Brain meningioma is usually a benign tumor with initial growth from the arachnoid (arachnoid) membrane of the brain, and not from the dura mater (DMA), contrary to popular belief. The term and classification, which is still in use today, was first introduced by American neurosurgeon Harvey Cushing in 1922. At that time there was no accurate idea of the histological nature of the tumor.
As the brain meningioma grows, it intimately grows into the dura mater and subsequently receives its main sources of blood supply from it. In addition, a meningioma tumor sometimes grows into the bones of the skull. Sometimes it becomes partially or completely calcified (ossified).
Usually this is a slow-growing tumor outside the brain, that is, clearly separated from the brain and having a capsule. Malignant forms with rapid growth are less common. Rarely, brain meningioma is multiple, when it grows simultaneously in different anatomical regions of the cranial cavity. This tumor occurs wherever there are arachnoid cells. Therefore, growth occurs not only inside the skull, but also inside the spinal canal, since the arachnoid membrane also covers the spinal cord.
Brain meningioma is the most common benign intracranial tumor. It happens more often in people aged 40-70 years. More often this disease affects women.
A complete cure is only possible with complete removal of the benign meningioma tumor. This outcome is possible, but highly depends on the location of the tumor.
Features of ischemic stroke of the left hemisphere
The main symptom of a stroke is damage to brain tissue, which impairs motor and speech function and causes paralysis of the right limbs.
Most often, damage to the left hemisphere occurs in people suffering from diabetes, overweight, and increased cholesterol in the body. When a person has a stroke, neurons, the main cells of the brain tissue, are damaged. When the left hemisphere is affected, symptoms are noted on the right limbs.
A left-sided stroke does not occur suddenly; it develops gradually, moving from one stage to another. The first degree, called an ischemic attack, lasts from several minutes to hours, while a person may notice an increase in heart rate and hyperemia of the skin on the face.
If measures are not taken, the disease enters the second stage, which also lasts a long time and is characterized by nausea, fainting or semi-fainting.
Causes
There are many reasons why damage to the area of the brain on the left side can occur. Among them:
- diabetes ;
- arterial hypertension;
- defects , including congenital;
- thrombosis ;
- blood diseases in which its viscosity increases;
- alcohol abuse and smoking;
- migraine;
- use of contraceptives .
The older a person is, the more closely he needs to monitor his health in order to prevent the development of dangerous processes in the body that lead to stroke.
Symptoms
The main symptoms by which you can determine the beginning of the process of brain damage:
- Decreased sensitivity of the limbs. Often there is a strong tingling sensation, accompanied by poor health, numbness in the arm or leg.
- Unnatural position of the corners of the mouth, the face seems skewed, the lower eyelid most often droops on one side.
- Loss of control over oneself, orientation in space.
- Decreased vision, unfocused gaze.
- Pain in the head, often increasing, dizziness.
- Severe vomiting, convulsions.
- Noticeable impairment of speech function.
On this topic
10 reasons for the development of ischemic attack
It is important to notice stroke symptoms within three to six hours of their onset. If you seek help in a timely manner, you can avoid the development of irreversible changes in the brain.
A person can independently diagnose a stroke on the left side of the brain based on the following signs:
- nausea and vomiting;
- numbness of the limbs;
- blurred vision;
- disorientation .
The presence of even two signs is a reason to consult a doctor.
If you notice a person's lack of coordination or speech, you should ask him to smile. In this case, it immediately becomes clear that a stroke has occurred - the corners of the lips will rise unevenly. Another way to diagnose a pathological condition before doctors arrive is to ask the person to stick out his tongue. The tip of the tongue will be directed to the side. Also, the patient will not be able to raise his arms up.
If at least one problem is detected, you need to call an ambulance.
All symptoms that can be detected with ischemic stroke of the left hemisphere are divided into three groups:
- General signs. Symptoms occur when the meninges become inflamed and when blood pressure increases. With the development of left-sided hemisphere damage, there are practically no indicators by which one can immediately understand that pathology has arisen. If the stroke is extensive and the necrosis comes into contact with the meninges, then the signs become more noticeable, especially impaired consciousness, vomiting and nausea, and headache.
