A benign tumor that develops from vessels, blood or lymphatic, and also affects the skin and internal organs and has a cavity, is called cavernous angioma, or cavernoma. This disease is congenital, although occasionally it is acquired. Signs and symptoms vary, it all depends on the location. There are cases of a hidden course, when a cavernoma is discovered by chance, or after transition to a complicated stage, which is very dangerous. Therefore, it is important to carry out diagnostics at the first signs in order to detect the presence of this disease in time.
In this article you will learn how cavernous angioma is formed, what are the signs of its appearance and methods that will allow you to diagnose this disease, treat it and prevent the development of possible complications.
What is cavernous angioma?
cavernous angioma
Cavernous angioma is a benign tumor consisting of pathologically dilated blood vessels.
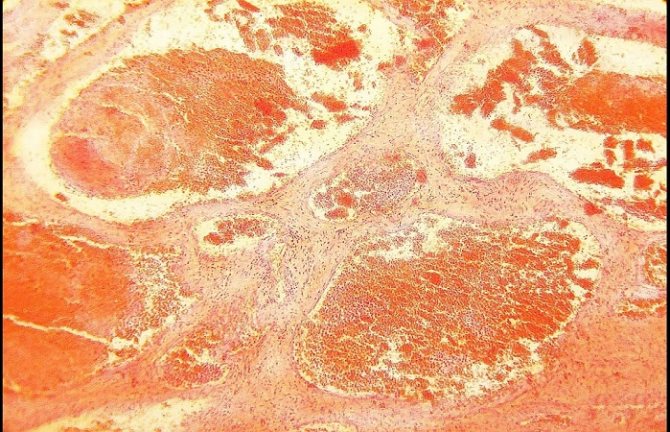
The distinctive features of cavernous angioma are the spongy structure of its walls. Neoplasms of this type are most often located subcutaneously and only occasionally in the depths of bone and muscle tissue. The most dangerous development of cavernous angioma is in brain tissue. Angiomas of the cavernous type have thin arteries that deliver blood to the cavity of the tumor, and thick veins that ensure its outflow. The tumor is soft and elastic when pressed. When compressed, it practically disappears and returns to its previous appearance after blood flow is restored. Cavernous angiomas are prone to bleeding, which explains the high frequency of their infection. In most patients, cavernous angiomas are congenital neoplasms. Their development is due to impaired tissue differentiation in the prenatal period. The onset of the tumor is given by fetal anastomoses connecting the arterial and venous beds.
As tumor vessels grow, the tumor increases in size. Occasionally, in the history of the occurrence of cavernous angiomas, there are indications of soft tissue injuries that served as an impetus for the occurrence of neoplasms of a vascular nature.
Cavernous angioma externally appears as a rounded neoplasm in the form of a spot, slightly elevated above the surface of the skin. Often the tumor is located in the tissues of the upper and lower extremities. The color of the spot varies from reddish to brown. A distinctive feature of angioma is its ability to undergo autonomous benign growth.
Symptoms of cavernous angioma include the following: Reduction in size or complete disappearance of the tumor when the limb is raised up and the tumor returns to its shape after lowering the arm or leg. Feeling of heaviness and discomfort in the limbs. Pain in the area of cavernous angioma, increased temperature of the skin above the surface of the angioma.
Neurological disorders in the area of cavernous angioma, the occurrence of epileptic seizures if the cavernoma is located in the brain tissue.
Examinations of patients suspected of having cavernous angiomas are carried out using the following diagnostic techniques: Radiography is highly informative in identifying cavernous angiomas of bone tissue. Angiography is a radiopaque research method that allows you to obtain accurate information about the structure of the bloodstream in a particular area of the body.
Ultrasound – helps in determining the depth of tumor spread, provides information about the structure and characteristics of the location of the tumor relative to other organs. CT, MRI – are used when it is necessary to examine vascular neoplasms of the central nervous system.
The goal of treating cavernous angioma is to stop its growth and eliminate tissues altered by the pathological process, followed by restoration of the normal structure of the vascular network. To achieve this goal, the following methods are used: Surgical treatment - used when the tumor lies in the deep layers of soft tissue.
Surgical treatment is most effective when it is possible to remove the tumor without damaging the healthy tissue located around it. Surgery is also used if angioma is detected in the later stages of development and there is no effect from the therapy.
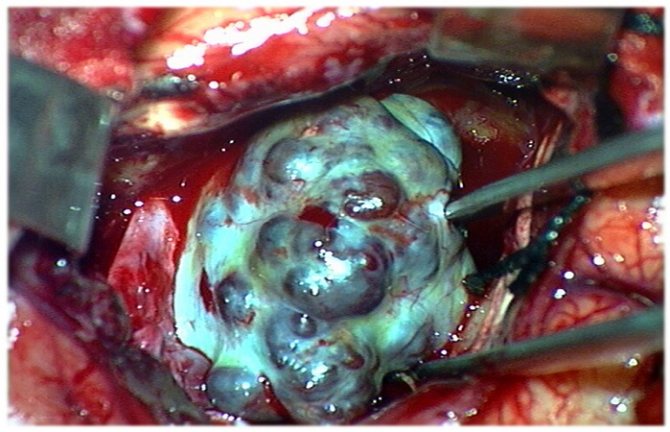
Surgical interventions for angiomas involve the use of complex microsurgical techniques that make it possible to work with even the smallest vessels. The accuracy of surgical intervention is of particular importance in the treatment of cavernous angiomas of the brain.
