MRI of the hippocampus
– a targeted study of a paired structure located in the temporal lobes of the brain, involving the receipt and digital processing of radio signals from hydrogen atoms when they are in a constant high-intensity magnetic field. MRI of the hippocampus can be performed alone or as part of a comprehensive brain study. Allows for a morphometric assessment of this intracerebral structure responsible for the formation of memory and emotions. Magnetic resonance imaging can detect changes in the size of the hippocampus (hyperplasia, atrophy, sclerosis). In neurological practice, MRI of the hippocampus is informative in the diagnosis of epilepsy, Alzheimer's disease, and the causes of amnesia.
MRI of the hippocampus
– a targeted study of a paired structure located in the temporal lobes of the brain, involving the receipt and digital processing of radio signals from hydrogen atoms when they are in a constant high-intensity magnetic field. MRI of the hippocampus can be performed alone or as part of a comprehensive brain study. Allows for a morphometric assessment of this intracerebral structure responsible for the formation of memory and emotions. Magnetic resonance imaging can detect changes in the size of the hippocampus (hyperplasia, atrophy, sclerosis). In neurological practice, MRI of the hippocampus is informative in the diagnosis of epilepsy, Alzheimer's disease, and the causes of amnesia.
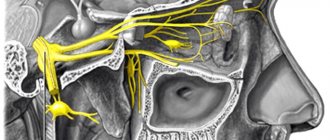
The very idea of developing a magnetic resonance imaging method was born precisely to solve the problem of visualizing brain structures, including the hippocampus. Since the brain consists of soft tissues, the use of X-ray techniques for this purpose is difficult; diagnosis is possible only by indirect signs (for example, expansion of the sella turcica with enlargement of the pituitary gland). Computed tomography is more informative in this regard, but it can only visualize structures that differ significantly in density (bone and brain tissue, brain tissue and cerebrospinal fluid in the ventricles). Unlike X-ray techniques, magnetic resonance imaging is built on completely different physical principles - the phenomenon of nuclear magnetic resonance. To put it simply, we can say that atoms, when exposed to a strong magnetic field, line up in accordance with their rotation (spin). At the same time, atoms whose rotation is opposite to the direction of the field are excited and, when irradiated with radio waves of a certain length, they themselves re-emit them. Capturing this radiation makes it possible to construct an image.
Modern devices used for MRI of the hippocampus capture radio waves from hydrogen atoms found in water and a number of organic compounds. The more water there is in the tissue, the brighter it will “glow” in the radio range when exposed to electromagnetic waves. Because different structures of the brain contain different amounts of water, lipids and other compounds, MRI can be used to study not only the brain as a whole, but also to visualize individual parts of it. MRI of the hippocampus has become an increasingly common study in recent years, as experts have established the role of this organ in the development of Alzheimer's disease, epilepsy, depression, and memory impairment. Therefore, for diagnosis (including differential) of these conditions, the hippocampus is examined.
MRI of the hippocampus is most often used in neurology; this study provides a unique opportunity to detect the earliest changes in the structure of the organ. Other modern diagnostic techniques are either capable of detecting only deep lesions in this part of the brain (for example, computed tomography), or are much more expensive with comparable or even less information (for example, positron emission tomography). In addition, MRI of the hippocampus is very often performed as part of research work to study the mechanisms of memory, the development of age-related changes in the brain, the causes of epilepsy and other neurological diseases.
Function
The hippocampus is part of the limbic system, which is associated with feeling and responding functions.
The limbic system is located at the edge of the cortex, and it includes the hypothalamus and amygdala.
These structures help control various body functions, such as the endocrine system and what is commonly called the "fight or flight" response.
Hippocampus and memory
The hippocampus helps people process and retrieve two types of memory, declarative memories and spatial relationships.
Declarative memories are those that relate to facts and events. Examples include learning to memorize speeches or lines in a play.
Spatial memory memories are associated with paths or routes. For example, when a taxi driver learns a route through a city, they use spatial memory. Memories of spatial relationships appear to be stored in the right hippocampus.