- Vegetative symptoms, expressed in heartbeat disturbances, pressure fluctuations. Skin color changes. At the same time, a person often begins to feel the fear of death and tries to fight it.
- Signs of the neurological picture of the disease, which appear depending on the size of the inflammatory focus and its location. Paralysis of the limbs, impaired sensitivity, loss of memory, vision, and hearing occurs.
All these signs can be detected immediately after the development of a stroke. Other symptoms often appear during the recovery stage.
Localization Features
Neurological symptoms that appear over a long period of time and cannot be relieved “help” in making a diagnosis.
A patient with an angioma periodically experiences headaches, non-food nausea, sensory disturbances, and fainting. Depending on which part of the brain the neoplasm is localized and what its nature is (veins, capillaries, or caverns are involved), specific symptoms will appear:
- Venous angioma of the occipital lobe:
- spasmodic sensations in the muscles of the back of the head;
- visual hallucinations (the appearance of long-term images and short-term sparkling).
- Venous angioma of the right temporal lobe:
- Damage to the left temporal lobe, just like the right, disrupts speech and the ability to perceive it. Strong emotional surges are added for no apparent external reasons.
- Venous angioma of the right parietal lobe:
- lack of “right-left” distinction when exposed to stimuli;
- unconscious paralysis.
- Damage to the left parietal lobe leads to loss of orientation not relative to one’s body, but in space (inability to determine distances or read a map).
- Venous angioma of the right frontal lobe:
- emotional instability;
- inability to control your actions;
- euphoric mood;
- loss of the ability to competently construct sentences of any length.
- With a tumor of the left frontal lobe, the patient cannot move on to the verbal formulation of thoughts (he thinks, but cannot speak), and has little control over his own behavior.
In general, capillary angiomas can occur in any part of the brain, and venous angiomas mainly in the cerebellum, the white matter of the brain.
The prognosis depends on the size of the tumor, its benign or malignant quality, and location. Most formations are treatable.
Most often, venous angiomas are located in the white matter of the cerebellum and cerebral hemispheres, near the walls of the ventricles. The temporal lobes are very rarely affected.
In the human body, angiomas can be single or multiple (from 2 to 9% of all cases), then they speak of the angiomatous type of structure of the venous system. The larger the tumor, the more pronounced the symptoms of the disease.
Diagnostics
A left-sided stroke can be diagnosed fairly quickly, which can save a person’s life. A dysfunction of the left hemisphere can be detected by the following signs:
- Loss of consciousness, fainting state.
- Unnatural smile, skewed to one side.
- Impaired balance and movements.
- Drawing, illogical speech.
On this topic
6 reasons for stroke at a young age
The patient may complain of headache, dizziness, double vision. The presence of even one or two symptoms is sufficient reason to call a medical team.
Treatment
Before doctors arrive, primary care must be provided to the patient. While waiting for a medical team, you can improve your condition somewhat by doing a few things:
- Place the person on a surface covered with pillows, with the head raised.
- When you are in the house, open the window.
- Remove all constrictive clothing, unbutton your shirt and belt.
- If a person feels the urge to vomit, gently tilt his head to the side. This is done in order to prevent vomit from entering the throat and respiratory organs.
Doctors in a hospital setting provide basic and specific therapy, which helps minimize damage to nerve cells. Basic therapy is used to preserve the functioning of the brain and cardiovascular system. Specific measures are aimed at restoring blood circulation and brain tissue. The greatest effect is achieved with the combined use of methods.
If treatment does not produce results or is not effective enough, therapeutic and preventive measures and rehabilitation courses are carried out aimed at restoring body functions.
The doctor prescribes the patient to take medications from the following groups:
- Thrombolytics are used in the first hours after a stroke to resolve blood clots.
- Anticoagulants.
- Medicines to lower blood pressure.
- Vasoactive drugs.
- Neuroprotectors.
All medications are selected in accordance with the clinical picture of the stroke.
What is venous angioma, how is it formed?
The blood vessels of the brain, with the participation of lymphatic tissue, can create “tangles” that impede blood flow and nutrition of brain cells.
