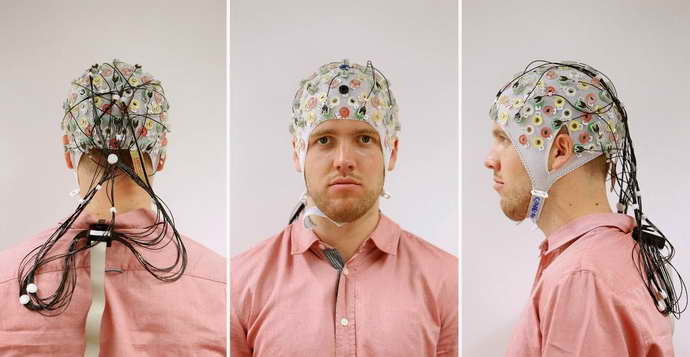
Before you start fixing the electrodes, you need to take measurements in several positions:
- Coverage of the skull.
- Distance from the bridge of the nose to the tubercle of the occipital bone.
- From one ear canal to the next, through the crown along longitudinal and transverse lines.
After this, the location of fixation of the electrodes is identified. Before fixing the sensors, the skin on the head is degreased with alcohol, then this area is treated with a gel that enhances electrical conductivity, and helmets and elastic caps are used.
Patients are seated in a chair or on a couch. He has to close his eyes and stop any body movements during the examination. When an acute respiratory infection occurs, cough, or stuffy nose, the examination has to be postponed.

Epilepsy is detected by EEG in different ways. Even in adult patients, abnormal bioelectrical activity of neurons is often observed due to a genetic predisposition. Some pilots, who are characterized by rapid reactions, display discharges of an epileptoform nature on the EEG.
In patients suffering from psychotherapy, nervous disorders or aggressive people, epileptic phenomena can be detected even in situations where clinical symptoms of the disease are not detected. Often in patients, such changes resolve on their own with age without the use of medications. In 14-15% of children, epilepsy is detected as a result.
Differential diagnosis of seizure
To accurately determine the presence of the disease, you need to study the symptoms. Signs of epilepsy include: passing problems with consciousness, significant changes in the emotional and mental sphere, convulsive syndrome, seizure-like disorders of the functioning of internal organs.

According to the classification approved in 1989, only 3 main types of seizures can be found. These include:
- Symptomatic – occurring due to brain damage or other complex illness.
- Idiopathic – syndromes provoked by hereditary predisposition.
- Cryptogenic – not identified during diagnosis.
There are many other seizures that you need to be able to distinguish. These are neurogenic, somatogenic and psychogenic.
During a seizure, a person falls to the ground, begins to convulse, may scream, and foam comes out of the mouth. Everything lasts about 5-7 minutes, after which it gradually gets worse. The second is characterized by the absence of prolonged loss of consciousness. The man stands still, freezes abruptly, then throws his head up. This condition quickly passes, and then the patient continues daily activities.
Therapy of paroxysms
It is impossible to cure the manifestations of paroxysmal activity until the causes of its occurrence are removed. If a person has suffered a head injury, then doctors try to eliminate the effect of the damaging factor as early as possible and restore blood circulation in the injured area, so as not to provoke the appearance of paroxysmal activity.
If paroxysms appear as a result of increased intracranial pressure, then all measures are taken to normalize blood circulation, and tactics for further prolonged care for such patients are determined.