Microsurgical operations using stereotactic guidance devices provide the most radical removal of a tumor with a low risk of damage to healthy brain tissue. Laser therapy involves layer-by-layer removal of tumor tissue using light energy.
The main characteristics of this method are the low tendency of the wound to bleed and the minimal risk of scar formation, which makes it indispensable when it is necessary to treat angiomas of open areas of the body. Radiotherapy involves exposing the tumor to ionizing radiation, slowing down its growth and development.
Most often, radiation therapy for cavernous angiomas is carried out if they are located in such hard-to-reach anatomical areas as the retrobulbar space and the orbital cavity.
Diathermocoagulation - allows you to get good results in the treatment of small angiomas prone to bleeding. Diathermocoagulation allows you to gain access to even hard-to-reach tumors and remove them through the action of electric current energy.
Sclerotherapy - this technique is based on the introduction of sclerosing drugs into the cavity of the cavernous angioma. Such substances can cause the walls of the neoplasm to stick together, followed by collapse and emptying of the vessels. Sclerotherapy can significantly reduce the size of vascular tumors without surgical intervention.
Cryotherapy – removal of cavernous angioma in this case is carried out using liquid nitrogen. Hormonal therapy - the immunosuppressive and anti-inflammatory properties of hormonal drugs are used in the case of rapidly growing large angiomas affecting several anatomical areas at once.
Source: cancertreatments.ru
Treatment
The use of therapeutic methods to eliminate this kind of illness is pointless. Therefore, only surgical removal is used. But the operation can be complicated by the location of the tumor formation, or the patient’s refusal to perform it due to the absence of manifestations of the disease. Therefore, doctors try to perform surgery only in extreme cases when the following factors are present:
- The formation is located on the superficial layers and is also the cause of frequent seizures;
- The tumor is large and located in a critical area of the brain;
- If the pathology has already led to bleeding or hemorrhage.
When there is still a need for surgical treatment, the following types of surgery can be used:
- Removing the classic type. In this case, after the operation, compression of the brain structures is eliminated, due to which the symptoms that it caused also go away;
- Radiosurgery or gamma knife. In this case, the effect occurs directly on the pathology and other structures and tissues of the brain are not affected;
- Laser therapy. This method allows you to remove cavenous angioma layer by layer, due to laser exposure. The main positive side of this treatment is the low risk of scarring and bleeding. This makes it most popular in terms of treating pathologies that have a superficial location;
- Diathermocoagulation. It is often used to treat small and medium-sized formations that have a high tendency to bleed. The removal procedure is carried out using electric current;
- Cryotherapy. In this case, a procedure is performed to expose the tumor to liquid nitrogen. Due to this, it freezes out.
It is also possible to use non-surgical treatment methods, but only to prepare for surgery:
- Sclerotherapy. This method involves the need to inject special preparations into the cavity to glue it from the inside. This technique makes it possible to significantly reduce the size of the pathology without resorting to surgery;
- Hormonal therapy. It is necessary to stop the growth of the pathology and in some cases even allows you to reduce its size if the drugs have been selected correctly. This allows the formation to be stabilized before removal.
Drug therapy for cavernomas is not necessary. After all, this tumor is not malignant. In addition, this neoplasm does not respond in any way to radiation therapy or treatment with anticancer drugs.
The only treatment method is surgery. Before deciding whether to perform surgery, the doctor, together with the patient, weighs the pros and cons. If cavernomas are small and do not cause any symptoms, then there is no need for intervention, there is only a risk of consequences.
There are strictly defined indications for any operation, because this method of treatment is far from harmless, and sometimes very dangerous for life and prognosis.
- Hemorrhage localized outside the functional areas associated with a cavernoma.
- Epileptic seizures caused by cavernous hemangioma.
- Brain stem tumors.
- Cavernomas affecting functionally significant areas (according to MRI).
For different localizations of the neoplastic process, operations with different approaches are used as a treatment method. Decompensation of concomitant diseases is a relatively contraindication for surgical treatment. The possibility of performing the operation is assessed by a commission (by several doctors).
Brain cavernoma: causes, symptoms, treatment
- Hemorrhage localized outside the functional areas associated with a cavernoma.
- Epileptic seizures caused by cavernous hemangioma.
- Brain stem tumors.
- Cavernomas affecting functionally significant areas (according to MRI).
