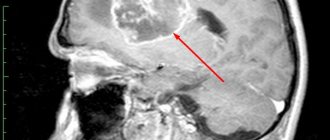
Brain puncture is a multi-purpose medical manipulation, with the help of which one or more therapeutic and diagnostic purposes are pursued. A puncture (injection) is any penetration with a needle or trocar into the cavity of a vein, another vessel, or an organ, to obtain material for research and diagnosis, optimize functions and remove obstacles, and perform operations. Modern techniques make it possible to combine operational and diagnostic goals, achieving them simultaneously.
Taking fluid for analysis does not exclude the use of other diagnostic methods. Modern technologies allow parallel ultrasound to determine the location of the dislocation, for example, a cyst. This combination can successfully remove the tumor.
There is no need to be afraid of a puncture - it is not only a diagnostic method, but also a treatment method that was used before, but in an indirect form.
What is a cerebral puncture?
Penetration into the cranium at the location of parts of the brain is carried out less frequently than other manipulations in places that are less dangerous and threaten negative consequences. Although any puncture can cause complications if it is carried out unprofessionally, affects some important segments or becomes a source of infection. Each invasive procedure has features specific to a particular department, developed techniques and precautions.
Brain puncture (cerebral puncture) is a collective name for a therapeutic or diagnostic procedure carried out according to indications at a strictly defined destination:
- in the lower parts of the temporal or frontal lobes;
- over the tympanic space or mastoid process;
- ventricular, in the region of the lateral ventricles;
- within the central nervous system, to obtain a sample to study the spinal cord and brain simultaneously.
To carry out the procedure, a special needle and scalpel are used, the trepanation window is cut out with a special cutter, and bone bleeding is stopped by rubbing wax or electrocoagulation. To regulate the flow of cerebrospinal fluid there is a special device - a mandrin. In most cases, the procedure is performed under local anesthesia, in compliance with all necessary conditions of sterility and preparation of a sterile surgical field.
However, just in case, a large operating room is being prepared, which in rare cases can be used to perform open brain surgery. This scenario is possible when surgical complications arise - damage to a vessel, air entering the cavity, or insertion of a needle to an unexpected height.
Although sometimes the reason for further surgical tactics is an insufficiently studied pathology located directly in the brain (abscess, abscess, cyst, neoplasm).
Why puncture for stroke?
A puncture of cerebrospinal fluid in medical terminology is designated as a lumbar puncture, and the fluid itself is called cerebrospinal fluid. Lumbar puncture is one of the most complex methods that has diagnostic, anesthetic and therapeutic purposes.
The procedure involves inserting a special sterile needle (length up to 6 cm) between the 3rd and 4th vertebrae under the arachnoid membrane of the spinal cord, and the brain itself is not affected at all, and then extracting a certain dose of cerebrospinal fluid.
A spinal tap is most often used when central nervous system infections such as meningitis and encephalitis are suspected. Multiple sclerosis is very difficult to diagnose, so a lumbar puncture is indispensable. As a result of the puncture, the cerebrospinal fluid is examined for the presence of antibodies.
With the use of lumbar puncture, diagnosis helps to detect inflammation of the brain, subarachnoid bleeding or detect herniated intervertebral discs by injecting a contrast agent, as well as measure the pressure of the spinal cord fluid. In addition to collecting fluid for research, specialists also pay attention to the rate of leakage, i.e.
if one clear drop appears in one second, the patient has no problems in that area.
In medical practice, spinal cord puncture, the consequences of which can sometimes be very serious, is prescribed in order to remove excess cerebrospinal fluid and thereby reduce intracranial pressure in benign hypertension, and is carried out to administer medications for various diseases, for example, chronic normal pressure hydrocephalus.
• dropsy with a space-occupying lesion in the temporal or frontal lobe;
• infringement of the brain stem;
• bedsores of the lumbosacral area;
• skin and subcutaneous infections in the lumbar region;
• extremely serious condition of the patient.
In any case, the doctor first conducts a series of tests to ensure that there is an urgent need for a spinal cord puncture. Its consequences, as already noted, can be very, very serious, since the procedure is risky and involves certain risks.
Contraindications to spinal cord puncture
Performing a spinal tap
Collecting a small amount of cerebrospinal fluid (CSF).
