Maltseva Marina Arnoldovna
Neurologist of the highest category, specialist in the field of extrapyramidal pathologies, doctor of the highest category
Shabunina Ekaterina Mikhailovna
Neurologist, category 2
Impairments in coordination and gait, stability and balance are not diseases in themselves. These disorders are symptoms that occur in a wide variety of diseases.
Balance is regulated automatically by the vestibular and muscular system, so people don’t really think about how to maintain an upright position while walking, standing or sitting. As long as the muscular and vestibular apparatus work harmoniously and reliably, a person simply does not need to think about it. However, like all systems of the body, the vestibular apparatus can work with disturbances. It is in such cases that a person experiences coordination disorders and movement disorders. Coordination of movements allows a person to perform clear movements and consciously control them. When vestibular disorders occur, a person experiences unsteadiness when walking and instability of the torso.
If the patient has impaired coordination of movements, this indicates some changes in the functioning of the central nervous system. The human central nervous system is a complex formation of nerve cells that are located in the brain and spinal cord. At moments when a person wants to make a particular movement, a signal is sent from the brain, in response to which the person’s limbs, torso or other parts of the body begin to move. In cases where the central nervous system does not work properly, the signal from the brain is transmitted in a distorted form or does not reach its target at all.
There are quite a few factors that influence poor coordination of movements:
- various brain injuries;
- strokes;
- physical exhaustion of the body;
- sclerotic changes;
- parkinsonism;
- muscle dystrophy;
- exposure to alcohol, narcotic and other toxic substances;
Catalepsy is a fairly rare phenomenon. This is a disorder in which the muscles weaken due to strong positive or negative emotions experienced by the person.
Impaired coordination of movements is considered a dangerous deviation, since in a state where a person cannot adequately control his movements, it is quite easy to get injured.
Various movement disorders are often observed in old age. In addition, such deviations may be a consequence of previous neurological diseases or diseases of the musculoskeletal system.
There are several main manifestations of motor coordination disorders:
- Tremor, manifested by rhythmic shaking of the hands or head. This disorder can be almost unnoticeable at rest, and increase with anxiety.
- Uneven, shaky movements.
- Ataxia. This disorder is caused by damage to the frontal parts of the brain, nerve fibers or cerebellum. With static ataxia, it is difficult for a person to maintain balance in a standing position; with dynamic ataxia, it is difficult for him to move in a balanced manner.
If you experience any of the symptoms described above, you should contact a neurologist, cardiologist or toxicologist.
Clinical Brain Institute Rating: 3/5 — 34 votes
Share article on social networks
Signs of poor coordination
Loss of stability is classified according to the phases of movement and the expected diagnosis. Slow action, unstable body position are a common symptom of polyneuritis.
After the assessment, the interdisciplinary team sets goals in each area of rehabilitation. After treatment is completed, the patient's progress and functional evolution are assessed and reflected in a new report. This reset report records the current patient situation and changes made. If necessary, he should also indicate recommendations for the direction of cases. In addition to establishing a diagnosis and preparing a treatment plan, the assessment will allow us to prepare other reports.
A report may be required to determine the patient's ability to work, to follow a case, and to determine the characteristics of the patient's progress or the suitability of a particular therapeutic procedure or simply for research or investigational purposes.
Involuntary twitching (chorea) is a consequence of damage to the central nervous system after rheumatism or a symptom. Chaotic muscle contractions indicate a latent form of epilepsy. If the gait is unbalanced, the cerebellum and cerebral circulation are examined.
Symptoms of impaired motor coordination:
- profuse sweating;
- blood pressure surges;
- changes in breathing rhythm, skin color of the face and neck;
- movement coordination disorder;
- sudden attacks of nausea.
The altered state is accompanied by involuntary movements of the eyeball (nystagmus): vertical, rotary, transverse, diagonal. There is paroxysmal positional with the formation of the illusion of rotation of the external picture. Ringing in the ear signals problems with receptors in the peripheral region.
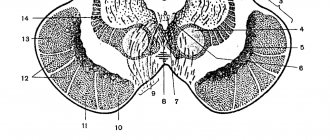
Uncoordinated movements are also known as lack of coordination, poor coordination, and loss of coordination. The medical term to describe this problem is ataxia. For most people, movements are smooth, coordinated and continuous. Walking, throwing a ball, or picking up a pencil involve movements that do not require any effort. However, in reality, each movement involves the action of several muscle groups, which are mainly controlled by the cerebellum. The cerebellum is an important structure of the brain.