- the tumor provokes convulsions and epileptic seizures;
- is close to vital areas;
- provokes repeated hemorrhages and neurological disorders;
- located in a functionally significant area.
Brain cavernoma: causes, symptoms, treatment
Cavernous angioma cannot be treated with medication. Surgery is required - it is advisable to remove the tumor. But sometimes due to its location this is not possible. Also, the operation may not be performed if the patient is against the operation, since it does not cause him any inconvenience. The operation is not performed, but the risks remain, and the patient is under the supervision of a neurologist.
Surgery to remove a tumor is required if:
This takes into account such indicators as: the age and general health of the patient, the presence of concomitant diseases, the size and shape of the tumor, and others.
If surgical removal of the tumor is not possible, there are other removal methods besides the traditional one:
- radiosurgery - gamma knife (cyber knife). Used in case of difficult-to-reach location of the tumor. There is no risk of hemorrhage, the tumor is completely eliminated;
- laser therapy. Used to remove superficial cavities. The risk of bleeding and scarring is minimal;
- Diathermocoagulation is indicated if the tumor is small and there is a high risk of bleeding. Cauterization is carried out with alternating current;
- cryotherapy. Liquid nitrogen ablation is used to remove superficial tumors.
In addition to these methods, the following can be used:
- hormonal therapy. It is used for fast-growing tumors; this method is used to stop its growth or regression;
- sclerotherapy is the introduction of sclerosing drugs into the cavity, which causes its cells to stick together and decrease in size.
In each case, the decision to use one or another method to remove the tumor is made individually.
After surgery to remove a cavernoma, sessions of restorative procedures are necessarily carried out in order to introduce the patient to normal life as early as possible and avoid disability. An individual rehabilitation program is drawn up for each patient in accordance with his needs.
Types of angiomas
Depending on the characteristics, several types of angiomas are distinguished: Angioma in the form of red moles Angioma in the form of red moles Cavernous, or cavernous, are pulsating neoplasms with blood-filled cavities, the color of which can vary from dark red to purple.
In appearance, these are ordinary spots, somewhat raised above the skin. A distinctive property of the cavernous variety of angiomas is their spongy structure. The most common location of this tumor is the subcutaneous layer. In extremely rare cases, it can grow into muscle or bone tissue. Angioma has a soft and elastic structure; when pressed, it can be easily compressed, after which it quickly restores its shape. Cavernous tumors are prone to ulceration and bleeding, which create a favorable background for secondary infection.
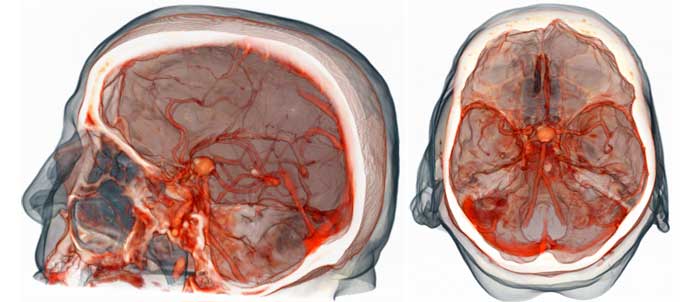
An increase in blood supply to the tumor can lead to a change in shape (mostly a significant increase) of the parts of the body on which it is located. Often the tumor is localized in the brain, mainly in the hemispheres, although it can also be located in the basal ganglia, brain stem or corpus callosum.
The brain type of angioma can lead to significant neurological disorders. Venous - also refers to benign formations. They can be different in size, prone to progressive autonomous growth. They are a combination of a large number of cavernous cavities with thin walls connected to each other.
The main location of venous angioma is: muscle tissue; subcutaneous fat; skin: brain. When located in the brain, angioma leads to dilation of the veins and can cause hemorrhage.
New growths come in different shades: from blue to brown. There are also: intraosseous variety - usually located on the cranial bones and can cause recurrent bleeding; branched form - develops extremely rarely, localized on the head, limbs, face. It consists of tangles of dilated branches of arteries or tortuous cords.
Source: lechimsya-prosto.ru
Health care
Depending on the type of venous angioma, treatment may consist of different blocks. For a benign tumor, the complex of medical care includes
- drugs to normalize blood circulation;
- sedatives and painkillers to stabilize the emotional state;
- surgical intervention (minimally invasive or extensive).
Surgical methods are used if the tumor is on the surface of the brain in a safe zone. These include all tumors on the surface of the brain, where access is not obstructed by adjacent tissues. Otherwise, they try to gain access to the tumor through the vessels themselves, since the risk of injury to the brain itself is less than with full-fledged invasion.
During the minimally invasive procedure, substances are introduced into the formation that block the flow of blood into pathologically growing vessels. This creates a new path for blood flow, bypassing the problematic blocked area.
The malignant nature of the tumor means unambiguous surgical excision and chemotherapy of a separate area of the brain.