The hippocampus is also where short-term memories are turned into long-term memories. They are then stored elsewhere in the brain.
Research has shown that nerve cells continue to develop into adulthood. The hippocampus is one of the few places in the brain where new nerve cells are generated.
Preventive actions
In order to reduce the frequency of seizures, experts recommend regularly taking prescribed medications, as well as:
- Follow a rest and sleep schedule; you need to go to bed and wake up at the same time.
- Adhere to a diet that includes limiting the consumption of spicy, salty and fried foods, as well as liquids.
- Avoid consuming alcoholic beverages; alcohol-containing products lead to the development of many different diseases.
- Eliminate the consumption of tobacco products - tobacco and combustion products negatively affect all body systems.
- Avoid overheating or hypothermia of the body; to do this, you should avoid visiting baths and saunas, and sunbathing in the open sun.
- Eliminate consumption of tea and coffee.
What could go wrong?
If one or both parts of the hippocampus are damaged by diseases such as Alzheimer's disease, or if they are damaged in an accident, a person may lose memory and lose the ability to create new, long-term memories.
They may not be able to remember some things that happened shortly before the hippocampus was damaged, but they can still remember things that happened longer. This is because long-term memories are stored in a different part of the brain once they become long-term.
Transient global amnesia is a special form of memory loss that develops suddenly, seemingly on its own, and then goes away quite quickly.
Most people with transient global amnesia eventually regain their memories, but the reasons why the problem occurs and why they resolve are unclear. This may be due to damage to the hippocampus.
Damage to the hippocampus can make it difficult to remember how to get from one place to another. A person can draw a map of the neighborhood they lived in as children, but finding their way to a store in a new area can be difficult.
It is also associated with conditions such as schizophrenia and post-traumatic stress disorder (PTSD).
Methodology
MRI of the hippocampus is performed using specialized equipment that creates a strong magnetic field to excite hydrogen atoms in the tissues being examined. Magnetic field strength, measured in teslas, is the most important characteristic of an MRI machine - the highest quality results are obtained on equipment with a strength of at least 1 Ts. Traditional closed devices consist of a superconducting magnet with a tunnel into which the patient is placed. At the same time, there are restrictions on the size and body weight of the subject; problems are possible if the patient has claustrophobia. Some clinics have open devices that operate on permanent neodymium magnets - they are used if the patient is extremely obese or claustrophobic.
During an MRI of the hippocampus, it is very important to keep your head still, as any movement can blur the image and reduce the value of the diagnostic study. The scanning takes several minutes, after which an image of the hippocampus and other elements of the brain in any plane is formed on a computer through mathematical processing of data. Hippocampal MRI results can be stored on digital media (disk) or recorded on special film. The results are interpreted by a radiologist, and the diagnosis is made by the specialist who referred the examination.
Diseases that affect the hippocampus
The hippocampus is the sensitive part of the brain. It can be negatively affected by a number of conditions, including long-term exposure to high levels of stress.
Certain diseases and factors are known to impair the hippocampus's ability to do its job.
Alzheimer's disease
The hippocampus is one of the first areas that can be affected by Alzheimer's disease. An early sign of Alzheimer's disease is when a person begins to lose their short-term memory. They may also have difficulty following directions.
As the disease progresses, the hippocampus loses volume and it becomes increasingly difficult to function in daily life.
Epilepsy
Autopsies suggested that 50 to 75 percent of people with epilepsy have damage to the hippocampus.
However, it is unclear whether epilepsy is the cause or result of this damage.
Depression and stress
In people with severe depression, the hippocampus loses volume.
Scientists are not sure whether small size is a result of depression or a contributing factor. There is evidence that stress has a negative effect on the hippocampus.
Causes
Depending on the severity of the pathological process, the disease can be either borderline in nature - subatrophy, or terminal - atrophy. These phenomena are caused by a number of reasons. These include:
- Hereditary genetic predisposition;
- Toxic alcoholic, narcotic or medicinal effects;
- Traumatic brain injuries received both in the event of an accident and during neurosurgical interventions;
- Ischemic abnormalities in the vascular bed of the brain;
- Neoplasms that compress the bloodstream;
- Hydrocephalus in children;
- Chronic anemia.