For example, blood from an artery immediately enters a vein, as a result, the tissues do not receive oxygen. Such vascular formations are called venous angiomas; they can be malignant or benign. Their main danger lies in compression of brain structures, possible rupture of vessel walls and hemorrhagic stroke. Hemorrhage can occur due to the thinness of the tumor walls with a slight increase in pressure, trauma, or emotional stress. If a person did not know about the presence of such structures, then he can only rely on the experience of doctors in making an accurate diagnosis in case of sudden manifestations of the disease (paralysis, significant sensory disturbances, stroke).
With a small size, a brain angioma may not show itself in any way throughout life, which explains the difficulty of diagnosis.
Angiomas grow slowly, from the period of intrauterine development of a person. They are detected during unscheduled examinations, or suspicions of the presence of neoplasms of various natures in the brain.
Angiomas can be either congenital (95% of cases) or acquired (5%). The exact reasons have not yet been clarified. The most proven versions are:
- disruption of the intrauterine formation of the vascular system due to maternal illness, vitamin deficiency, pathological pregnancy;
- concomitant pathology of organs with a high risk of cancer (stomach, liver, mammary glands, lungs, uterus and prostate), this confirms the connection with liver cirrhosis;
- head injuries;
- infectious diseases suffered in early childhood.
It has been proven that children are more prone to the spread and growth of angiomas than adults. This is associated with the functional inferiority of various body systems and insufficient immunity.
Recovery
Speaking about recovery, it should be noted what functions the brain performs and those that may be impaired:
- vision and hearing, smell;
- movements;
- speech;
- the ability to process information of any kind, to read, write;
- understanding the meaning of words;
- memory , both visual and verbal;
- abstract thinking.
The more severe the degree of brain damage, the more various functions are impaired. The recovery process often takes a long time. In many ways, the possibility of recovery depends on how quickly the victim received medical care.
During the recovery process, the patient takes medications, visits a massage room, and undergoes physiotherapy. Classes with a psychologist and speech therapist are of no small importance.
Manual therapy and kinesiotherapy are used, during which the patient is forced to move correctly in order to restore body functions.
source
Consequences of a stroke of the left hemisphere of the brain
Ischemic stroke of the left hemisphere is an acute violation of the blood circulation of the brain in its left hemisphere. A stroke begins suddenly and manifests itself with general cerebral and focal symptoms. The clinical picture of the pathology persists for up to 24 hours and leads to the death of the patient or to consequences in the form of neurological and mental disorders.
The mortality rate of stroke depends on the severity of symptoms and the quality of treatment in the hospital. 35% of all patients die in the first 30 days. The mortality rate in hospital is 24%, and the mortality rate for those treated at home is 43%. More than 50% of all patients die in the first year after an acute condition.
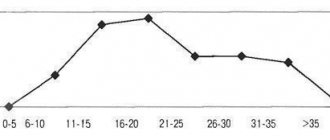
The likelihood of having a stroke increases after age 30. More than 90% of all acute conditions occur between 45 and 60 years of age.
There are risk factors that provoke acute circulatory disorders of the left hemisphere:
- Atherosclerosis of cerebral vessels: due to plaques, blood flow worsens and brain nutrition suffers.
- Hypertonic disease.
- Diabetes.
- Heart failure, coronary heart disease, arrhythmia.
- Passive lifestyle.
- Excess body weight.
- Bad habits and addictions: alcohol, drug addiction, overeating. Especially smoking.
These points are not causes, they only increase the likelihood of developing a stroke.
Consequences of a left hemisphere stroke:
- death;
- permanent loss of some motor functions;
- speech disorder;
- gait disturbance;
- recurrent stroke;
- loss of vision, hearing;
- memory loss.
Forecast
The prognosis depends on the nature and size of the tumor, the age of the patient, and the absence of obvious concomitant pathologies.
The highest chances of cure are in patients with benign tumors of the first stage, accessible for surgical manipulation. In such cases, the probability of recovery is 60-80%.
However, there is always a risk of relapse. Repeated intervention carries additional risks. Therefore, after recovery, you should take maintenance medications and avoid the influence of factors that provoke cancer.
Diagnostics
The most important methods for cerebral circulatory disorders are computed tomography and magnetic resonance imaging.