Causes
The central nervous system can be a substrate for the emergence of a large number of different tumors: gliomas, astrocytomas, medulloblastomas. But in addition to neoplastic formations developing from cells of nervous tissue, the brain can be affected by a tumor of vascular origin, because the vascular bed supplies blood to all organs of the human body. Brain cavernoma is a dangerous disease. Hemangioma is a neoplasm of endothelial cells. It is usually associated with the general blood flow. Outwardly it looks like an expanded vascular formation, an aneurysm. Cavernous angioma (or cavernoma) is a type of vascular formation that consists of several vascular cavities with thin walls.
As a rule, these chambers have different sizes, sizes and volumes. But their main characteristic is that they are clearly demarcated from the brain parenchyma surrounding them. Cavernous hemangioma is a tumor that does not have a clear organic and functional connection with the general blood flow.
However, next to it there is usually an artery or vein, usually also deformed like an aneurysm. It is she who is the source of her blood supply. Therefore, angiomas fill with blood and can, under certain conditions, cause hemorrhage.
Among the causes, neurologists and oncologists prefer to recognize a genetically determined defect. The genes responsible for the pathology have already been discovered. The inflammatory theory also remains relevant today.
Source: headexpert.ru
What is a cerebral cavernoma
Cavernoma (vascular malformation) is a benign tumor.
When pressed, it is elastic and soft, initially disappears, but soon returns to its original shape. Cavernoma (ICD code 10 – D33) is a brain tumor in the form of vascular cavities (cavities) containing air or blood breakdown products. These breakdown products consist of blood clots, connective tissue, etc. The size of cavities and their number can be different - several neoplasms can be adjacent to one another or located at some distance from each other.
Cavernous angioma has a knobby, bluish-colored surface with a heterogeneous structure; the tumor has clear boundaries that separate it from other tissues; most often it is round in shape. The partitions between the cavities consist of dense fibrous tissue. The size of the cavernoma can vary - from very small to several centimeters in diameter.
Multiple cavities occur in 10-15% of cases. Such cavernomas have a predisposition to frequent hemorrhages, and the medulla that surrounds them becomes yellowish as a result.
Cavernoma is localized in the head and neck area and affects the brain and spinal cord. This pathology occurs due to a genetic mutation during intrauterine development, when the formation of areas of the nervous system is disrupted. The presence of a cavernoma leads to a person’s loss of ability to adapt socially.
Symptoms and structure
The sizes of caverns can be very different - from microscopic to gigantic. The most typical cavernomas are 2–3 cm in size. Cavernomas can be located in any part of the central nervous system. Up to 80% of cavernomas are found supratentorially. Typical localization of supratentorial cavernomas is the frontal, temporal and parietal lobes of the brain (65%).
Rare cases include cavernomas of the basal ganglia and thalamus opticum - 15% of cases. Even less common are cavernomas of the lateral and third ventricles, the hypothalamic region, the corpus callosum, and the intracranial sections of the cranial nerves.
In the posterior cranial fossa, cavernomas are most often located in the brain stem, mainly in the tegmentum of the pons. Isolated midbrain cavernomas are quite rare, and medulla oblongata cavernomas are the least common. Cerebellar cavernomas (8% of all cavernomas) are most often located in the cerebellar hemispheres, less often in the vermis.
Cavernomas of the medial parts of the cerebellar hemispheres, as well as the vermis, can spread to the fourth ventricle and to the brain stem. Spinal cord cavernomas in our series accounted for 2.5% of all cavernomas. Taking into account the location of cavernomas in terms of difficulty of access and the risk of surgical intervention, it is customary to divide supratentorial cavernomas into superficial and deep.
Among superficial cavernomas, there are those located in functionally important zones (speech, sensorimotor, visual cortex, insula) and outside these zones. All deep cavernomas should be considered as located in functionally significant zones. According to our data, cavernomas of functionally significant areas of the cerebral hemispheres make up 20% of supratentorial cavernomas.
For cavernomas of the posterior cranial fossa, all localizations, with the exception of cavernomas of the lateral parts of the cerebellar hemispheres, should be considered functionally significant. CNS cavernomas can be single or multiple. The latter are detected in 10–20% of patients. According to our data, patients with multiple cavernomas made up 12.5% of those examined.
Single cavernomas are typical for the sporadic form of the disease, and multiple ones are typical for the hereditary form. The number of cases of multiple cavernomas in the hereditary form reaches 85%. The number of cavernomas in one person varies from two to 10 or more. In some cases, the number of cavernomas is so large that it is difficult to count.
Prevalence
Cavernomas can remain asymptomatic throughout a person’s life, so it is quite difficult to get an idea of the prevalence of the pathology. According to a few studies, cavernomas occur in 0.3%–0.5% of the population.
It is not possible to estimate what proportion of these cavernomas manifest clinically, since such studies are lacking. However, it is safe to say that the vast majority of cavernomas remain asymptomatic.
Cavernomas occur in two main forms: sporadic and hereditary. Until recently, it was believed that the sporadic form of the disease was the most common.