Subatrophic changes in the brain, what is it? This is a condition that precedes the death of neurons. It's moderate. This means that the pathological process has already started, but the body is still compensating and containing the disease. In addition to the main list of factors that trigger the process, atrophy provocateurs can be:
- Lack of intellectual stress;
- Long-term use of drugs that constrict blood vessels.
What happens if the hippocampus is small?
Alzheimer's disease, depression and stress appear to be associated with a smaller hippocampus.
In the case of Alzheimer's disease, the size of the hippocampus can be used to diagnose the progression of the disease.
In people with depression, the hippocampus may shrink by 20 percent, according to some researchers.
Reviews of studies have found that the hippocampus in people with severe depression may be on average 10 percent smaller than in those without depression.
Cushing's disease has a number of symptoms that are associated with high levels of cortisol, a hormone produced when people are under stress. One of these symptoms is a decrease in the size of the hippocampus.
A study in monkeys found that hippocampal size was 54% heritable. However, because the hippocampus continues to produce neurons throughout adult life, the connection remains unclear.
It is also unclear whether a small hippocampus is the underlying cause of certain conditions or whether it is a result.
Diagnosis and treatment
To confirm the fact of the disease, the doctor must conduct a neurological examination. The patient is observed visually and is also tested for reactivity to stimuli and reflexes. The doctor collects the patient’s medical history – that is, all the information about the supposed origin of the disease. The likelihood of a genetic predisposition to atrophy is being clarified.
Instrumental research methods complement the diagnostic picture. MRI or CT can be used for this. And if a newborn baby is suspected of having the disease, an ultrasound scan is performed. These studies make it possible to obtain specific CT, ultrasound or MR signs characteristic of a given disease.
Subatrophic or atrophic changes in the brain require complex therapy for patients. Be sure to provide patient care. As the pathology progresses, his socialization decreases significantly. Therefore, the support of loved ones will be necessary.
It is important to create a calm atmosphere so that external stimuli are less likely to provoke his dying brain. If possible, they try to remove the causes that caused the disease. If the provoking factor of atrophy is ischemia, then drugs are prescribed that improve blood supply, or attempts are made to remove the neoplasm that creates the block. In case of intoxication, stop taking harmful substances.
To curb the restless temperament of a sick person, sedatives, tranquilizers, and antidepressants are often prescribed. Physical activity is an indispensable companion to therapeutic measures.
Current research
In 2020, scientists published a review of research into the effects of exercise on cognitive decline and aging.
The results suggest that exercise in old age can enhance this structure's ability to generate new nerve cells. This will preserve and potentially improve memory. However, how this happens remains unclear. In addition, a number of variables influence the result. More research is needed to confirm any results.
In August 2020, researchers from Hong Kong published results suggesting that low-frequency activity in the hippocampus can lead to functional connectivity in other parts of the brain. In other words, activity in the hippocampus may influence not only memory and wayfinding, but also functions such as seeing, hearing and touch.
In this sense, the hippocampus can be described as the “heart of the brain.”
Source: medicalnewstoday.com/articles/313295.php
Diagnostic measures
Neurologists are involved in diagnosing this condition. It is this specialist who should be contacted if the clinical picture described above manifests itself. During the first visit, the attending physician will talk with the patient to obtain a medical history. During the dialogue, the doctor assesses the patient’s intellectual capabilities and determines behavioral traits. If emotional or intellectual abnormalities are detected, the patient is referred for examination to a psychiatrist.
Along with this, the medical specialist will undertake a number of manipulations to assess the patient’s reflexes:
During the diagnosis, the patient undergoes the following studies:
- An electroencephalogram allows you to identify existing foci of pathological impulses in the brain.
- CT and MRI make it possible to take a layer-by-layer image of the brain and other structures of the skull.
- Angiography determines the presence of disturbances in the blood flow of the brain.
- ECHO is an encephalogram, which is important if the patients are newborns or young children.
