Find out more about diseases starting with the letter “Z”: Stuttering, Malignant tumors of the spinal cord.
This is a dangerous disease that can behave like other illnesses. It remains invisible for a long time. Only after the tumor becomes large can the disease be diagnosed.
The development of pathology is accompanied by a wave-like increase in symptoms due to compression of the nervous tissue. Painful sensations appear, sensitivity and motor function are impaired. The diagnosis is determined after examination, magnetic resonance imaging, and puncture.
General concept
Malignant neoplasm of the spinal cord is a group of tumors “born” from the membranes and roots of the spinal cord. Shows itself at any age. Most often occurs in people between 30 and 55 years old. Men suffer from this disease more often than women.
Clinical signs depend on the level of damage and how the tumor is located in relation to the substance and lining of the brain, as well as how it adheres to the surface of the spinal cord.
Treatment is carried out by specialists: oncologists, neurosurgeons, neurologists.
Treatment of spinal cord tumors: conservative therapy or surgery?
The only treatment for spinal cord tumors is radical surgery to remove the tumor and the tissue affected by it.
But we must understand that the location of the pathology in this case is a complex structure that is difficult for surgical access and manipulation.
That is why early diagnosis of spinal cord tumors is very important, when the chances of effective surgery and complete removal of the tumor are high.
With correct diagnosis and timely surgery, there is a high chance of a complete cure for the patient and restoration of his ability to work.
Even with a malignant neoplasm, surgical treatment is performed in order to delay the progression of the pathological process, reduce the symptoms of neurological disorders and pain.
Conservative methods of treating spinal cord tumors - is it possible to do without surgery?
Conservative methods in the treatment of spinal cord tumors are used as auxiliary methods to reduce pain and neurological disorders.
- Therapy uses painkillers and anti-inflammatory drugs, vitamins and restoratives, and diuretics.
- The patient is prescribed a special motor regimen, given recommendations on nutrition and exercise, and may be recommended to wear a support corset and/or a Shants collar.
As a rule, treatment is performed in a hospital setting .
Unfortunately, conservative treatment alleviates the symptoms of the disease only for a while, and then the symptoms progress.
Therefore, therapy methods are used during diagnostic procedures and at the stage of preparing the patient for surgical treatment, as well as after surgery.
01 September 2020
Classification
A malignant tumor of the spinal cord, depending on the location, is divided into:
- primary - comes from the medulla and surrounding tissues;
- secondary - the result of distant metastases.
Based on their origin they are divided into:
- intramedullary tumors - formed from the brain matter;
- extramedullary - develop from membranes and roots.
The former are located inside the spinal cord, the latter - outside it. Extramedullary are divided into:
- located under the membrane of the brain (subdural);
- located above the membrane (epidural).
Pathology is most often a consequence of metastases of lung and breast cancer, lymphoma. Based on histology, neoplasms are divided into:
- hemangiomas and hemangiopericytomas;
- schwannomas and angiomas;
- dermoids and epidermoids;
- chondromas.
The most common are meningiomas and neuromas.
Forecasts and possible consequences
If the spinal cord is compressed by a tumor, a person faces disability
If a spinal cord tumor has been diagnosed, symptoms and prognosis, treatment and rehabilitation are determined by the doctor individually. With a benign tumor, a person can live a long time, as the prognosis is favorable. If the conduction of nerve impulses is disrupted, a person’s quality of life is significantly reduced. At the same time, one has to put up with a disability, which consists of paralysis of the limbs.
With a malignant neoplasm, daughter tumors form - metastases in distant areas of the body, and at the same time severe intoxication develops, which can cause death. The main negative consequence is a total transverse lesion of the spinal cord with complete blockade of impulses.