Studies in recent years have shown that the ratio of sporadic and familial cavernomas depends on the quality of examination of relatives of patients with clinically manifested pathology - the wider the scope of those examined, the higher the percentage of hereditary forms. According to some data, the frequency of hereditary forms reaches 50%.
Cavernomas of the central nervous system can manifest clinically at any age, from infancy to the elderly. Among those examined at the institute, in two cases the first symptoms of the disease appeared in the first weeks of life, and in several patients - at the age of over 60 years.
The most typical development of the disease is between the ages of 20 and 40 years. According to our data, with a hereditary form of the pathology, the first signs of the disease appear in childhood more often than with sporadic cavernomas. The ratio of men and women among patients with cavernomas is approximately the same.
Etiology and pathogenesis
Cavernomas can be sporadic and hereditary. The etiopathogenesis of the disease is most well studied for the hereditary form of the pathology. To date, an autosomal dominant type of inheritance has been proven and three genes have been identified, mutations of which lead to the formation of cavernomas: CCM1/Krit1 (locus 7q21.2), CCM2/GC4607 (locus 7q13-15), CCM3/PDCD10 (locus q25.2-q27 ).
Studies to decipher the molecular mechanisms of the implementation of these genes have shown that the formation of cavernomas is associated with a violation of the formation of endothelial cells. It is believed that the proteins encoded by the three genes work in a single complex complex. The etiology of sporadic cavernomas remains unclear.
It has been proven that some cavernomas can be radioinduced. There is also an immune-inflammatory theory of the genesis of the disease. The main mechanism for the development of any clinical symptoms in patients with cavernomas is single or repeated macro- or microbleeds. The criteria for the diagnosis of cavernoma hemorrhage remain the subject of debate.
The importance of this issue is due to the fact that the frequency of hemorrhages is one of the main factors in determining the indications for surgery, as well as in assessing the effectiveness of various treatment methods, especially radiosurgery.
Depending on the criteria used, the incidence of hemorrhage varies widely, from 20% to 55%. According to various sources, the frequency of hemorrhages ranges from 0.1% to 2.7% per cavernoma per year.
Clinical picture of the disease
In some cases, the reason for examination is nonspecific subjective symptoms. The clinical picture of the disease largely depends on the location of the formations. The most typical clinical manifestations of cavernomas are epileptic seizures and acutely or subacutely developing focal neurological symptoms.
The latter can occur both against the background of general cerebral symptoms and in their absence. In some cases, the reason for examination is nonspecific subjective symptoms, most often headaches.
In some patients, all these manifestations in various combinations are possible. Epileptic seizures are typical for patients with supratentorial cavernomas, in which they occur in 76% of cases, and when cavernomas are localized in the neocortex - in 90%.
The course of the epileptic syndrome is varied - from extremely rare seizures to the formation of drug-resistant forms of epilepsy with frequent seizures. Focal symptoms are typical for cavernomas of the deep parts of the cerebral hemispheres, brain stem and cerebellum. The most severe picture can develop with cavernomas of the diencephalic region and brain stem, which are characterized by the formation of alternating syndromes, including severe oculomotor disorders, pseudobulbar or bulbar symptoms. Repeated hemorrhages in this area lead to permanent disability.
With a certain localization of the cavernoma, the clinical picture may be due to occlusion of the cerebrospinal fluid pathways. Asymptomatic cavernomas are usually discovered during examination for some other disease, during preventive examinations, as well as during examination of relatives of patients with clinically manifested cavernomas.
Source: neurovascular.ru
Treatment and diagnosis of cavernous angioma
Most cavernomas do not require active treatment. All that is needed is dynamic observation over a long period of time. Surgery may be required if symptoms occur, which are usually caused by bleeding into the brain tissue surrounding the cavernoma.
In case of repeated hemorrhages detected on CT or MRI, hospitalization in a neurosurgical hospital is necessary with further decision-making on surgical intervention.
Because cavernomas are clearly demarcated from surrounding tissue and surrounded by glia, their surgical removal is a relatively simple task. Control of blood loss is also quite simplified, since blood flow in the pathological vessels is slower than what would normally be expected when excision of well-perfused tissue.
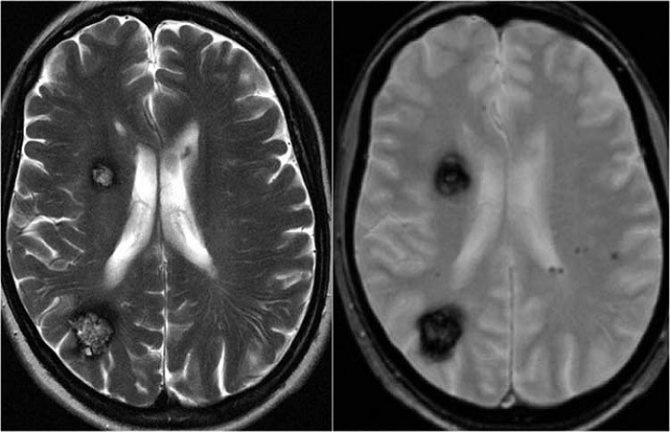
Despite the fact that cavernous angiomas are visualized using computed tomography (CT), this method is not the method of choice: the fact is that the identified signs in a CT study may correspond not only to cavernous angioma, but also, among other possible options, poorly differentiated tumor.