Major convulsive seizures are more difficult to cope with; they are treated surgically, and the treatment does not always give a stable result.
In cases of a seizure, a sick person must be protected from injury, and after the seizure ends, he must be helped to recover . If the attack lasts longer than 5-7 minutes, it is necessary to call an ambulance and the patient will be given anticonvulsants. For the treatment of non-epileptic paroxysmal conditions, patients are prescribed medications.
Paroxysmal conditions in medical practice have not yet been sufficiently studied. Available data indicate a variety of pathologies, difficulties in diagnosing and treating paroxysms. At the moment, there are a number of conservative and surgical methods for the treatment of paroxysms, however, they still need to be improved to achieve a stable effect.
Provoking tests
A simple EEG recording is performed in a state of inactive wakefulness. Provoking tests are used to identify violations. You need to open and close your eyes. This allows us to determine the level of interaction with patients; as an exception, disturbances of consciousness are detected. This test makes it possible to determine changes in the activity of alpha rhythms and other types of activity when light hits the visual receptors. Alpha rhythms stop being produced when a person is looking somewhere.
Hyperventilation is performed when diagnosing the condition in children over three years of age for a maximum of 3 minutes and up to 5 minutes in adults. Performing such a test is used to determine generalized peak-wave activity and temporal visualization of a seizure. Localized epileptoform activity is not often detected.
Rhythmic photostimulation. The test is used to determine abnormal bioelectrical activity in the photosensitivity type of epilepsy. The lighting device is mounted at a distance of 30 cm in front of the patient’s closed eyes.
In this case, an extended frequency spectrum is used, the initial speed is 1 flash per second. This indicator gradually increases to 50. The most effective in determining epileptiform activity is conventional rhythmic photostimulation with a frequency of 16 Hz.
The photoparoxysmal reaction manifested during such a test is considered a manifestation of epileptoform activity. At the same time, discharges of generalized accelerated polypik-wave activity are recorded on the EEG. Myoclonic paroxysms often appear as contractions of muscle tissue on the face, shoulder girdle and upper limbs. All this is carried out synchronously with the operation of the light bulb.
Epileptiform activity on the EEG: changes characteristic of epilepsy
Electroencephalography allows you to change the bioelectrical activity of nerve cells in the brain and record painful transformations caused by the appearance of foci of epileptic activity in the head. Today, EEG is the only effective way to accurately determine the state of neurons. Below is information about what an EEG shows in epilepsy.
The exact signs of the disease are discharges and patterns of attack. The disorder is characterized by high-amplitude outbursts with varying activity. By themselves, they are not evidence of the development of epilepsy and are determined in the context of the clinical picture.
In addition to diagnosing epilepsy, EEG plays a significant role in identifying the form of the disease. This determines the prognosis for the development of the disorder and the choice of appropriate medications. EEG makes it possible to determine the required amount of drugs to assess the decrease in epileptic activity and to provide for side effects due to the occurrence of additional pathological activity.
To determine epileptoform activity on the EEG, rhythmic light stimulation, hyperventilation and other methods of influence are used, taking into account information about the factors that provoke seizures. Long-term recording during sleep allows the identification of epileptoform impulses and patterns related to seizures. The diagnosis is determined by the characteristic bioelectrical activity of neurons.
The concept of “epileptic activity”
This term is used in two cases:
- Registration of epileptiform phenomena on the EEG during a seizure (psychomotor seizure pattern or ongoing polyspike). The activity may not contain epileptic seizure patterns.
- In the case of a clear activity schedule. Can be recorded outside of an attack .
Hereditary EEG patterns may be associated with epileptic seizures. Some specific combinations have different epileptic syndromes.
The presence of epileptiform activity and epileptic seizure patterns on the EEG, high-amplitude bursts of activity (more than 150 μV) are important signs of the presence of epilepsy.
EEG patterns
Causes of the disease
Many factors can trigger a neurological disorder. The main reasons that can lead to epileptic seizures are:
- genetic predisposition caused by hereditary pathology;
- viral and neuroinfections that affect the brain (meningitis, myelitis, encephalitis, arachnoiditis, etc.);
- brain damage due to toxic poisoning;
- circulatory disorders, internal hemorrhage (stroke);
- traumatic brain injury, concussion, mechanical damage;
- birth trauma, difficult childbirth;
- metabolic disorders of a pronounced nature;
- tumor formations, oncology;
- state of fever.
Using MRI and EEG, a diagnosis of epilepsy can be made by identifying multiple signs of the disease. However, it must be taken into account that these same manifestations may indicate the presence of other pathological processes.
EEG patterns in clinical epileptology
The most studied patterns:
- focal benign sharp waves (FOW);
- photoparoxysmal reaction (PPR);
- generalized spike waves (during hyperventilation and at rest).
FOV is more often registered in childhood, between 4 and 10 years, and FPR in children under 15-16 years of age.
With FOV, the following negative deviations are observed:
- mental retardation;
- febrile seizures;
- development of Rolandic epilepsy;
- partial epilepsy;
- mental disorders;
- speech disorders;
- various functional disorders.
Develops in approximately 9%.
In the presence of FPR, the following are revealed:
- photogenic epilepsy;
- symptomatic partial epilepsy;
- idiopathic partial epilepsy;
- febrile seizures.
FPR is also observed with migraines, dizziness, syncope, and anorexia.
Generalized spike waves
The frequency of FGPs is observed in children under 16 years of age. They also occur very often in healthy children, in about 3% of cases under the age of 8 years.
Associated with primary generalized idiopathic epileptic conditions, for example: Govers-Hopkins or Herpin-Jantz syndrome, Calp's pycnolepsy.
Source: https://neuro-orto.ru/diagnostika/eeg-pri-epilepsii.html