Source
D10 | Benign neoplasm of the mouth and pharynx | |
D10.0 | Lips | |
D10.1 | Language | |
D10.2 | Floor of the mouth | |
D10.3 | Other and unspecified parts of the mouth | |
D10.4 | Tonsils | |
D10.5 | Other parts of the oropharynx | |
D10.6 | Nasopharynx | |
D10.7 | Laryngopharynx | |
D10.9 | Throats of unspecified location | |
D11 | Benign neoplasm of the major salivary glands | |
D11.0 | Parotid salivary gland | |
D11.7 | Other major salivary glands
| |
D11.9 | Major salivary gland, unspecified | |
D12 | Benign neoplasm of the colon, rectum, anus (anus) and anal canal | |
D12.0 | Cecum | |
D12.1 | Appendix | |
D12.2 | Ascending colon | |
D12.3 | Transverse colon | |
D12.4 | Descending colon | |
D12.5 | Sigmoid colon | |
D12.6 | Colon, unspecified part | |
D12.7 | Rectosigmoid junction | |
D12.8 | Rectum | |
D12.9 | Anus (anus) and anal canal | |
D13 | Benign neoplasm of other and ill-defined digestive organs | |
D13.0 | Esophagus | |
D13.1 | Stomach | |
D13.2 | Duodenum | |
D13.3 | Other and unspecified parts of the small intestine | |
D13.4 | Liver | |
D13.5 | Extrahepatic bile ducts | |
D13.6 | Pancreas | |
D13.7 | Pancreatic islet cells | |
D13.9 | Ill-defined locations within the digestive system | |
D14 | Benign neoplasm of the middle ear and respiratory organs | |
D14.0 | Middle ear, nasal cavity and paranasal sinuses | |
D14.1 | Larynx | |
D14.2 | Trachea | |
D14.3 | Bronchi and lung | |
D14.4 | Respiratory system, unspecified location | |
D15 | Benign neoplasm of other and unspecified organs of the chest | |
D15.0 | Thymus gland | |
D15.1 | Hearts | |
D15.2 | Mediastinum | |
D15.7 | Other specified organs of the chest | |
D15.9 | Chest organs, unspecified | |
D16 | Benign neoplasm of bones and articular cartilage | |
D16.0 | Scapula and long bones of the upper limb | |
D16.1 | Short bones of the upper limb | |
D16.2 | Long bones of the lower limb | |
D16.3 | Short bones of the lower limb | |
D16.4 | Bones of the skull and face | |
D16.5 | Lower jaw bone part | |
D16.6 | Spinal column | |
D16.7 | Ribs, sternum and collarbone | |
D16.8 | Pelvic bones, sacrum and coccyx | |
D16.9 | Bone and articular cartilage, unspecified | |
D17 | Benign neoplasm of adipose tissue | |
D17.0 | Skin and subcutaneous tissue of the head, face and neck | |
D17.1 | Skin and subcutaneous tissue of the body | |
D17.2 | Skin and subcutaneous tissue of the extremities | |
D17.3 | Skin and subcutaneous tissue of other and unspecified locations | |
D17.4 | Chest organs | |
D17.5 | Intra-abdominal organs | |
D17.6 | Spermatic cord | |
D17.7 | Other localizations | |
D17.9 | Unspecified localization
| |
D18 | Hemangioma and lymphangioma of any location | |
D18.0 | Hemangioma of any location
| |
D18.1 | Lymphangioma of any location | |
D19 | Benign neoplasm of mesothelial tissue | |
D19.0 | Pleura | |
D19.1 | Peritoneum | |
D19.7 | Other localizations | |
D19.9 | Unspecified localization | |
D20 | Benign neoplasm of soft tissues of the retroperitoneum and peritoneum | |
D20.0 | Retroperitoneal space | |
D20.1 | Peritoneum | |
D21 | Other benign neoplasms of connective and other soft tissues | |
D21.0 | Heads, faces and necks | |
D21.1 | Upper limb, including the shoulder girdle area | |
D21.2 | Lower limb, including hip area | |
D21.3 | Chest | |
D21.4 | Belly | |
D21.5 | Taza | |
D21.6 | Torso part unspecified | |
D21.9 | Unspecified localization | |
D22 | Melanoform nevus | |
D22.0 | Lips | |
D22.1 | Eyelids, including commissure of eyelids | |
D22.2 | Ear and external auditory canal | |
D22.3 | Other and unspecified parts of the face | |
D22.4 | Scalp and neck | |
D22.5 | Torso | |
D22.6 | Upper limb, including the shoulder girdle area | |
Development of pathology
Primary tumors may differ from each other in their origin:
- matting connective tissue cells of hard structures, ligaments, tendons give impetus to the formation of extradural sarcomas;
- cells of the lining of the brain provoke the appearance of intradural meningiomas;
- nerve roots are the root cause of neurofibromas;
- neuroglial cells contribute to the formation of intramedullary astrocytomas;
- cells lining the spinal canal give rise to ependymoma.