The sensitivity of magnetic resonance imaging (MRI) is much higher, due to its higher contrast resolution, as well as its greater ability to image flowing blood and its breakdown products.
The combination of different MRI pulse sequences has largely solved the problem of misdiagnosis or under-detection of cavernous angiomas, since these lesions have quite specific features on MRI.
CT and MRI can be used for follow-up of patients with already diagnosed cavernous angiomas, especially in cases where there is a risk of hemorrhage.
Although the MR image of cavernous angiomas does not predict the occurrence of bleeding, MRI is the method of choice for long-term follow-up of patients with cavernous angiomas, as well as for the evaluation of family members of the patient who are at risk of having such malformations.
In addition, MRI is extremely useful in planning surgical intervention, as it allows you to assess the size of the formation, its boundaries, and thus determine the type of operation and surgical approach. With classical angiography, most cavernous malformations are not visualized, and even when signs are detected, they are extremely nonspecific.
If the lesion develops in combination with other vascular malformations, which occurs in approximately 30% of patients with venous malformations, then its MR characteristics become much more complex and less specific.
In such patients, angiography may be useful to further clarify the diagnosis. Brain scanning using CT and MRI in most cases allows one to clearly distinguish a cavernoma from other brain formations, including tumors of varying degrees of malignancy.
However, in some cases, differentiation of these formations represents a diagnostic problem, the solution of which requires extensive experience. In this regard, the ability to attract a highly qualified diagnostician is critical.
In addition, high-quality interpretation of CT and MRI images provides a solution to other diagnostic problems: exclusion of surrounding cerebral edema, identification of the severity of hemorrhage, description of details affecting the operability of the cavernoma.
If you are in doubt about the diagnosis, you should consult a radiologist from a leading center specializing in brain pathology. A second opinion from such a diagnostician can be very valuable in the differential diagnosis of angiomas and other pathological conditions.
Source: teleradiologia.ru
Diagnostics
It is impossible to identify a cerebral hemangioma without a special examination. The absence of specific signs of pathology greatly interferes with making a correct diagnosis.
If vascular proliferation is suspected, doctors suggest undergoing:
- Angiography . This method involves the introduction of a contrast agent into the vascular system, after which an x-ray is taken.
- Superselective angiography , in which a contrast agent is injected into the area of the suspected location of the hemangioma.
- Computed or magnetic resonance imaging . These methods are considered the most accurate and harmless to the patient.
Using modern diagnostic techniques, it is possible to study the size, structure and localization of the growth, which will allow specialists to carry out adequate therapy.
Surgical removal
Cavernoma removal is a recognized effective method of treating the disease. At the same time, determining indications for surgery is a difficult task. This is primarily due to the fact that the disease has a generally benign course.
The vast majority of patients at the time of treatment do not have objective symptoms of central nervous system damage, and cases of persistent disability are noted mainly with repeated hemorrhages from cavernomas of deep structures and the brain stem, difficult to access for surgery.
On the other hand, predicting the course of the disease in each specific case is impossible, and a successfully performed operation can forever save the patient from the risks associated with the disease. We consider the localization of the cavernoma and the clinical course of the disease to be the main criteria in determining the indications for surgery.
Based on these factors, surgery is indicated in the following cases: Cavernomas of a superficial location outside functionally significant areas, manifested by hemorrhage or epileptic seizures.
Cortical and subcortical cavernomas located in functionally significant areas, deep cavernomas of the cerebral hemispheres, brainstem cavernomas, cavernomas of the medial parts of the cerebellar hemispheres, manifested by repeated hemorrhages with the formation of persistent neurological disorders or severe epileptic syndrome.
In addition to the above criteria, there are a number of conditions that determine the indications for surgery: the size of the cavernoma, the duration of the hemorrhage, the patient’s age, concomitant diseases, etc.
In any case, the indications for cavernoma removal are relative, so a necessary condition for making a decision is the patient’s awareness of the nature of the disease and its course options, the purpose of the operation and its possible outcomes.
For difficult-to-reach cavernomas, radiosurgical treatment is possible, although information about its effectiveness is contradictory. When using this method, the patient must be informed about the risk of complications.
Surgical interventions: technique and results
Planning of access and surgical intervention for removal of cerebral cavernomas generally correspond to the general principles used in surgery of space-occupying brain lesions. In the case of superficial subcortical localization, the search for malformation is greatly facilitated by the presence of post-hemorrhagic changes in the superficial cortex and meninges.