Any change in communication between the brain and the rest of the body can cause ataxia. People with ataxia have clumsy and unsteady movements. Affected people may walk unsteadily or are prone to stumbling. In addition, they may have difficulty with daily activities involving mental motor skills, including simple tasks such as eating or using a pen. Ataxia can profoundly affect a person's life.
Intramuscular coordination training
If intermuscular coordination can be called the development of movement technique, then intramuscular coordination is correlated with the broader concept of the general physical training of an athlete. Therefore, the goal of training aimed at developing this type of coordination is the development of power potential to its maximum. Often, an intramuscular coordination training program is designed in such a way that an increase in strength occurs without gaining muscle mass. Mainly, the athlete is tasked with performing exercises at high speed in a short time, which stimulates the neuromuscular system. Thanks to this, the fastest activation of the maximum number of motor units occurs, that is, movements are performed with maximum frequency. The following will help achieve a similar effect:
- eccentric strength exercises, from which the muscle begins to lengthen under the influence of load, subject to submaximal tension. Jumping, performing exercises with both arms or legs at once in the contraction phase, or with one of the arms/legs in the muscle stretching phase are good options. They should be performed at a fast pace, with an intensity of 120 to 150%, in 3-5 approaches with 2-5 repetitions and a three-minute pause.
- concentric strength exercises are used to improve coordination of movements
, in which the muscle contracts, maintaining maximum tension. You can use in training: acyclic variations of jumps, exercises in interaction with a companion who takes part of the load on himself during the eccentric phase of movement. Exercises are performed with 100% intensity, at maximum pace, with 5 sets of 1-2 repetitions and a pause of 3 minutes.
- development of reactive strength, using cyclic and acyclic jumps, at an explosive pace, with an intensity of 120 to 150%, in 2-3 or 3-5 approaches, with 6-10 repetitions and a break of three minutes.
Of course, the optimal option for developing coordination would be to engage in a sport that activates two types of coordination at once: intramuscular and intermuscular, for example, CrossFit. The main thing is not to let your muscles adapt; this can be easily achieved by coming up with new variations of well-known exercises.
Don't miss interesting news and events in the telegram channel: https://tlgg.ru/fitbarnews
Causes of poor coordination
Loss of coordination and dizziness are sometimes associated with organic brain damage and neurotic conditions. Attacks are accompanied by diplopia (double image), bulbar signs (impaired functions of the medulla oblongata) lasting from a few minutes to several hours.
Causes related to diseases and injuries
Coordinated movements involve the combined action of the cerebellum, peripheral nerves, and spinal cord.
Diseases and injuries that damage or destroy any of these structures can cause ataxia. These include the following. Traumatic brain injury traumatic brain injury brain infection multiple sclerosis: a chronic condition that affects the course of an ischemic attack of the brain and spinal cord: a temporary decrease in blood supply to part of the brain congenital cerebellar ataxia: an inherited form of ataxia Friedreich's ataxia: an inherited disease that affects the muscles and heart. Wilson: a rare inherited disorder characterized by liver and nervous system damage caused by excessive increases in copper levels in the body cerebral palsy: a group of disorders caused by brain damage occurring in the early stages of paraneoplastic syndrome child brain tumors: a rare immune response to cancerous tumor neuropathy: a disease or damage to the nerve vertebral lesions of chickenpox. The toxic effects of certain substances can cause ataxia. Symptoms come on suddenly. The patient may experience respiratory and heart rhythm disturbances, impaired muscle sensitivity, swallowing and chewing. Predisposing factors may be:
- Strong smell;
- weather change;
- any irritating factor.
Causes of the disease
The movement problem is dangerous and serious for a patient with disabilities. Being in this state, a person is unable to coordinate his own actions.
The development of the disease is influenced by many factors. The following reasons are identified:
- Traumatic brain injury;
- Formation of tumors in the brain or cerebellum;
- Parkinson's disease;
- Changes in blood circulation in the brain;
- Cervical osteochondrosis;
- Muscular dystrophy;
- Stroke;
- Cerebral palsy;
- Intoxication due to improper use of medications;
- Gas poisoning;
- Autoimmune diseases (diabetes mellitus);
- Sclerotic changes in old age;
- Infectious diseases: meningitis, encephalitis;
- Taking narcotic drugs;
- Catalepsy is muscle relaxation due to a surge of emotions.