The neoplasms listed above can be benign or malignant.
General symptoms of pathology
Signs indicating a problem:
- Increasing dysfunction of the spinal cord.
- Pain in the area of injury. At first she is fickle. Appears with sudden movement, straining, coughing. As the tumor grows, the pain intensifies. The pain becomes constant.
- Sensitivity disturbance occurs. There are cases when problems with sensitivity and movement immediately arise, and then pain is added to them.
The nature of the signs of the disease depends on the type of neoplasm.
Intramedullary:
- The patient feels weak in the legs and arms, and quickly gets tired when moving. Pelvic dysfunctions begin to manifest themselves. After some time they develop into severe pelvic disorders.
- Pain and tactile sensitivity fades. Paresis turns into paralysis. Bedsores appear.
Extramedullary neoplasms:
- Radicular syndrome begins to develop. Then compression myelopathy is added to it.
Symptoms are influenced by the location of the tumor in relation to the surface of the spinal cord.
- Lateral sections - motor ability is impaired on the side where the tumor is located. Sensitivity disappears on the opposite side.
- The anterior or posterior part of the spinal cord is determined by neurological disorders.
The spread of motor and sensory disorders depends on the type of origin of the pathology.
- Extramedullary - ascending disorders. The problem begins to appear in the distal parts of the limbs. Spreads proximally. Sensitivity may remain in the perineal area.
- Intramedullary - descending disorders. There is no sensitivity in the perineal area.
A specific symptom of spinal cord tumors is narrowing and subsequently blockade of the subarachnoid space.
To confirm the diagnosis, the patient is prescribed an X-ray contrast study. The next procedure that confirms the blockade is a lumbar puncture with liquorodynamic tests.
Main types of spinal cysts. Diagnostic and treatment methods
Cyst on the body › Main types of spinal cysts. Methods of diagnosis and treatment.
03.03.2020
Spinal cysts are rare among spinal column diseases (about 1%). In most cases, it is benign and may not show its symptoms for a long time.
What is a neoplasm and why is it dangerous?
A cyst in the spine is a cavity filled with serous fluid, located in different parts of the spinal column.
Like most neoplasms, it has a round shape, a capsule separating it from the tissues in which it is located and the contents of the cavity.
A cavity, even a small one, can be dangerous. Especially if it is located in the canal of the spinal column, where cerebrospinal fluid flows.
The danger of a cyst in the spine lies in quite serious complications:
- Liquor block, which contributes to increased intracranial pressure. The result is constant and intense headaches.
- When pressure is placed on the spinal cord, symptoms of impaired limb movement (paresis and paralysis) occur.
- When pressure is placed on the vessels supplying the spinal cord, a spinal stroke can occur.
- Symptoms of compression of internal organs.
A small cyst located away from nerve fibers and plexuses, as well as blood vessels supplying the spine, can resolve on its own.
Types and locations of localization
The classification distinguishes several divisions:
By location:
- cervical cyst;
- thoracic region;
- cyst in the lumbosacral spine.
By origin:
- congenital;
- acquired.
By structure:
Types of neoplasms:
- A perineural (cerebrospinal fluid) cyst is a cavity located in the spinal canal itself, containing cerebrospinal fluid (CSF).— When it increases in size, it causes symptoms of compression of the spinal nerves (severe pain and neurological deficit).— When the nerves are compressed, PKOP can manifest itself as pain radiating to the joint area of the limbs.
