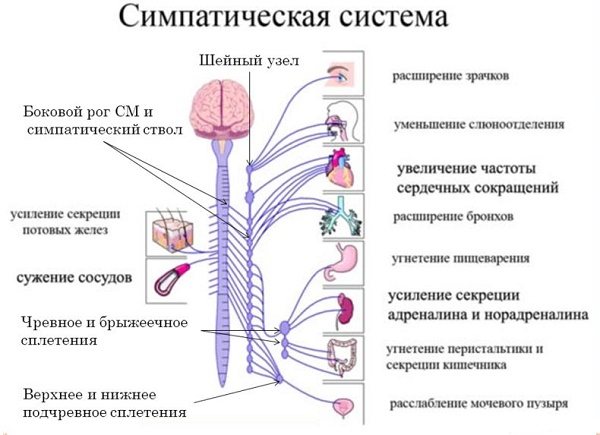
The sympathetic department is part of the autonomic nervous tissue, which, together with the parasympathetic, ensures the functioning of internal organs and chemical reactions responsible for the life of cells. But you should know that there is a metasympathetic nervous system, part of the autonomic structure, located on the walls of organs and capable of contracting, contacting directly with the sympathetic and parasympathetic, making adjustments to their activity.
The human internal environment is directly influenced by the sympathetic and parasympathetic nervous system.
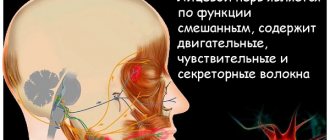
The sympathetic division is localized in the central nervous system. Spinal nerve tissue operates under the control of nerve cells located in the brain.
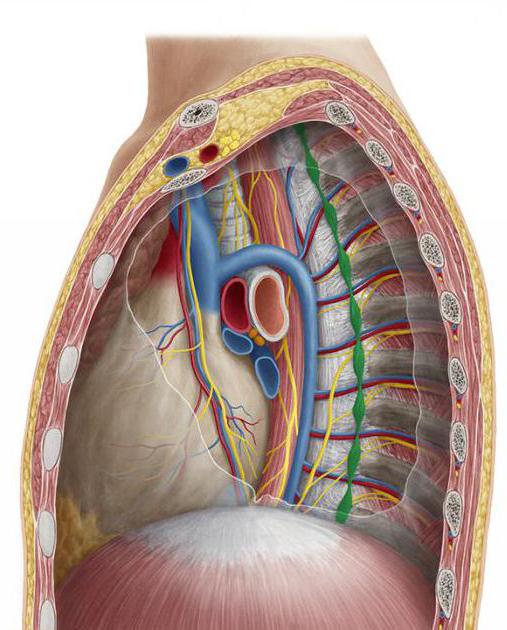
All elements of the sympathetic trunk, located on two sides of the spine, are directly connected to the corresponding organs through nerve plexuses, and each has its own plexus. At the bottom of the spine, both trunks in a person are united together.
The sympathetic trunk is usually divided into sections: lumbar, sacral, cervical, thoracic.
The sympathetic nervous system is concentrated near the carotid arteries of the cervical region, in the thoracic artery - the cardiac and pulmonary plexus, in the abdominal cavity the solar, mesenteric, aortic, hypogastric.
These plexuses are divided into smaller ones, and from them impulses move to the internal organs.
The transition of excitation from the sympathetic nerve to the corresponding organ occurs under the influence of chemical elements - sympathins, secreted by nerve cells.
Interaction of systems
They supply the same tissues with nerves, ensuring their relationship with the central system, often having the opposite effect on these organs.
The influence that the sympathetic and parasympathetic nervous systems have can be seen from the table below:

Together they are responsible for cardiovascular organisms, digestive organs, respiratory structures, secretions, the work of smooth muscle of hollow organs, and control metabolic processes, growth, and reproduction.
If one begins to predominate over the other, symptoms of increased excitability appear: sympathicotonia (the sympathetic part predominates), vagotonia (the parasympathetic part predominates).
Sympathicotonia manifests itself in the following symptoms: fever, tachycardia, numbness and tingling in the extremities, increased appetite without the appearance of weight loss, indifference to life, restless dreams, fear of death for no reason, irritability, absent-mindedness, decreased salivation, as well as sweating, migraine appears.
In a person, when the increased work of the parasympathetic department of the autonomic structure is activated, increased sweating appears, the skin feels cold and damp to the touch, a decrease in heart rate occurs, it becomes less than the prescribed 60 beats in 1 minute, fainting, salivation and respiratory activity increase. People become indecisive, slow, prone to depression, and intolerant.