Prevention
- Young children, especially infants, should sleep on their backs to prevent sudden infant death syndrome (SIDS), although the back of the head may become flattened. But to avoid problems, alternate the position of your baby's head.
- Be sure to place your baby on his tummy and play with him for as long as possible.
- Do not forget about such procedures as and. They will strengthen the muscles of the neck and back, so the child will be able to turn his head independently, taking a position that is comfortable for him.
Hippocampal sclerosis is the most “fashionable trend” in neurology and radiology now, by the way. Here we are competing with each other to see who was the first to “see the hippocampus,” but the public is indifferent... And in the West there are entire official communities of “hippocampus lovers”...
I think it's epileptic
I think that this is status epilepticus, but we need dynamics after 2-3 non-epileptic weeks
and the case that you indicated is that one and that one and the same person or what?
IT, and a variant of herpetic
IT, can’t there be a variant of herpetic encephalitis here? With sclerosis of the hippocampus, there should be a decrease in volume, but here it seems to be symmetrical, or does this require more time? For my understanding, this is a complex topic, but interesting and relevant, because... Several times I saw on a CT scan the asymmetry of these parts of the brain and there was a clinic for epilepsy, the hippocampus was small, the sulci were widened and the temporal horn was deepened, I regarded this as medial temporal sclerosis.
You are looking only at the heads of the hippocampi (this area is mainly represented, where the mass and the focus of accumulation are), but there are a couple of sections at the level of the bodies caudal - it is not symmetrical there. Plus: hippocampal sclerosis is manifested not only by volumetric reduction of the hippocampus. Some points on CT cannot be clarified technically, CT for epilepsy, unfortunately - ((((((. If only the changes are pronounced, then yes. This is my individual opinion.
I think you're right
It seems to me that you correctly put FCD and DNET in the differential row, I would even put DNET in first place, contrast can be regarded as a neuroradiological marker of DNET, this formation contains dysplastic cells and neuroglia, and the more dysplastic cells the less capable of contrast it is amplification, maybe this is the same case, and according to the literature, DNET can outwardly almost completely mimic FCD. Regarding other causes, these could be ganglogliomas, oligodendrogliomas, but there the cystic component still predominates in the structure, which is not the case in this case. They also describe it as a variant of astrocytoma I II, but I don’t know about this, maybe in last place in the differential. diagnosis can be made, although there should be at least a slight mass effect and perifocal edema. Against encephalitis, there is a long history of detectable changes, because they were previously on MRI, even if they were not contrasted. The tumor nature of the lesion may be due to the clinical picture of steadily progressing epilepsy and poor amenability to treatment, but this is relative.
Thank you for your comment.
Thank you for your comment. There is still a slight mass effect; you can compare the medial contours of the structures in the coronal projection. What is your opinion about not only FKD OR DNET, but FKD AND Dnet? It’s a shame that there is no verification in the first case; I would like to build on personal experience with morphology...
In the book by Prof. Alikhanov
In the book by Prof. Alikhanova found: associated FCDs are isolated, i.e. various variants of cortical dysgenesis coexisting in close topographical relationship (and sometimes losing a clear histological separation from each other), most often classic Taylor or balloon cell FCD are combined with gliomamia and hippocampal gliosis, forming FCD associates.
Researchers from Harvard Medical School in Boston, Massachusetts, studying the pathophysiology of mental disorders, found that patients with such disorders have smaller hippocampal volume. Previous studies have suggested that changes in the medial temporal lobe (MTL), hippocampus, parahippocampal gyrus, and entorhinal cortex are hallmarks of schizophrenia. Attempts to identify the extent of differences in patients with other mental disorders have remained inconclusive, however, for example, in bipolar disorders, changes in the medial temporal lobe are minor or absent. Other studies have also failed to find any reduction in hippocampal volume in patients with bipolar disorder who took lithium.