Subsequently, their histology is carried out; measuring the pressure of cerebrospinal fluid in the spinal canal; removing excess cerebrospinal fluid; introducing drugs into the spinal canal; facilitating difficult labor in order to prevent painful shock, as well as as anesthesia before surgery; determining the nature of the stroke; discharge tumor markers; cisternography and myelography.
Bacterial, fungal and viral infections (meningitis, encephalitis, syphilis, arachnoiditis); subarachnoid bleeding (hemorrhages in the brain); malignant tumors of the brain and spinal cord; inflammatory conditions of the nervous system (Guillain-Barre syndrome, multiple sclerosis); autoimmune and dystrophic processes.
Often a spinal tap is equated with a bone marrow biopsy, but this statement is not entirely correct. During a biopsy, a tissue sample is taken for further research.
Access to the bone marrow is achieved through a puncture of the sternum. This method allows you to identify bone marrow pathologies, some blood diseases (anemia, leukocytosis and others), as well as metastases in the bone marrow.
In some cases, a biopsy can be performed during the puncture process.
Spinal cord puncture is mandatory for infectious diseases, hemorrhages, and malignant neoplasms.
Inflammatory polyneuropathy; fever of unknown pathogenesis; demyelinating diseases (multiple sclerosis); systemic connective tissue diseases.
Before the procedure, medical workers explain to the patient why the puncture is being performed, how to behave during the procedure, how to prepare for it, as well as possible risks and complications.
Registration of written consent for the manipulation. Taking blood tests to evaluate blood clotting, as well as the functioning of the kidneys and liver. Hydrocephalus and some other diseases require computed tomography and MRI of the brain. Collection of information on the medical history, recent and chronic pathological processes.
The specialist must be informed about the medications the patient is taking, especially those that thin the blood (Warfarin, Heparin), relieve pain, or have an anti-inflammatory effect (Aspirin, Ibuprofen). The doctor should be aware of existing allergic reactions caused by local anesthetics, anesthesia drugs, iodine-containing agents (Novocaine, Lidocaine, iodine, alcohol), as well as contrast agents.
It is necessary to stop taking blood thinning drugs, as well as analgesics and non-steroidal anti-inflammatory drugs in advance.
Before the procedure, water and food are not consumed for 12 hours.
Women must provide information about their suspected pregnancy. This information is necessary due to the expected x-ray examination during the procedure and the use of anesthetics, which may have an undesirable effect on the unborn child.
Your doctor may prescribe a medication to take before the procedure.
The presence of a person who will be next to the patient is mandatory. A child is allowed to undergo a spinal puncture in the presence of his mother or father.
A spinal cord puncture is performed in a hospital ward or treatment room. Before the procedure, the patient empties his bladder and changes into hospital clothes.
Spinal cord puncture
The patient lies on his side, bends his legs and presses them to his stomach. The neck should also be in a bent position, with the chin pressed to the chest. In some cases, spinal puncture is performed with the patient sitting. The back should be as motionless as possible.
The skin in the puncture area is cleaned of hair, disinfected and covered with a sterile napkin.
The specialist may use general anesthesia or use a local anesthetic. In some cases, a drug with a sedative effect may be used. Also during the procedure, heartbeat, pulse and blood pressure are monitored.
The histological structure of the spinal cord provides for the safest needle insertion between the 3rd and 4th or 4th and 5th lumbar vertebrae. Fluoroscopy allows you to display a video image on a monitor and monitor the manipulation process.
Next, the specialist collects cerebrospinal fluid for further research, removes excess cerebrospinal fluid or injects the necessary drug. The liquid is released without outside help and fills the test tube drop by drop. Next, the needle is removed and the skin is covered with a bandage.
CSF samples are sent for laboratory testing, where histology occurs directly.
Spinal cord cerebrospinal fluid
The doctor begins to draw conclusions based on the nature of the fluid coming out and its appearance. In its normal state, the cerebrospinal fluid is transparent and flows out one drop per second.
Maintaining bed rest for 3 to 5 days as recommended by a doctor; keeping the body in a horizontal position for at least three hours; avoiding physical activity.
When the puncture site is very painful, you can resort to painkillers.