The parasympathetic nervous system reduces the activity of the heart and tends to dilate blood vessels.
What do system pathologies lead to?
In the body, the activity of all internal organs is provided by signals from the autonomic system. Any violation of it leads to a decrease in the body’s protective functions. This provokes destabilization of general well-being and can develop functional or organic damage to the nervous system.
In the medical classification of diseases, there are several types of autonomic dysfunction:
Somatoform disorder. Refers to one of the types of neurosis. It manifests itself as symptoms of existing chronic pathologies in humans.
Systematic impact of irritating factors on the vegetative structures of the peripheral region. Precursors to the development of this pathology are premenstrual tension syndrome and cervical dorsopathy.
Damage to subcortical structures. It is one of the consequences of brain injury or residual pathology of the central nervous system.
In today's intense pace of life, many people have autonomic disorders. According to medical statistics, about 75% of adults and 20% of children are familiar with this pathology.
The etiology of the development of autonomic dysfunction is associated with the following factors:
- Constantly being in a stressful situation
- Hereditary predisposition
- Dysfunction of the hormonal system, especially during puberty
- Having excessive excess weight
- Birth injuries in children
- Unbalanced diet
- Abuse of negative habits
- Strong physical and psycho-emotional stress
- Infectious pathologies
- Inactive lifestyle

- Surgery or injury to nerve connections
- The entry of toxins into the nervous and circulatory systems as a consequence of inflammation
- Self-medication or a long course of potent medications
- Various pathologies associated with the presence of allergies in the body
Characteristic signs of autonomic disorders are a complex of symptoms, among which it is worth highlighting neurosis and neurasthenia. Also, a person’s intestinal motility is impaired, the nutrition of muscle fibers deteriorates, the sensitivity of the skin changes and an allergic reaction appears.
All symptoms of this pathology are divided into several classes:
- Cardiovascular system syndrome. Dysfunction of the heart rhythm, disturbances in pressure and blood flow, discomfort in the area of the heart muscle.
- Da Costa syndrome. Choking, rapid breathing, spasms of muscle fibers, loss of sensation in the limbs.
- Irritable bowel syndrome. Systematic urge to have a bowel movement, flatulence, cramping and pain in the abdominal area, diarrhea.
- Dysfunctions of the digestive system. Feeling of a lump in the throat, loss of appetite, nausea, vomiting, discomfort in the stomach.
- Hyperhidrosis of the feet and palms.
- Genital-vesical neurosis. It manifests itself as paruria with high frequency and acute painful sensations.
- Sexual disorders. Lack of erection and seminal fluid discharge, lack of orgasm and sexual desire.
- Hyperthermia and hypothermia of the body.
Often many people do not attach importance to these symptoms. Or they may attribute these symptoms to other types of diseases. But, over time, the general condition of a person worsens significantly. Signs of vegetative dystonia begin to accumulate and increase in intensity.
In this case, even the slightest manifestations of such pathology should not be ignored. You should immediately consult a doctor for a full examination and subsequent treatment.
Functions
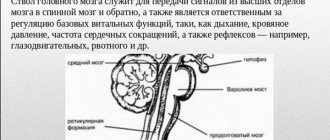
The sympathetic nervous system is a unique design of an element of the autonomic system, which, in the event of a sudden need, is capable of increasing the body’s ability to perform work functions by collecting possible resources.
As a result, the design carries out the work of organs such as the heart, reduces blood vessels, increases muscle capacity, frequency, strength of the heart rhythm, performance, and inhibits the secretory and absorption capacity of the gastrointestinal tract.
The SNS supports functions such as the normal functioning of the internal environment in an active position, coming into action during physical effort, stressful situations, illnesses, blood loss and regulates metabolism, for example, an increase in sugar, blood clotting, and others.
It is most fully activated during psychological shocks, through the production of adrenaline (enhancing the action of nerve cells) in the adrenal glands, which allows a person to react faster and more effectively to suddenly occurring factors from the outside world.
Adrenaline can also be produced when the load increases, which also helps a person cope with it better.
After coping with the situation, a person feels tired, he needs to rest, this is due to the sympathetic system, which has most fully used up the body’s capabilities, due to the increase in body functions in a sudden situation.
The parasympathetic nervous system performs the functions of self-regulation, protection of the body, and is responsible for human bowel movements.