Scientists from Harvard conducted scientific work using neuroimaging in healthy volunteers and patients with schizophrenia, schizoaffective and psychotic bipolar disorders. According to the results, the medial temporal lobe decreases in volume in patients with schizophrenia and schizoaffective disorder, but not in patients with psychotic bipolar disorder. In addition, a decrease in hippocampal volume was found in all three groups of patients with mental disorders, compared to healthy volunteers. Each disturbance in mental work is accompanied by certain changes characteristic of this condition. The researchers also found that the extent of hippocampal volume reduction depended on the severity of psychosis, memory status, and overall cognitive performance.
But despite the correlation between symptoms and volume reduction in various areas of the hippocampus, the authors acknowledge that it is too early to say anything concrete. The patients in this study were treated with antipsychotic medications, and the researchers plan to further study the problem to examine changes in the brain before and after starting to use the drugs. Additionally, this study did not include patients with nonpsychotic bipolar disorder, so the researchers cannot expect their findings to generalize to patients with this diagnosis.
This study used the most advanced technology to analyze the functioning of the hippocampus to date. This made it possible to study small substructures in the hippocampus in a large sample of individuals with certain mental disorders, including schizophrenia and psychotic bipolar disorders. Scientists' observations show that changes in the hippocampus, a key region of the brain responsible for the formation, storage, processing and retrieval of memories, may not be caused only by schizophrenia, but occur in connection with a whole range of psychotic disorders.
When studying the human brain, scientists found that even the most powerful computer cannot compare with this part of the human body. The researchers paid particular attention to a small structure in the brain called the .
(c) Shutterstock
Positional plagiocephaly
Cranial Correction Helmet for Plagiocephaly
If your child has flat head syndrome caused by sleeping position, there are many treatment options that can be easily applied at home after consultation with a doctor.
- Changing head position while . Turn your baby's head (left to right, right to left) when he sleeps on his back. The baby can move throughout the night; you can force him to maintain the desired position using special devices in the form of slightly uneven pillows.
- Alternative positions in the crib. Usually parents put the baby in the same direction, as a result, the inquisitive baby begins to look at the room and the people entering in the same direction. As a result, torticollis may develop with flattening, for example, on the right side of the head. Changing the baby's position will encourage active head turns in the other direction.
- Hold your baby in your arms more often. Reduce the amount of time your baby spends lying on his back or with his head resting on a flat surface (such as in a car seat, stroller, swing, etc.). For example, if your baby falls asleep in the car seat while traveling, be sure to move him to the bed rather than leaving him in the carrier. By holding your baby in your arms, you force his muscles to develop, which is an excellent prevention of plagiocephaly.
- Place your baby on his tummy. Allow enough time to place your baby on his tummy. This will contribute to the normal formation of the back of the head and develop the muscles of the neck and back. By looking around the child will learn and socialize faster. In addition, he will begin to sit down faster.
Since most children with plagiocephaly have some degree of torticollis, physical therapy and an exercise program will be an essential part of the recommended treatment. A physical therapist can teach you how to do stretching exercises. Most movements will involve stretching the neck in the direction opposite to the tilt. In due course, the neck muscles will become longer and the neck will straighten. Even though all the exercises are very simple, they must be done correctly.
For children with severe flat head syndrome for whom position adjustments have not improved the situation within 2-3 months, doctors may prescribe molded helmets or other devices. A helmet helps most when used between 4 and 12 months, when the baby is growing most quickly and his bones are most flexible. The result is achieved by applying light but constant pressure to the baby's growing skull in an attempt to redirect growth.
Important condition: never use specialized devices to correct the skull without prior approval from your doctor. The decision to use a helmet in therapy is made on an individual basis, and this method may be prescribed in serious cases, for example, if the child is at risk of facial deformation in the future.
When a condition requires correction
Babies are born with “soft bones” in the head to allow the brain to develop quickly and without restriction. Passage through the birth canal during childbirth, especially if prolonged or complicated, can lead to deformation of the newborn's head. So it's completely normal for a baby's skull, which is made up of several bones, to have a slightly odd shape for a few days or weeks after birth.
But if your baby eventually develops a flat spot on one side of the head or on the back of the skull, it's called flat head syndrome. This problem does not harm brain development or cause long-term appearance problems, so it does not require surgery. In this case, simple methods such as changing the baby's sleeping position can help.