The first method allows you to distinguish one type of stroke from another. MRI is used to determine the location of the stroke and assess the extent of damage to brain tissue.
At the first signs, it is extremely important to diagnose a stroke of the left hemisphere of the brain on the spot. There are 3 techniques for this. The patient should be asked:
- Smile. Due to damage to the motor centers, the smile can become crooked and the corners of the mouth asymmetrical. Facial expressions are also affected: the eyelids droop, the corner of the lip is directed downward.
- Talk. Let the victim say a simple sentence of a few words. For example, “there is cold water in the river.” Pronunciation is impaired and words are difficult to pronounce.
- Raise both arms at the same time. They should rise evenly and equally. With a stroke, the symmetry of the arm muscles is disrupted.
Additional diagnostic methods:
- Stick out tongue. If the motor nerves are damaged, the tongue may be irregularly shaped, recessed, or not protrude at all.
- Extend your arms in front of you, point your palms up and close your eyes. If one of the arms begins to change position involuntarily, it may be a stroke.

Methods for removing angiomas
In the initial stages, cerebral angiomas are usually asymptomatic and are detected by chance during a brain examination for other diseases. The doctor can suspect the presence of such tumors based on the patient’s complaints, which appear when the tumor increases in size and compresses the brain tissue.
To make a diagnosis and determine treatment tactics, the following instrumental examination methods may be prescribed:
- MRI (with contrast);
- CT (with and without contrast);
- angiography.
You can also read: Arteriovenous malformation of cerebral vessels
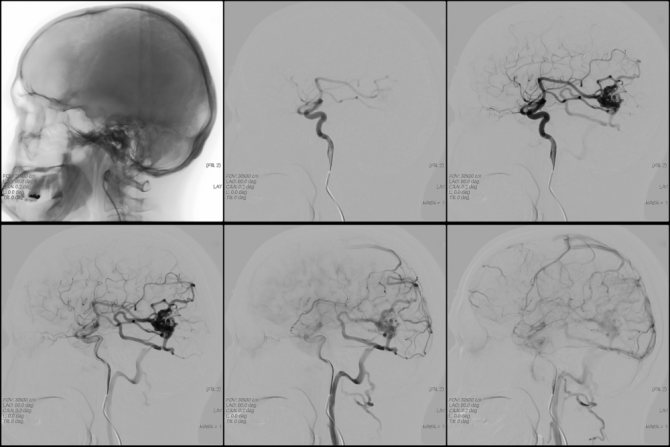
- Angiography is a combination of X-ray examination of the skull with the introduction of a contrast agent into the vessels. The image reveals abnormalities in the blood supply to the brain, the location, size of the angioma, and its connection with the vessels.
- Computed tomography is a recognized non-invasive method (does not involve penetration into blood vessels) and is painless. The results are layer-by-layer images of different depths in a two-dimensional version. This increases the diagnostic capabilities of the method.
- MRI (magnetic resonance imaging) - using magnetic radiation and radio waves, images are more accurate and fine details are highlighted.
- For the purpose of differential diagnosis with different types of intracranial hemorrhage (stroke, rupture of aneurysm), a spinal puncture and examination of fluid from the brain canal are performed in specialized hospitals.
The choice of treatment depends on the diagnostic results.

An appeal to a neurologist with complaints of systemic headaches, nausea, sensory disturbances is the reason for MRI and contrast angiography.
Sometimes we are talking about a neoplasm that is significant in size and significantly affects the performance of the brain. A tumor of this type can be detected in the middle and late stages by performing a non-routine CT or MRI of the head with contrast.
Modern diagnostic methods make it possible to accurately determine the location, size of the tumor, and type of vascular formation.
Venous angioma on MRI
Venous angioma of the right frontal lobe is indicated in the photo by an arrow
As mentioned above, in most cases the pathology discussed in this article begins to develop in utero. In this case, it is recommended to radically solve the emerging problem before the child reaches one year of age. We are talking about surgical intervention. This approach to treatment helps prevent further growth of the pathology, as well as minimize the possibility of their reappearance.
One of the protocols for the treatment of angiomas is the prescription of drugs belonging to the hormonal pharmacological group. But often their use cannot completely eliminate the problem, leaving residual defects. Therefore, in most cases, the most effective way to get rid of the problem is to remove angiomas.