- Which can imitate the symptoms of a hip cyst or arthrosis (pain in this area). - Arachnoid cyst.—Often affects a couple of segments of the spinal cord, can grow into the intervertebral space.—Located on the posterior and posterolateral-lateral surface of the dural sac. Morphologically classified into types:—extradural cysts without nervous tissue;—extradural arachnoid;—sacral meningocele;— Tarlov cyst;
- intradural neoplasm. - Periarticular (paraarticular) cyst is a formation affecting the facet joint of the spine. It can be part of the joint, located nearby or grow into the ligamentum flavum. It has two subtypes: synovial cyst: located in the posterolateral part of the spinal canal, the inner part of the cavity is covered with synovial epithelium, filled synovial fluid;
- ganglionic: located in the surrounding soft tissues of the joint, does not contain synovial epithelium. - Syringomyelic cyst: a sign of a chronic disease - syringomyelia. — The result of expansion of the longitudinal canal of the spinal cord. Most often found in the cervical spine.
- The aneurysmal form of formation is a cavity located inside the bone tissue. — Arises due to its expansion; it contains venous blood inside.
- Paravertebral cyst - a cavity located in the soft tissues surrounding the spine
Etiology
Cysts on the spine have various causes.
Often, such defects are formed as a result of exposure to external factors:
- Injuries to the spine and spinal canal are the main cause of the formation of tumors.
- Infectious processes.
- Uneven and intense loads.
- Dorsopathies of intervertebral disc tissue (including herniated disc), ligamentous apparatus, intervertebral joints.
- Passive lifestyle.
- Hemorrhages affecting the spine.
- Obesity, which results in improper formation of the muscle corset (or lack thereof).
- Parasitic infestation.
Most rarely, a neoplasm occurs at the time of the formation of organs and systems during intrauterine development. In such cases, the cyst is congenital.
Symptoms
The symptoms of a spinal cyst depend on its type, location and size.
Small formations may not manifest themselves (be asymptomatic) and may be detected by chance during an MRI of the spine.
As the size of the tumor increases, symptoms of compression develop. The manifestation of which depends on the part of the spine where it is located.
- Pain syndrome.—In most cases, the very first sign of the disease.—Can manifest itself as chronic, aching pain, present both at rest and during movement.
— As the tumor grows, severe back pain may occur that cannot be treated with analgesics. - Increased intracranial pressure: - tinnitus; dizziness;
severe headaches. - Sensitivity disturbance: - numbness;
- paresthesia. - Neurological disorders: - weakness of the limbs (paralysis and paresis);
- changes in the pelvic organs (functional disorders) with formations located in the lumbar region and sacrum.
Diagnostics
First, you need to consult a neurologist, who will prescribe the necessary examination, based on the results of which he will make a diagnosis.
If surgical treatment is necessary, consultation with a neurosurgeon is necessary.
For differential diagnosis use:
- studying the anamnesis (to determine the nature of the pain syndrome and its duration);
- blood tests (biochemical tests);
- neurological status (definition of functional disorders);
- X-ray of the spine in several projections (to assess the bone structure);
- Ultrasound of the spine (to evaluate soft tissues);
- magnetic resonance imaging (for detailed visualization);
- myelography (to assess the patency of fluid in the spinal canal);
- electromyography (used when symptoms of compression of the spinal roots appear, to determine the location of the tumor);
- biopsy of the contents of the cyst cavity (to exclude a malignant process).
Therapy methods
In most cases, it is necessary to treat the cyst.
Neoplasms of the spinal column can be treated:
- promptly;
- conservatively (treatment without surgery).
Traditional treatment
Small cysts can be treated without treatment. Such formation can resolve on its own. But you need to monitor the pathology (periodically undergoing instrumental examinations).
Taking medications will help relieve symptoms and shorten recovery time.
Such medicines include:
- analgesics and NSAIDs for pain relief;
- vitamins (especially group B) improve trophism and metabolic processes in the body (including the spine).