Axial herniation; meningism (symptoms of meningitis occur in the absence of an inflammatory process); infectious diseases of the central nervous system; severe headache, nausea, vomiting, dizziness. The head may hurt for several days; damage to the roots of the spinal cord; bleeding; intervertebral hernia; epidermoid cyst; meningeal reaction.
If the consequences of the puncture are expressed in chills, numbness, fever, a feeling of tightness in the neck, or discharge at the puncture site, you should immediately consult a doctor.
There is an opinion that during a spinal tap the spinal cord can be damaged. It is erroneous, since the spinal cord is located higher than the lumbar spine, where the puncture is directly made.
Spinal cord puncture, like many research methods, has contraindications. Puncture is prohibited in case of sharply increased intracranial pressure, dropsy or cerebral edema, or the presence of various formations in the brain.
It is not recommended to take a puncture if there are pustular rashes in the lumbar region, pregnancy, impaired blood clotting, taking blood thinning drugs, or ruptured aneurysms of the brain or spinal cord.
In each individual case, the doctor must analyze in detail the risk of the manipulation and its consequences for the life and health of the patient.
It is advisable to contact an experienced doctor who will not only explain in detail why it is necessary to perform a spinal cord puncture, but will also carry out the procedure with minimal risk to the patient’s health.
What is it done for - diagnostic and therapeutic purposes
Obtaining cerebrospinal fluid to determine treatment tactics, analysis and diagnostic prognosis is carried out with the goal of achieving a certain result, and before prescribing a puncture, the tasks are strictly delimited. However, there are situations when a cerebral puncture for the purpose of research, collection of cerebrospinal fluid, as material for diagnostics, turns into shunting or removal of excess fluid to reduce pressure inside the skull.
Ventricular puncture (penetration into the lateral ventricles of the brain) helps doctors achieve several goals:
- performing diagnostics by obtaining important biological fluid for research;
- measuring intracranial pressure or conducting studies with a radiopaque substance;
- operations performed using a special device - a ventriculoscope, or shunting in the cerebrospinal fluid system;
- reducing intracranial pressure by removing spinal fluid if the natural outflow system does not work.
Well-established techniques and precautions allow operations to be performed as needed, using only local anesthesia. The methods and routes of penetration have been developed over many years of practice, and the data obtained in most cases helps to carry out more effective treatment based on objective information.
Is it dangerous to do a puncture?
For diseases or damage to organs and nerves of the central and peripheral nervous systems, specific examinations may be required. These include spinal cord puncture. In what cases is this procedure performed, why is it done, and is it dangerous?
Preparation for puncture
Before collecting cerebrospinal fluid for analysis, it is necessary to conduct an examination:
- pass general and biochemical blood and urine tests;
- do a blood coagulogram;
- change fundus pressure and intracranial pressure;
- for neurological disorders, cerebral signs indicating dislocations - CT or MRI of the brain;
- other tests prescribed by your doctor.
Source: https://prodyhanie.ru/opasno-li-delat-punkciju/
How to take a brain puncture
The operation is carried out under local anesthesia with strict adherence to all the rules of sanitary processing, first the incision, and then cutting the bone with a special tool, after which cerebrospinal fluid begins to flow through the hole, which is taken to alleviate the patient’s condition and conduct tests.
The surgical field is limited to sterile tissue, and the outflow of biological fluid is strictly controlled, as well as possible bleeding when a burr hole appears.
It is necessary to take into account all indications and contraindications, possible obstacles to the operation. Thorough sanitization at each stage, preparation of spare instruments, a large operating room, careful monitoring of the patient’s condition at each stage.
Mandrin and other instruments must be thoroughly disinfected
The manipulation is carried out with the patient positioned on his back, with his head bowed to his chest. The neurosurgeon determines the incision line by touch.
There is a method of penetration through the orbit (the so-called Dogliotti method), and there is another method - according to Germanovich, who developed penetration through the temporal bone from below.
Indications for lumbar puncture of cerebrospinal fluid.
- Traumatic and non-traumatic subarachnoid hemorrhage. In this case, spinal puncture is the single most reliable research method, since after three days a CT scan may not detect SAH. In addition to the diagnostic purpose, there is also a therapeutic one - the sanitation of cerebrospinal fluid from spilled blood and toxic products of its decay.