Today, there are various methods for removing angiomas. In some cases, surgical treatment is carried out in stages. The main goal of such treatment is complete removal of tumors and restoration of normal functioning of the vascular and lymphatic systems.
It is worth recalling the most common techniques that can effectively rid a patient of single and group clusters of angiomas.
- Cryotherapy is the burning of pathological tumors using low temperatures (cold). In this case, a refrigerant such as liquid nitrogen is used. This technique is effective and helps prevent bleeding.
- For cavernous angiomas, sclerotherapy is mainly performed. The essence of the technique is the use of special iodine salts, which make it possible to normalize the flow area of certain blood vessels, which has a positive effect on blood flow. The injection is performed in cases where the angioma is located in a place that is difficult to access for larger surgical intervention.
- Electrocoagulation is the cauterization of pathological neoplasms using electric current. This technique has recently been used less and less due to its pain and residual effects in the form of log scars. But this method is simple and cheap.
- Laser treatment. In this case, the process of removing the tumor is carried out in several stages. In this case, layer-by-layer excision of the mutated tissue occurs. This process is repeated until healthy cells appear and mutated ones are completely removed. At the same time, damage to healthy tissue is minimal.
- If it is not possible to achieve the desired result using the above methods, then doctors resort to excision of the tumor with a surgical scalpel.
- The most advanced, but complex and not universally applicable excision techniques are radio and electric knife. Innovative technology makes it possible to easily and practically without leaving stitches to relieve the patient of his problem. It is only worth noting that this technique requires special medical equipment and highly qualified doctors. Today, not every specialized institution can boast of such equipment. At the same time, this procedure is still quite expensive, so not every patient can afford it.
Mostly, the method of removing angiomas is chosen by a dermatocosmetologist. His decision is based on the results of a visual examination of the patient and the capabilities of the clinic. In most cases, sclerotherapy or removal of the tumor using a laser is prescribed. These two techniques are characterized by painlessness and high cosmetic effectiveness of the result obtained over several sessions.
Treatment
Stroke therapy consists of three stages:
The main rule of first aid is to deliver the patient to the nearest clinic as quickly as possible in the first hour after the first sign of a stroke appears.
During transportation, do not give the victim food or drink. The motor nerves of the pharynx may be damaged, allowing food to enter the airway. In the car, provide access to air: unbutton your shirt, take off your tie, open the window. Take care of the victim's comfort.
If the patient begins to vomit, turn him on his side: this way the vomit will not enter the bronchi and block his breathing. It is best for the person to lie down and have a soft bolster or pillow under his head. Try to make sure that the head and neck are in one line.
After admission to the hospital, a diagnosis is made and resuscitation measures begin. Their goal is to support the physiological constants of the body: pulse, blood pressure, oxygen saturation, pressure in the veins. Based on these indicators, doctors determine the chances of survival.
During treatment, the patient needs constant care: he needs to change his underwear, feed him, turn him to the other side to prevent bedsores.
This is the most difficult stage for relatives and staff. The essence of the period is the restoration of lost motor and mental functions, restoration of muscle strength and acquired skills. In general, rehabilitation is social resuscitation. Several specialists care for the patient at once:
- a physiotherapist who helps restore movement functions;
- an occupational therapist who deals with a person’s adaptation to the normal rhythm of life;
- speech therapist, restoring speech apparatus and swallowing.
The prognosis for life is unfavorable. The prognosis for socialization with proper care is relatively favorable.
source
Tumor in the occipital lobe - symptoms
For this location of the tumor, hallucinations, half, quaternary or central losses of visual fields and failure to recognize familiar objects are typical. The patient cannot explain the purpose of an object that he clearly sees. When asked why this item is needed, the patient usually answers correctly, but cannot use it. A chair placed in his path, even after a request to sit on it, will be ignored - the patient will simply go around it or move it out of the way. As the tumor develops, such unconscious and strange behavior becomes more and more common.
A special feature of this location of the tumor is an extremely rare increase in intracranial pressure.