It is not difficult to identify the disease; the symptoms are visible to the naked eye. But to know exactly what they are, you need to familiarize yourself with the clinical picture.
Symptoms of ataxia
Typical imbalances are often caused by cerebellar lesions. It is difficult for the patient to remain in one position. When walking, he spreads his legs wide and swings his arms chaotically. In the severe stage, he cannot sit, stand, or hold his head up without assistance.
When should you see your doctor?
Alcohol anticholinergics phenytoin carbamazepine phenobarbital antidepressants tricyclic sedatives mercury, lead and other heavy metals toluene and other types of solvents.
The following list can help you determine whether you need to see your doctor for ataxia. This list is useful when a clear cause for ataxia cannot be determined. Call your doctor immediately if the following symptoms occur. Loss of balance difficulty swallowing lack of coordination that persists for several minutes lack of coordination in one or both legs, arms or hands difficulty speaking difficulty walking. The doctor will ask about your medical history and perform a physical examination. In addition, he will evaluate the functioning of the muscular and nervous systems. Your doctor will likely evaluate your ability to balance, walk, and point your fingers and toes. You may also be given the Romberg test, which is a very simple test in which you have to stand with your feet together, then close your eyes and see if you maintain your balance.
The vestibular form develops when one of the elements of the vestibular apparatus is damaged. Patients with encephalitis suffer. Main symptoms:
- sense of rotation of objects;
- motion sickness;
- nausea;
- loss of orientation, dizziness.
The cortical form develops when the function of the fronto-pontocerebellar system is impaired. In addition to typical manifestations, the psyche changes, the grasping reflex weakens, and odors disappear. Causes of the condition: abscesses, problems with cerebral circulation. They also distinguish between kinetic, sensitive, and static ataxia with subjective symptoms.
In addition, your doctor may ask you the following questions. Do you have other symptoms such as weakness, numbness or confusion?
- When did ataxia start?
- Is ataxia constant or sporadic?
- How severe is ataxia?
Your doctor may request the following tests.
Blood test urine test computed tomography magnetic resonance lumbar puncture genetic tests. However, in some cases, treating the underlying cause may relieve symptoms. In other cases, your doctor may recommend the use of adaptive devices or therapy.
Important! One of the dangerous symptoms is blockage of the auditory artery.
Thrombosis or embolism interferes with blood flow, causing severe pain, ataxia, noise, and loss of stability. With partial blockage, the patient suffers from high-frequency sounds.
The phenomenon is fraught with stroke and one-sided deafness. Attacks of Meniere's disease - dropsy of the endolymphatic space - are associated with impaired blood flow. Usually there is noise in anticipation of an attack. With chronic attacks, hearing decreases and the perception of individual sounds is difficult.
If ataxia is caused by a chronic disorder such as cerebral palsy, your doctor may not be able to treat it. The following adaptive devices may make life easier for patients with ataxia. Rods or utensils modified for the use of communication devices. With a number of simple changes in different parts of the home, people who have ataxia can cope better.
Make sure circulation areas are large enough to remove rugs and other objects that could cause slips, trips and falls. Avoid clutter. . Therapies that may be helpful include the following. Physiotherapy. . Acute immobility, understood as an episode of rapid decline in mobility over a period of at least three days, represents a true medical emergency and requires immediate attention, both for its functional prognosis and for the high mortality it carries with it, a 33% mortality rate in three month and 58% per year.
Vestibular neuritis occurs after infectious diseases. In addition to the classic symptoms, spontaneous rotatory nystagmus is observed with rotation of the eyes across and along the orbit. After treatment, the syndrome of incoordination disappears after 3 days.
After 60 years, vertebrobasilar insufficiency may develop. The disease is typical for people over 60. The causes of loss of balance are: cerebellar ischemia of the middle ear, problems with the vestibular nerve. Subjective signs: falls, nasal pronunciation of sounds, double vision.
The immobilized older adult is a patient at high risk for medical complications, requiring assistance with virtually all major activities of daily living and a candidate for admission to a geriatric residency. We cannot consider it normal and inevitable that all majors end up immobilized over the years.
If it's true that as you get older, there are a number of changes that limit mobility. Discrete muscle atrophy followed by fibrosis, so muscle contraction occurs more slowly. Muscle strength decreases by 15% over 30 to 70 years. Joints lose elasticity and ability to move. Changes in the vestibular systems that maintain balance. The center of gravity moves up and forward, making it difficult to maintain balance.