- Inflammatory diseases of the brain: meningitis, encephalitis, myelitis, arachnoiditis.
- Spontaneous, traumatic or postoperative liquorrhea. The goal is to reduce cerebrospinal fluid pressure and create conditions for self-closure of the cerebrospinal fluid fistula, as well as eliminate the inflammatory process.
- The need to administer antibacterial drugs directly into the cerebrospinal fluid in case of infection of the brain or spinal cord and their membranes.
- TAP-TEST is performed to determine the indications for shunt surgery for non-occlusive hydrocephalus. Approximately 30-50 ml of cerebrospinal fluid is excreted. If after this there is a temporary improvement in the patient’s condition, the test is considered positive.
Doctor's competence
Taking biological fluid for analysis or to alleviate the patient’s condition is considered a surgical intervention of a high degree of complexity. The procedure is the responsibility of the neurosurgeon and anesthesiologist. The first one must certainly have extensive practical experience in order to transfer the process from puncture to open brain surgery in case of complications.
No one is immune from errors or complications during the operation. The result may be bleeding and hematoma, damage to the brain substance itself or its vessels, displacement of brain structures or rapid swelling.
Risks and consequences of a spinal tap
Complications after puncture occur primarily when the rules of manipulation are not followed and doctors make mistakes. In other cases, the following consequences may occur:
- wedging of individual structural elements of the brain;
- dislocation of midbrain structures;
- damage to nerve endings causing pain in the patient;
- headaches, nausea, vomiting;
- hematomas at the site of needle insertion when small capillaries are damaged.
When taking cerebrospinal fluid material from pregnant women, the risk of spontaneous abortion increases, especially in the first third. Patients suffering from cardiovascular diseases also represent a risk group during manipulation. In particularly serious cases, the launch of vasovagal processes can provoke cardiac and respiratory arrest.
Contrary to popular belief that puncture can lead to paralysis, this complication is unlikely. The needle is inserted into the part of the spine that is most poorly innervated and the risk of damage to nerve endings is very low. The incidence of complications after puncture in patients does not exceed 1%.
After two weeks of intensive treatment, the patient’s health condition and the effectiveness of the chosen therapy method are assessed. To do this, repeat manipulation is performed with the collection of spinal fluid material for research. Based on the results of the puncture, changes in the cellular composition are analyzed and the presence or absence of a bacterial culture in the contents is determined. Positive dynamics indicate the patient’s clinical recovery.
Meningitis is a serious disease that requires accurate identification of the causative agent of the infection and the appointment of competent treatment. Cerebrospinal fluid puncture is the only and reliable method for diagnosing the disease.
Cost in Russia
In Moscow, the price of the procedure starts from 5 thousand rubles, and can increase, depending on the prestige of the clinic and the luminaries of world medicine working in it. In the provinces, prices are significantly lower, but the complexity of the procedure and the responsibility of the surgeon suggest that this category of interventions is not cheap.
For many, brain puncture is subconsciously considered dangerous, but in fact it is not. If performed by an experienced doctor, it is absolutely safe. It is thanks to it that it is possible to detect ulcers in brain tissue, determine the contents of neoplasms and the state of other pathologies.
But there are also a number of dangers that can be encountered with this procedure. Let's figure it out.
Frequency of pain after puncture
In the late 19th century, when the spinal anesthetic technique was first used, the incidence was over 60%. This was due to the use of imperfect instruments that left too large a hole at the piercing site. Over time, the incidence of headaches after spinal anesthesia decreased. Today, this post-puncture side effect occurs in 1 case out of 100.
Pain after spinal anesthesia can be a complication of inadvertent puncture of the dura and arachnoid membranes. This is a rare phenomenon, occurring in 3% of cases.
Interesting: Headache after a long sleep: causes, prevention, treatment
Complications: how to avoid
The puncture is performed with a special needle, which, penetrating the brain tissue, can draw fluid from it. To make a puncture safe, you need to follow a number of rules:
- The area of the head where the puncture will be made must be thoroughly disinfected. First, it is treated with hydrogen peroxide, and then generously lubricated with iodine.
- For the procedure, you cannot use a regular needle, only a special puncture needle with a blunt end. It is produced quite wide and equipped with a mandrel.