Physiotherapy
The most effective physiotherapeutic methods are:
- acupuncture for spinal cysts - helps reduce pain and sensory disturbances (pins and needles sensations, burning and coldness of the extremities);
- electrophoresis and phonophoresis (improves tissue trophism);
- massage (only as prescribed by a doctor, in the absence of contraindications).
Exercise therapy
Therapeutic exercises help relax muscles and relieve pain. Initially, it is better to perform the exercises under the supervision of an instructor, but for better effectiveness, repeat them yourself several times a day.
Swimming is gentle on the spine and is preferable.
Principles of physical therapy:
- avoid sudden movements (this may aggravate symptoms);
- move from simple to complex exercises;
- a clear program and performing exercises in several approaches;
- supervision of a doctor or exercise therapy instructor;
- If discomfort and pain appear, training should be stopped.
Laser treatment
Laser treatment (burning out the cyst with a laser) has advantages over classical surgical interventions:
- passes without blood;
- minimal surgical access;
- postoperative complications are minimal;
- rapid tissue regeneration in the area of the postoperative wound.
Prices for laser removal of a tumor depend on its size, and in some cases it can be performed free of charge.
Surgical correction
Surgery to remove a spinal cyst is a method to avoid relapse of the disease. The cost of surgical intervention depends on its type.
- Puncture method.— Puncture is performed under local anesthesia.
— A special needle is used to pump out the contents from the tumor cavity. - Radical excision. — Excision of the cyst is carried out using a classic approach and can be complicated by damage to a segment of the spinal column.
- Endoscopic removal. — Using endoscopic equipment, the cyst is desquamated through minimal access.
- Radiotherapy.—Radiation therapy is the method of choice in the presence of absolute contraindications to surgery.
— Accurate selection of the radiation dose is important to avoid damage to the spinal cord.
ethnoscience
Treatment of spinal cysts with folk remedies can be used as an aid to the main type of therapy.
Traditional methods of treatment include:
- burdock juice;
- elecampane grass;
- chaga;
- Walnut.
In most recipes, dry substances mixed in the required proportions must be infused and taken orally.
It is important to remember that traditional methods of therapy cannot be replaced with herbal treatment and medical supervision is necessary.
Possible consequences and complications
With timely diagnosis and treatment of the tumor, the risk of complications is minimal.
In some cases, you may experience:
- rupture of the cyst cavity;
- tumor recurrence;
- compression symptoms;
- consequences of surgical treatment (bleeding, infections).
Prevention
Preventive measures include nonspecific measures: a healthy lifestyle, strengthening the muscle and bone structure of the spinal column.
- acceptable physical activity (yoga, swimming, walking);
- periodic back massage courses;
- proper nutrition;
- correct distribution of the load on the spine;
- clinical examination.
Conclusion
A spinal cyst is a formation that, if detected and treated in a timely manner, goes away without consequences. To avoid the appearance of dorsopathies of the spine, it is important to follow preventive measures and maintain an active lifestyle.
Main types of spinal cysts. Methods of diagnosis and treatment. Link to main publication
Source: https://kistabolezn.ru/kista-na-tele/kista-pozvonochnika.html
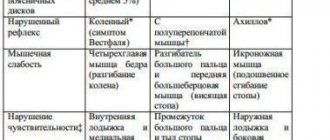
Focal signs of pathology
The disease is also characterized by focal symptoms. They depend on the location of the tumor:
- Upper cervical vertebra. The symptom is spastic tetraplegia. Pain appears in the cervical region and shoulder girdle.
- Lower cervical vertebra, first thoracic. Flaccid paralysis of the upper limbs is diagnosed. Lower - spastic paralysis. At a late stage of the disease, pelvic disorders appear.
- Thoracic department. Symptoms are girdling pain, fecal and urinary incontinence. Spastic paralysis of the lower limbs.
- Lumbar region. Signs: paralysis (flaccid or spastic), dysfunction of the pelvic region.
- Sacral area - pain in the posterior surface of the lower extremities. The flexor muscles are paralyzed. Pelvic disorders are observed. Bedsores appear in the sacrum area.
- Cauda equina area - severe pain in the legs, lack of reflexes, development of paralysis. Bedsores also appear. The process of urination occurs with a delay.