Self-regulation of the body has a restorative effect, working in a calm state.
The parasympathetic part of the activity of the autonomic nervous system is manifested by a decrease in the strength and frequency of the heart rhythm, stimulation of the gastrointestinal tract with a decrease in glucose in the blood, etc.
By carrying out protective reflexes, it rids the human body of foreign elements (sneezing, vomiting, etc.).
The table below shows how the sympathetic and parasympathetic nervous systems act on the same elements of the body.

Top knot
Spindle-shaped formation measuring 20*5 mm. It is located on 2-3 cervical vertebrae (their transverse processes) under the prevertebral fascia.
Seven main branches depart from the node, which carry postganglionic fibers innervating the organs of the neck and head:
- Connecting gray rami to the 1st, 2nd, 3rd spinal cervical nerves.
- N. jugularis (jugular nerve) is divided into several branches, two of which are attached to the glossopharyngeal and vagus nerves, and one to
- N. caroticus internus (internal carotid nerve) enters the outer shell of the internal carotid artery and forms a plexus of the same name there, from which, in the area where the artery enters the canal of the same name on the temporal bone, sympathetic fibers depart, which form a stony deep nerve passing along the pterygoid canal in the sphenoid bones. After leaving the canal, the fibers pass and join the parasympathetic postganglionic nerves from the pterygopalatine ganglion, as well as the maxillary nerve, after which they are sent to the organs in the facial area. In the carotid canal, branches separate from the carotid internal plexus, which penetrate and form a plexus in the tympanic cavity. Inside the skull, the carotid (internal) plexus transforms into the cavernous, and its fibers spread through the vessels of the brain, forming the plexus of the ophthalmic, middle cerebral and anterior cerebral arteries. In addition, the cavernous plexus gives off branches that connect to the parasympathetic fibers of the parasympathetic ciliary ganglion and innervate the muscle that dilates the pupil.
- N. caroticus externus (carotid external nerve). It forms an external plexus near the artery of the same name and its branches that supply blood to the organs of the neck, face and dura mater of the brain.
- The pharyngeal-laryngeal branches accompany the vessels of the pharyngeal wall and form the pharyngeal plexus.
- The superior cardiac nerve passes near the cervical portion of the sympathetic trunk. In the chest cavity it forms the superficial cardiac plexus, which is located under the aortic arch.
- Branches that are part of the phrenic nerve. Their endings are located in the capsule and ligaments of the liver, pericardium, parietal diaphragmatic peritoneum, diaphragm and pleura.
Sacral section
The lowest section (according to the topography of the sympathetic trunk) is the sacral region, which consists of one unpaired coccygeal ganglion and four paired sacral ganglia. The nodes are located just medial to the sacral anterior foramina.
There are several branches of the sacral portion of the sympathetic trunk:
- Connecting gray branches heading to the sacral and spinal nerves.
- The splanchnic nerves are part of the autonomic plexuses in the pelvis. Visceral fibers from these nerves form the hypogastric inferior plexus, which lies on branches from the internal iliac artery, through which the sympathetic nerves penetrate the pelvic organs.
Lumbar
The lumbar ganglia of the sympathetic trunk are nothing more than a continuation of the chain of ganglia of the thoracic region. The lumbar region includes 4 nodes, which are located on both sides of the spine on the inner edge of the psoas major muscle. On the right side, the nodes are visualized outward from the vena cava inferior, and on the left - outward from the aorta.
The branches of the lumbar sympathetic trunk are:
- White connecting branches arising from the 1st and 2nd lumbar spinal nerves and approaching the 1st and 2nd ganglia.
- Gray connecting branches. They unite the lumbar ganglia with all lumbar spinal nerves.
- Internal lumbar branches that arise from all ganglia and enter the superior hypogastric, celiac, aortic abdominal, renal and superior mesenteric plexuses.
Middle node
A formation measuring 2*2 mm, located at the level of the 4th cervical vertebra, at the place where the common carotid and inferior thyroid arteries intersect. This node gives rise to four types of branches:
- Connecting gray branches that go to the 5th, 6th spinal nerves.
- The middle cardiac nerve, which is located behind the chest cavity, the nerve participates in the formation of the cardiac plexus (deep), which is located between the trachea and the aortic arch.
- Branches that participate in the organization of the nerve plexuses of the subclavian, common carotid and thyroid inferior arteries.
- The internodal branch that connects to the cervical superior sympathetic ganglion.