- There should be 2 needles, one of which will be a spare if the first one is blocked by brain tissue.
- The puncture should be made to a depth of no more than 4 cm. This is the only way to ensure the safety of the fence and prevent the penetration of purulent secretions into the cerebral ventricles.
- Before the procedure, the patient must have a bowel movement.
- The patient must be completely immobile, so he can be fixed with special devices.
Technique
Most often, puncture of the anterior or posterior horn of the lateral ventricle is performed.
When puncturing the anterior horn of the lateral ventricle, a linear soft tissue incision about 4 cm long is made. The edges of the skin are separated using a Jansen retractor. A burr hole is placed at Kocher's point, which should be located 2 cm anterior to the coronal suture and 2 cm lateral to the midline of the sagittal suture. The dura mater is opened crosswise and a cannula is inserted into the brain for ventriculopuncture. The cannula is advanced parallel to the sagittal plane in the direction of the internal auditory canal. Normally, in adults, the anterior horn is located at a depth of 5-5.5 cm. With hydrocephalus, this distance can be significantly reduced. To puncture the posterior horn, a burr hole is placed at the Dandy point 3 cm lateral and 3 cm above the external occipital protuberance. The cannulas are immersed into the brain in the direction of the upper outer edge of the orbit. Normally, the posterior horn is located at a depth of 6-7 cm.
Areas of application, indications, contraindications
Such a study is carried out in areas where there is suspicion of pus formation, most often these are:
- lower part of the frontal lobe;
- inferior part of the temporal lobe;
- tympanic space;
- near the mastoid process.

A puncture is taken to diagnose brain pathologies, such as:
- infectious lesion of the central nervous system;
- inflammatory process in the central nervous system;
- bacterial, viral, fungal diseases;
- infection of brain tissue with tuberculosis or syphilis;
- bleeding of subarachnoid type;
- stroke of any type;
- skull injuries;
- multiple sclerosis;
- neoplasms of any type;
- neuralgic pathologies;
- swelling of brain tissue;
- problems with the vascular system.
Important! Before the procedure, the patient must indicate in a special questionnaire a list of medications that he is currently taking, whether he is allergic to anesthetics or medications, and whether he has problems with blood clotting.
The procedure is prohibited if:
- the patient is at any stage of pregnancy;
- he is in a state of traumatic shock;
- lost a lot of blood;
- there are intracranial hematomas;
- brain abscess diagnosed;
- there is extensive cerebral edema;
- diagnosed with hypertension;
- there are abundant infectious and purulent lesions on the back;
- there are lumbar bedsores;
- the brain is injured.
Risk factors for headaches after puncture
The risk of developing post-puncture headache is due to the influence of a number of factors. Some of them are related to the patient’s health, others are the result of the doctor’s professional incompetence or the use of low-quality instruments.
Risk factors depending on the patient's health
The individual characteristics of the patient’s body can provoke the development of post-puncture complications. The doctor pays attention to:
- age;
- gender;
- body weight;
- history of headaches;
- position of the patient during puncture.
Risk factors depending on the doctor and the needle
The occurrence of post-puncture headache after anesthesia may be associated with the peculiarities of the procedure and the use of instruments. The caliber of the needle and the type of its tip are taken into account.
Among the factors that depend on the doctor are the following:
- the access chosen for the puncture,
- slice orientation;
- use of mandrel instruments, which are the least invasive;
- avoiding repeated anesthetic procedures.
Needle diameter
The diameter of the needle used to pierce is directly related to the appearance of cephalgia. The larger it is, the more likely it is that you will have a headache after the puncture.
Other factors also influence the occurrence of side effects:
- quality of puncture needles;
- needle design;
- technical difficulties during spinal tap;
- location of the needle cut during puncture;
- composition of the solution administered subarachnoidally;
- method of removing the needle;
- access from which the puncture is performed.
How to carry out the procedure
Why the procedure is being done has been determined, now you need to understand the methods for carrying it out. They are different and directly depend on the area where the liquid is taken.

The ventricular procedure for this area is performed as follows:
- The patient lies on his back when a tumor in the brain is to be identified. Usually the patient lies down on the healthy side to make it more convenient for the doctor to perform a puncture on the injured side.