Main functions
Ever since school, everyone knows about the cross-function of the cerebral hemispheres. Thus, the left hemisphere is responsible for the functioning of the right side of the body . That is, the movement of the right leg and right arm is controlled by the left hemisphere. In addition, the left side of the brain has other areas of responsibility:
- Logics.
- Analysis processes. The left side of the brain helps us recognize numbers and analyze facts.
- Speech function. Understanding the semantics of a statement through the work of the left hemisphere is limited to the literal meaning. The ability for imaginative thinking in people with a predominant left hemisphere is poorly developed.
- Ability to read.
- Stage-by-stage and detailed processing of information material.
- The ability to identify a chain of cause-and-effect relationships.
- Literacy. People with a developed left hemisphere naturally have the ability to write accurately.
Signs and symptoms

As a result, the tissues do not receive enough blood and nutrients along with it. Nerve cells die. In parallel, general cerebral and focal symptoms develop. General cerebral ones include:
- Headache.
- Convulsive attack.
- Nausea, vomiting.
- Violation of spatial orientation.
Manifestations of the vegetative system:
- The heart begins to beat faster.
- Blood pressure changes. Both an increase and a decrease in indicators are possible.
- Muscle weakness.
Focal symptoms depend on the specific location of the pathology in the left hemisphere. The initial symptoms often remain as consequences of a stroke.
- Changes in sensitivity (numbness, tingling sensations).
- Difficulty in motor functions on the opposite side of the body.
- Impaired sensitivity.
- Hearing and vision problems.
- Speech dysfunction.
- Asymmetrical face. Facial muscles, like all others, also have a control center in the brain. With an ischemic stroke on the left, a characteristic sagging of the cheek, eyelid and corner of the mouth appears on the right side.
Tumor in the parietal lobe - symptoms
Initially, symptoms manifest as a significant decrease in sensitivity in one of the limbs. Over time, a unilateral lesion becomes clearly noticeable. The described signs are observed in the left arm and left leg if the tumor is localized on the right side and vice versa.
The location of the tumor growth center is in the lower part of the parietal area. leads to loss of reading, writing, counting skills and speech impairment. These symptoms manifest themselves in the same way in both congenital right-handers and left-handers, but only with a mirror-like different location of the tumor.
Treatment
Therapeutic actions aimed at eliminating a stroke must be taken within three hours from the onset of the pathology, which is why it is important to provide first aid correctly and call an ambulance in time. In this case, the prognosis for saving life and further recovery is favorable. Treatment is carried out comprehensively, using medications, physiotherapy and speech therapy sessions.

In the list of pharmaceuticals for ischemic stroke of the brain:
- Thrombolytic agents aimed at resolving thrombotic plaques. They are prescribed urgently.
- Anticoagulants thin the blood, preventing it from clotting.
- Neuroprotectors. Restore metabolic processes in the brain and prevent damage to neural connections.
- Medicines against high blood pressure.
- Surgical intervention is prescribed when an extensive hematoma is detected.
Consequences
The consequences of the disease are visible from the first minutes of the onset of stroke. They are also determined by the functions for which the left hemisphere is responsible.
- Restriction or complete paralysis of the right side of the body . Affects both the muscles of the limbs and other parts of the body. Especially noticeable in facial expressions. Muscle paralysis leads to the fact that a person is unable to move on his own, and constant pain in the limbs causes discomfort and suffering.
- Speech impairment . The person begins to talk incoherently. The rate of speech slows down due to impaired articulatory motor skills. The semantic content of the statement is lost. The disorder affects all levels of speech production: from perception and understanding to reproduction.
Tumor in the frontal lobe - symptoms
This localization of the tumor site hides it for a long time - it remains unnoticed due to the lack of clear symptoms. As they grow, cerebral symptoms appear. They are expressed by a gradual change in the patient’s behavioral reactions, especially noticeable in unusual, stressful situations. As the disease progresses, the symptoms worsen and become obvious.
For a tumor localized in the left part of the frontal lobe of the brain, it is typical to manifest itself with speech disorders - at first, speech becomes not as smooth and relaxed as usual, unusual and incorrect pronunciation of sounds occurs. At this stage, such problems are clearly felt by the patient himself, but he cannot fix anything and is nervous. As the tumor grows, the symptoms are complemented by a decrease in the tone of the muscles of the tongue and the right side of the face.