In all of the above cases, impaired sensitivity is associated with the nature of the damage.
Types of tumors and features of their development ↑
There are many classifications of spinal tumors based on a variety of criteria.
From a clinical point of view, in terms of assessing the severity of the patient’s condition, determining the prognosis for life and treatment tactics, one of the most important classifications is the division of tumors into malignant and benign.
Benign
The main characteristics of benign tumors:
- Availability of capsule.
- Tumor growth with an increase in size and compression of surrounding tissues.
- Tumor cells are highly differentiated and rarely divide.
- Tumor growth is usually slow.
- There are no metastases.
Most benign tumors have a good prognosis, respond fairly well to treatment, and can be completely eliminated through surgery.
However, if the tumor is localized on the spine, various difficulties in treatment often arise due to the location of the space-occupying lesion near the spinal cord, nerve roots, and large vessels.
Malignant
Main characteristics of malignant tumors:
- They do not have capsules.
- Infiltrating growth is the growth of a tumor into neighboring organs and tissues.
- Tumor cells are undifferentiated and divide frequently.
- The tumor is growing rapidly.
- There are metastases - with the flow of blood and lymph, tumor cells penetrate into other, even distant organs, “attach” and begin to divide - more tumors are formed.
Due to the characteristics of their growth and development, malignant tumors are very difficult to treat, especially in the later stages, when there are multiple metastases to other organs.
In addition to dividing into malignant and benign, tumors of the spinal column are divided into primary and secondary.
Primary tumors initially develop on the spine, and secondary tumors are metastases of cancer in another location.
It is clear that with metastases, complete treatment will require the elimination of not only the formation on the spine, but also the impact on the primary focus.
Secondary cancer tumors also include degenerated, initially benign tumors and malignancy (cancerous degeneration) of non-tumor lesions of the spine.
The most common spinal tumors are:
Osteoma
Benign tumor of bone tissue. It grows very slowly, so it remains asymptomatic for a long time.
When it reaches a large size, pain occurs; the tumor causes deformation of the spine, compression of the spinal cord and nerve fibers.
Photo: osteoma in the picture
Osteochondroma
A benign tumor of bone and cartilage tissue, which, however, can become malignant.
Due to slow growth, symptoms increase gradually.
Photo: osteochondroma
Osteoid osteoma
A small (less than one centimeter) tumor that most often affects teenagers and young men.
Characterized by intense, constant pain that gets worse at night.
The pain syndrome is relieved briefly with painkillers, but is quite well controlled by aspirin and its derivatives.
Another typical symptom is spasm of the paravertebral (running along the spinal column) muscles, which is accompanied by the development of scoliosis.
Larger osteoid osteomas of the spine are less common.
Photo: vertebral osteoid osteoma
With them, the pain syndrome is less pronounced, but their growth into the spinal canal causes compression of the spinal cord and roots with the development of corresponding neurological symptoms.
Hemangiomas
Vascular benign tumors, mostly congenital, resulting from intrauterine development disorders.
In women, hemangiomas are found 2 times more often than in men.
Hemangioma is usually localized in the vertebral body, and on x-ray it manifests itself with specific symptoms of “honeycomb” (multiple foci of bone destruction) and “bloating” of the affected vertebra.
Diagnostics
The first step to determining a diagnosis is collecting complaints and medical history. The next manipulation is conducting a neurological examination and collecting examination data. Classic diagnosis is radiography. It is believed that this method does not provide all the necessary information to diagnose the disease. Especially at an early stage of the disease. Thanks to it, it is impossible to determine whether changes are occurring in soft tissues. At an advanced stage, an x-ray shows the presence of destruction and displacement of the vertebrae. More accurate results are obtained with lumbar puncture using special samples. Then the cerebrospinal fluid is checked.
Queckenstedt test - this method determines the patency of the subarachnoid space of the spinal cord. It is based on changes in spinal fluid pressure when the jugular veins are compressed.