- The head is slightly tilted towards the chest.
- The puncture site is thoroughly disinfected and coated with iodine twice.
- Draw a puncture line, which should be guided by the arrow-shaped seam, passing the Kocher point. It is covered with a layer of brilliant green solution.
- The head is covered with a sterile sheet.
- Any local anesthetic to which the patient is not allergic is used to numb the puncture area, most often it is Novocain.
- Using a scalpel, an incision is made along the intended line.
- A cut is made on the trepanation window on the exposed skull.
- The neurosurgeon makes a cross-shaped incision on the dura mater. Wax is rubbed in or electrocoagulation is performed. For what? To stop bleeding, the latter method being the most effective.
- The cannula is inserted into the brain tissue to a depth of no more than 5-6 cm so that it runs parallel to the incision line. When puncturing the wall of the lateral ventricle, the doctor will feel a slight dip.
- Yellowish cerebrospinal fluid will begin to flow through the submerged cannula. Having penetrated the cavity of the ventricle, the doctor fixes the needle and, using a mandrel, regulates the volume and speed of the withdrawn fluid.
Important! Rapid collection of cerebrospinal fluid is strictly prohibited. This must be done drop by drop.
Often there is high pressure in the ventricular cavity, and if it is not controlled, the fluid will flow out in a stream. This will lead to the patient developing neuralgic problems.
The permissible volume of fluid intake is in the range of 3-5 ml. It is important to note that in parallel with the preparation of the room for the puncture, the operating room is also prepared, since there is a high risk that air may enter the area being examined, or the depth of the puncture will be excessive, which may cause injury to the blood vessel. In these cases, the patient will be urgently operated on.

In cases of puncture, children use the methods of collecting cerebrospinal fluid according to Dogliotti and Geimanovich:
- In the first case, the puncture is carried out through the orbit.
- In the second - through the lower part of the temporal bone.
Both of these options have a significant difference from the traditional procedure - they can be repeated as often as necessary. For infants, this procedure is carried out through an open fontanel, simply by cutting the skin above it. In this case, there is a serious danger that the baby will develop a fistula.
The technology for collecting cerebrospinal fluid from the area is carried out in the following order:
- The patient lies on his stomach. His head is tightly fixed so that the sagittal suture is strictly in the middle cavity.
- The preparatory process is identical to the above procedure.
- The incision of the skull tissue is carried out parallel to the sagittal suture, but so that it passes through the Dandy point, which should be strictly in its middle.
- Take a needle number 18, which is used strictly for this type of puncture.
- It is inserted at an angle, directing the needle tip into the outer upper edge of the orbit to a depth of no more than 7 cm. If the procedure is performed on a child, the puncture depth should not exceed 3 cm.
Clinical picture after the procedure
Of course, the symptoms after puncture sampling are different for everyone, but they can be combined into a general clinical picture:
- Pain in the head area of varying intensity and duration.
- Prolonged nausea and vomiting.
- Convulsions and fainting.
- Malfunction of the cardiovascular system.
- Impaired respiratory function; in rare cases, the patient may need artificial ventilation.
- Neuralgic problems.
Whether the patient will have the above symptoms directly depends on the experience of the neurosurgeon and his skills. The procedure must be performed strictly according to medical instructions, which can guarantee the absence of complications after the puncture.
It is important not only to correctly fix the patient, but also to accurately determine the puncture area. Treatment of the affected area is important both at the stage of preparation for the procedure and after it. Upon completion of the collection, be sure to apply a sterile bandage.
It is important that the patient does not feel any discomfort, much less pain, at the time of the puncture.
Due to the fact that the procedure is most often prescribed for diagnosing pathologies, it, like any other diagnostic measure, should be painless. The patient will be conscious at all times, so he should immediately inform the doctor about any discomfort that has arisen. This will help avoid a number of complications. The doctor will change the technology or completely interrupt the procedure.
Puncture is an important procedure in medicine, and taking cerebrospinal fluid from the brain is even more important. Before undergoing it, the patient will undergo a series of studies that will help identify possible contraindications. There is no need to worry; brain puncture is performed only by experienced specialists who know their job.