To improve the outcome of treatment of epilepsy, in some cases a technique is also used to excise the medulla around the cavernoma, which is macroscopically altered by blood breakdown products, although information about the effectiveness of this technique is contradictory.
The cavernoma, as a rule, is clearly demarcated from the medulla, which simplifies its isolation. If the cavernoma is localized outside functionally important areas, identifying the malformation in the area of perifocal changes and removing it in one block significantly facilitates and speeds up the operation.
Operations to remove cavernomas located in functionally significant cortical and subcortical parts of the brain, as well as in the deep structures of the cerebral hemispheres, have a number of features. In case of hemorrhage from a cavernoma of this localization, the patient should be monitored for 2–3 weeks.
The absence of regression of focal symptoms during this period provides additional justification for surgical intervention. When making a decision about surgery, you should not wait for the hematoma to resolve, since due to the processes of organization and gliosis, the operation becomes more traumatic.
Internal decompression of a cavernoma by evacuation of the hematoma is a necessary step when removing cavernomas from functionally significant areas, as it allows to reduce surgical trauma. Resection of perifocal posthemorrhagic changes is impractical.
To improve the outcomes of cavity removal, various instrumental intraoperative auxiliary techniques are used. In the absence of clear anatomical landmarks, it is advisable to use intraoperative navigation methods. Ultrasound scanning in most cases allows you to visualize the cavity and plan the access trajectory.
A significant advantage of the method is the provision of information in real time. Ultrasound imaging of cavernomas can be difficult for small lesions. Frameless neuronavigation based on preoperative MRI data allows for the most accurate planning of access and craniotomy of the required (minimum possible for a given situation) size.
It is advisable to use the technique to search for small caverns. Stimulation of the motor area with assessment of the motor response and M-responses should be used in all cases of possible intraoperative damage to the motor cortex or pyramidal tracts.
The technique allows you to plan the most gentle access to the cavernoma and evaluate the possibility of excision of the zone of perifocal changes in the medulla. Intraoperative use of ECoG to assess the need for excision of distant foci of epileptiform activity is advisable in patients with a long history of epilepsy and drug-resistant seizures.
In the case of epileptic lesions of the medial temporal structures, the technique of amygdalohippocampectomy under ECoG control has shown high effectiveness.
For any location of the cavernoma, one should strive for complete removal of the malformation due to the high frequency of repeated hemorrhages from partially removed cavernomas. It is necessary to preserve venous angiomas found in the immediate vicinity of cavernomas, since their excision is associated with the development of disturbances in the venous outflow from the medulla adjacent to the cavernoma.
In most cases, cavernomas, even very large ones, can be completely removed, and the outcomes of operations are usually favorable: most patients do not experience neurological disorders. In patients with epileptic seizures, improvement is noted in 75% of cases, and in 62% of cases, seizures do not recur after removal of the cavernoma.
The risk of developing postoperative neurological complications depends largely on the location of the formation. The incidence of defects in cavernomas located in functionally insignificant parts of the cerebral hemispheres is 3%. With cortical and subcortical cavernomas of functionally significant areas, this figure increases to 11%.
The risk of the appearance or worsening of a neurological deficit in the case of removal of a deep-seated cavity reaches 50%. It should be noted that the neurological defect that occurs after surgery is often reversible. Postoperative mortality is 0.5%.
Treatment of cavernous angiomas of the brain stem has a number of features that justify the classification of this pathology into an independent group. First of all, the anatomy and functional significance of the trunk makes surgical interventions in this area extremely difficult.
Due to the compact location of a large number of various, including vitally important, formations in the brain stem, any, even minimal, hemorrhages from the trunk cavernomas cause neurological disorders, which distinguishes the course of the disease from the clinical manifestations of cavernomas of the cerebral hemispheres.
The small size of trunk cavernomas often complicates histological verification of the pathology, and therefore the nature of the disease more often than with cavernomas of other localizations remains unrecognized.
According to MRI and surgical data, three variants of pathological formations can be distinguished, united by the common name “trunk cavernomas”.
Subacute and chronic hematomas, when removed only in 15% of cases it is possible to verify the cavernous tissue. It cannot be ruled out that these hematomas are based on malformations other than cavernomas, possibly telangiectasia. Typical cavernomas in combination with acute, subacute or chronic hematoma.
Typical cavernomas, having a heterogeneous structure and surrounded by a ring of hemosiderin, without signs of hemorrhage. In the clinical course of cavernous trunk, there are two main options. The stroke-like variant is characterized by the acute development of pronounced brainstem symptoms, often against the background of intense headache.