- Positive test - the pressure of the cerebrospinal fluid does not change. It doesn't leak. Pain appears. It is caused by its introduction into the neoplasm with a puncture needle. Patency is impaired.
- Negative – fluid pressure increases. The patency of the spinal cord space is normal.
Tumor cells in the cerebrospinal fluid appear very rarely. The most information about the disease can be obtained during magnetic resonance imaging of the spine. Thanks to this procedure, the location and size of the malignant neoplasm in relation to bone and tissue structures is assessed. If magnetic resonance imaging is not possible, the patient is referred for contrast myelography. It is used to determine the type and level of tumor location. Currently, pneumomyelography and isotope myelography are rarely performed. These procedures may cause complications. The diagnosis is confirmed only after receiving the results of histology of the neoplasm (after surgery).
Treatment of intramedullary tumors
According to statistics, about 85% of oncological tumors, including intramedullary tumors, are treatable. Tumors located in the spinal cord are operable. Surgical interventions have their consequences and risks, and operations do not always end well for the patient. However, if cancer is detected at an early stage of development, radical methods can be avoided in the fight against it. This is where various therapy techniques come to the rescue.
Ultrasonic aspiration
It involves intense exposure of the affected area to a laser beam, which helps destroy cancer cells without surgery. The advantage of the method is the absence of side effects that could seriously harm the patient’s health.
Radiation therapy
The technique is usually used after ultrasound aspiration or surgery to remove remaining cancer cells in the body. Consists in the use of radioactive radiation. Radiation therapy may be used in cases where the tumor is inoperable or cannot be reached by surgery, or if secondary tumors need to be removed. The procedure can cause significant negative side effects. However, the benefits of such treatment outweigh the risks that cancer entails.
Chemotherapy
Today this is the most common type of treatment for malignant tumors. The therapy uses chemicals that act on cancer cells and prevent them from developing. Unfortunately, the method also has negative side effects.
Stereotactic radiotherapy
This procedure is an innovative way to treat malignant tumors. The method is used for patients who cannot be operated on due to the location or size of the tumor. Stereotactic radiotherapy involves targeted distribution of gamma radiation to cancer cells. The procedure helps destroy the formation without affecting healthy tissue. Gamma radiation can penetrate and damage the DNA of cancer cells, preventing the tumor from spreading and eventually destroying it.
Choose treatment
Treatment and expected results
Radical surgery is most often impossible to perform. The reason is the germination of surrounding tissues. The method of treatment depends on the clinical signs. The patient is prescribed chemotherapy and radiation therapy. Corticosteroids reduce the inflammatory response and reduce pressure on nerve tissue. If severe compression of the spinal cord occurs, surgical decompression is performed. The tumor is partially removed or excised.
For severe pain, surgery is performed. The spinothalamic tract or nerve root is cut. The prognosis for this diagnosis is unfavorable. Full recovery, most often, does not occur. Treatment improves a person's quality of life. Thanks to it, symptoms are reduced. Life expectancy depends on the type and degree of tumor development. On the effectiveness of chemotherapy and radiation therapy.
Forecast
Growth parameters and tumor characteristics determine the prognosis of spinal neoplasms. Even successful surgery to remove a tumor does not guarantee that there will be no relapse or continued development of the tumor.
Ependymomas have a favorable prognosis because many patients do not experience recurrence of the disease for many years after surgery.
The prognosis of astrocytoma is not so favorable, since almost 50% of all patients experience relapses within 4-5 years after surgery.
On this topic
- central nervous system
What threatens a cyst in the head?
- Olga Vladimirovna Khazova
- February 28, 2020
If we talk about teratomas, they have an unfavorable prognosis: after a short period of time, the patient may develop systemic metastases. The same applies to metastatic intramedullary neoplasms, the prognosis of which in most cases does not inspire much hope.
Depending on the start of surgical treatment and the severity of the clinical picture, the level of recovery of the neurological deficit may vary. This process is also influenced by the quality of rehabilitation treatment.
There are many cases in medicine where timely and high-quality surgery to remove a tumor allows patients to return to a full life and work activity after a long rehabilitation period.