Puncture of the ventricles of the brain (ventriculopuncture) is performed for diagnostic and therapeutic purposes. Puncture of the cerebral ventricles becomes especially important for the patient when providing emergency assistance during a hypertensive-hydrocephalic crisis, being often the only measure that allows the patient to be brought out of a serious condition. There are no contraindications for ventricular puncture, with the exception of bilateral tumors of the cerebral ventricles.
The anterior and posterior horns of the juice ventricles are most often punctured; the lower horns are rarely punctured.
Puncture of the temporal horns of the lateral ventricles is performed when puncture of the anterior and posterior horns is unsuccessful or during surgery in the temporal region of the brain, as a stage.
The patient is prepared for puncture of the lateral ventricle of the brain (if it is not done on an emergency basis) as for an operation: they give a cleansing enema the night before, take a hygienic bath, shave their head bald the day before or on the day of the operation, and do not feed or drink in the morning on the day of the examination.
Puncture of the ventricles of the brain is performed under local anesthesia with 30 ml of 2% novocaine solution.
Treatment of post-puncture headache
In the treatment of post-puncture headache, it is necessary to take into account the solution of the following problems: increase the production of cerebrospinal fluid and reduce its exit through the remaining excision in the meninges. For this purpose, various methods of therapy are used. The choice of technique depends on the severity of the complication, the age of the patient, and the clinical picture of the pathology.
Interesting: Headache from bright light: causes and treatment of photophobia
Treatment algorithm
It is important to follow a set of therapeutic measures. By following your doctor's recommendations, you can get rid of unpleasant symptoms. The patient must remain in bed.
Infusion treatment is prescribed when medications are administered intravenously. Analgesics and caffeine-based medications have a therapeutic effect.
If the patient's condition does not change, the technique of epidural filling with autologous blood is used.
Drug treatment
In the absence of contraindications and the severity of the disease, drug therapy is used. It consists of the use of medicinal solutions administered orally by injection. The volume of saline solutions is determined individually. Adding caffeine helps relieve symptoms in 85% of cases.
Filling the epidural space with autologous blood
When conservative treatment is ineffective, the method of epidural filling with autologous blood is used. Up to 20 ml of autologous blood is injected into the epidural space at the level where the cut was placed. It closes the defect in the membrane and prevents the cerebrospinal fluid from escaping. The pressure in the epidural space increases and eliminates pain. Over time, the autologous blood dissolves.
Links
Wikimedia Foundation. 2010.
- Ventry
- Vyanta eldership
See what “Ventricular puncture” is in other dictionaries:
- PUNCTURE
- (punctio), puncture of the cavity with a syringe containing diagnostic or therapeutic. purpose. P. is used for emptying various kinds of liquids and gases from tissues and cavities (emptying P.), determining their presence (test P.), for bacterial, chemical. And… …
ventricular puncture
- (p. ventricularis) P. ventricles of the brain ... Big Medical Dictionary
Hydrocephalus
— Skull of a patient with hydrocephalus... Wikipedia
Intracranial hematoma
— Intracranial hematoma is a pathological formation that is a hematoma widespread within the cranial cavity. The incidence of intracranial hematomas is 12–13% of neurosurgical patients. Contents 1 Etiology 2 ... ... Wikipedia
HEART
- HEART. Contents: I. Comparative anatomy……….. 162 II. Anatomy and histology……….. 167 III. Comparative physiology………. 183 IV. Physiology………………. 188 V. Pathophysiology……………. 207 VI. Physiology, pat.... ...Big Medical Encyclopedia
Cerebrospinal fluid
— Pulsation of the cerebrospinal fluid during heartbeat Cerebrospinal fluid, cerebrospinal fluid (lat. liquor cerebrospinalis), cerebrospinal fluid is a fluid constantly circulating in the ventricles of the brain, cerebrospinal fluid... Wikipedia
HEART
- Rice. 1. The heart of various animals. Rice. 1. Heart of various animals: 1 - cattle (front view); 2 — horses (rear view); 3 — pigs (front view); 4 — sheep (rear view); 5 — dogs (left view); 6 —… … Veterinary encyclopedic dictionary
Brain puncture
is not a dangerous procedure.
It is carried out to detect abscesses in the brain.
complications are possible during a brain puncture This is an infection in the brain; vascular damage; penetration of pus into the ventricles of the brain.