Removal of trunk cavernoma
Removal of a hematoma and/or cavernoma is performed from the side closest to the surface of the brain stem. Most often, median suboccipital craniotomy with access through the fourth ventricle is used. This is due to the fact that most of the hematomas and malformations are located subependymal, in the area of the bridge tire. Even with large hematomas that occupy almost the entire diameter of the trunk, this approach is the most acceptable due to the ease of its implementation and less trauma compared to other approaches. For cavernomas and hematomas located in the ventral-lateral sections of the bridge, from our point of view, the most optimal are the retrolabyrinthine, presigmoid and subtemporal approaches, since they provide a wider viewing angle of the surgical field and, accordingly, a greater possibility of radical removal of the malformation and the capsule of the chronic hematoma .
Removal of hematomas and midbrain malformations is possible through subtentorial supracerebellar or suboccipital transtentorial approaches. An important stage of the operation is to determine the projection of the location of the cranial nuclei in the bottom of the rhomboid fossa (mapping) by recording motor responses.
Information about the location of the main nuclear structures of the brain stem allows the surgeon to manipulate as far away from these formations as possible. When performing operations on the brain stem, spatulas are not used - the surgeon creates a field of view with the instruments he uses to perform the operation - suction, tweezers, scissors, etc.
During the operation, the cavernous angioma is divided into fragments and removed in parts. In case of chronic hematomas, the capsule should be completely removed if possible.
If the cavernoma or chronic hematoma capsule is incompletely removed, repeated hemorrhages are possible. More often they occur after removal of chronic hematomas. This is due to the fact that if there is insufficient revision of the hematoma walls, fragments of a small malformation that was the cause of the first hemorrhage may remain in it. Subsequently, this malformation can transform into a larger cavernoma.
Source: neurovascular.ru
Possible complications
If the angioma begins to progress, the sick person experiences discomfort in the area of the tumor.
Dizziness appears, memory and speech are lost, vision decreases, and coordination of movements is impaired. Complications of angioma depend on the location of the formation: In the area of the eye and ear - dysfunction of these organs or irreversible loss of vision and hearing. On the skin - the formation of ulcers, platelet retention, heart failure. In the sacral area - dysfunction of the pelvic organs and intestines due to damage to the spinal cord. In the brain area, rupture of an angioma leads to epileptic seizures and hemorrhage. For newborns, pregnant women and adolescents, lymphangioma is a concern. It can compress neighboring organs, which leads to the development of hypoxia and ischemia of the heart. Rarely, lymphangioma develops into lymphosarcoma with metastases to the lymph nodes. When lymphangioma becomes infected, phlegmon develops - acute purulent inflammation.
Consequences
Cavrenous tumors of the cerebral cortex, in addition to general cerebral symptoms (vomiting, epileptic convulsions and headache), cause focal lesions. In contrast to localization in the trunk region, cortical neoplasias are very common.
If the focus of cavernoma hemorrhage is the frontal lobe, or there is a large angioma there that compresses the brain substance, a characteristic symptom complex develops. After hemorrhage, the surrounding brain tissue is saturated with hemosiderin and other metabolic products and is disabled.
Damage to the right or left temporal lobe carries the risk of complications such as aphasia (inability to pronounce words), hallucinations (associated with hearing), hemianopsia (loss of visual fields). If the cavernous hemangioma is located in the right temporal lobe of the non-dominant hemisphere (right for right-handed people and left for left-handed people), then the consequences will be less serious, and everything will turn out to be transient auditory hallucinations.
But when the tumor is localized in the dominant hemisphere (right temporal lobe in left-handed people and left temporal lobe in right-handed people), aphasia (Wernicke's aphasia, associated with damage to the cortical center of the same name) is possible. For any lesion of the temporal lobes, the development of delirium may be typical, the mechanism of development of which in this situation is not fully understood.
The presence of a cavernoma causes consequences associated primarily with neurological disorders and focal brain lesions. The tumor grows, squeezing the substance of the brain, and the symptoms described above begin to appear. After a hemorrhage occurs, the brain substance is saturated with hemosiderin and other metabolic products, the result is the shutdown of some functions.
If the frontal lobe is damaged, the patient loses practical skills and cannot critically evaluate himself and others. If the right or left temporal lobes are damaged, loss of visual fields (hemianopia), impaired functioning of the hearing organs, and impaired ability to pronounce words (aphasia) may occur. If the lesion does not occur in the dominant area of the temporal lobe, the development of mental disorders is typical.
If the diagnosis of cavernoma occurred at a late stage of development, when the inflammatory process or dystrophic transformations began, then the following complications may occur:
- hemorrhages;
- cerebrovascular accident;
- rupture of blood vessels and disruption of local blood flow;
- increase in vascular congestions and cavities;
- death.
Prevention of cavernous angioma
In order to prevent angiomas of all types, it is necessary to avoid stress and prevent injuries. Alcoholic drinks can only be consumed in minimal quantities. Women are advised to properly prepare for pregnancy.
Experts recommend taking folic acid. You need to spend less time in the sun. Scientists have not developed prevention of congenital angioma.
If you notice any of the above signs, you should definitely consult an experienced specialist. He is guaranteed to be able to save you from an unpleasant disease.
Source: skalpil.ru