The described symptoms are true for congenital right-handed people, and in left-handed people, such manifestations are observed with a tumor located on the right side of the frontal lobe of the brain.
Localization of the tumor in the upper part of the frontal lobe causes weakness of the lower extremities - one or both, and further development of the situation is accompanied by problems with the organs of the pelvic girdle.
Rehabilitation and lifestyle

- Massage sessions perform several functions at once:
- restore blood circulation in paralyzed parts of the body;
- prevent bedsores;
- The massage time is gradually increased from session to session from 5 minutes to 30.
- Physical exercise at the treatment stage is possible in a passive form. Gymnastics starts with the arms. It is important to move not only the affected limbs, but also healthy ones.
- In a sitting position, the muscles of the eyeball and neck are developed.
- They are working on regaining fine motor skills.
Classification.
Regarding histology:
- Meningothelial, Fibrous, Transitional, Psammomatous, Angiomatous, Microcystic, Secretory, Lymphoplasmacytic, Metaplastic (Grade I, benign).
- Atypical, Chordoid, Clear cell (Grade II, second degree of malignancy). They grow quickly and often recur.
- Papillary, Rhabdoid, Anaplastic (Grade III, malignant). It grows even faster and recurs more often.
Grade is the degree of malignancy of CNS tumors. There are four degrees. Developed by the World Health Organization (WHO).
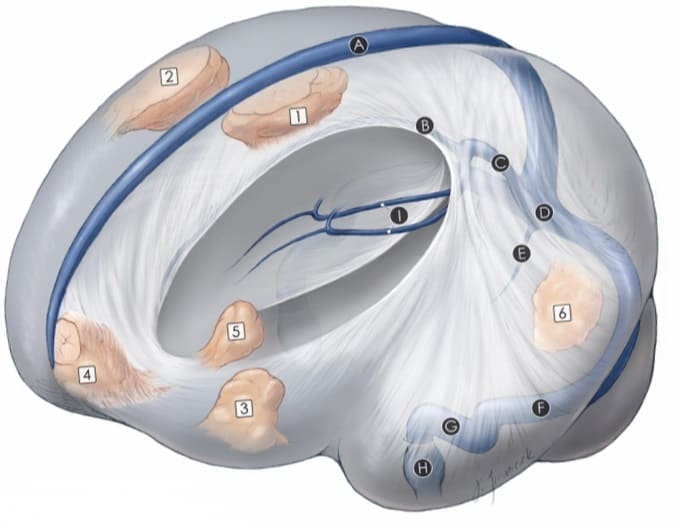
Regarding the base of the skull, meningioma is distinguished:
- anterior cranial fossa (ACF);
- middle cranial fossa (MCF);
- posterior cranial fossa (PCF).
Regarding the tentorium cerebellum there are:
- supratentorial, localized above the tentorium;
- subtentorial, localized under the tentorium.
By location:
- Parasagittal meningioma of the brain.
It occurs most often and is divided into tumors of the anterior, middle or posterior third of the superior sagittal sinus.
- Convexital meningioma of the brain.
Happens less often than the previous one. Located on the surface of the brain, which covers the cranial vault. Superficial tumor, in other words.
- Meningioma of the skull base.
It is less common to be convexital and parasagittal.
| Type of meningioma | Location |
| olfactory pit | HRC center |
| lesser and greater wings of the sphenoid bone | SCHYA |
| tubercle of sella turcica | center of the SCN, next to the pituitary gland |
| petroclival | on the clivus in the PCF and in front of the brain stem |
| foramen magnum (FOM) | PFC, next to the BZO, through which the brain stem passes |
| pyramids of the temporal bone | anatomical formation of the temporal bone with the same name |
- Falx meningioma and meningioma of the tentorium cerebellum.
Between the hemispheres of the brain there is a falx-shaped process (falx). The occipital lobes of the brain are separated from the cerebellum by the tentorium. These formations are processes of the dura mater, in the area of which the tumor grows.
- Intraorbital.
Grows in the orbit where the eyeball is located. The source is the arachnoid membrane of the optic nerve. Rare occurrence among all meningiomas.