Treatment
Any condition in which a person cannot control his movements is dangerous, since the patient can injure himself if he falls. This disorder can cause disability. The main danger posed by impaired motor coordination is the disease that caused the symptom.
If you experience any of the symptoms described above, immediately make an appointment with a neurologist.
The human body is the most complex system imaginable. We don't think about how to take a step or clench our hand into a fist. But to ensure even the simplest movement, a whole cascade of reactions and interactions is needed, starting from awareness of the need to perform a particular action and to transmitting an impulse to the muscle. And all this is coordinated and controlled by the human nervous system. If at least one of the links fails, a violation of coordination of movements occurs, when a person loses the ability to perform precise processes, instability appears when walking, in severe cases the patient is unable to even get out of bed and needs constant assistance.
More often, problems with coordination are observed in people of older age groups. As the body ages, the activity of the nervous system slows down somewhat. In addition, with age, a certain “baggage” of diseases accumulates, which can cause impaired coordination of movements (discoordination). The most susceptible to pathology are people who have worked with small parts for many years, as well as people suffering from vascular pathology, with a history of injuries to the nervous system or musculoskeletal system, and abusing alcohol and drugs.
Causes of coordination problems in children
1. Early organic damage to the central nervous system, which can be caused by insufficient oxygen supply to the child’s brain during pregnancy, childbirth and after it.
2. Cerebral palsy.
3. Injuries to the nervous system and limbs (during childbirth, household injuries, car accidents).
4. Hereditary diseases (Friedreich's disease, Glippel-Lindau syndrome, Pelizaeus-Merzbacher demyelinating encephalopathy and others).
5. Infectious diseases and inflammatory processes of the brain and its membranes:
- encephalitis.
6. Intoxication:
- medicinal, as a result of the use of high doses of drugs;
- poisoning with carbon monoxide, heavy metals, chemical compounds;
- endogenous (hepatitis, severe viral or bacterial infection, kidney pathology).
In young children, it is impossible to detect the presence of coordination disorders. Pathology can be noticed only after the child learns to perform voluntary actions (pick up a toy, bring a spoon to his mouth).
Causes of coordination problems in adults
For adults, all of the above reasons are valid. But while in children most changes are congenital, in adults acquired diseases come to the fore:
1. Vascular pathology of the brain:
- stroke;
- atherosclerosis of cerebral vessels;
- encephalopathy.
2. Parkinson's disease.
3. Tumors.
4. Intoxication of the body:
- alcoholic;
- narcotic;
- hepatic as a result of cirrhosis;
- renal for acute or chronic renal failure.
5. Diseases and injuries of the musculoskeletal system.
Loss of coordination with dizziness
Often coordination disorders are accompanied by dizziness. This is a sign that the brain is involved in the pathological process, namely its vestibular center, which is responsible for the balance of the body in space. In addition to dizziness and incoordination, additional concerns may include:
- nausea, sometimes vomiting, sharply increasing when turning the head or any movements;
- pain and discomfort in the cervical spine;
- headaches, noise in the head;
- increased blood pressure.
Causes of poor coordination with dizziness:
- Stroke
in the veno-basilar region and other vascular pathology. - Cervical osteochondrosis
, in which there is a decrease in blood flow to the brain, and ischemia of its centers develops. - Meniere's disease
is a disease of the inner ear. - Hypertonic disease
. As pressure increases, the lumen of blood vessels decreases, which leads to disruption of the nutrition of the vestibular centers. - Tumors
, brain cysts.
Treatment for impaired coordination of movements
The key to success in the treatment of coordination disorders is finding out their cause. If it can be eliminated, coordination defects may completely disappear. But most processes are often irreversible; the development of some of them can be slowed down or suspended. In any case, when incoordination occurs, the nervous system is involved to one degree or another, so drugs to nourish neurons must be prescribed:
- nootropics (piracetam, emoxypine);
- neuroprotectors (cerebrolysin, cortexin, gliatilin);
- activators of cellular metabolism (Actovegin, Ceraxon).
In case of acute vascular pathology, immediate treatment is required in order to stop the process of neuronal death and minimize the consequences of the disaster. In other situations, therapy is carried out in courses 2-3 times a year and during exacerbations. In addition, in each specific case it is necessary to prescribe drugs aimed at the cause (antiparkinsonian, antihypertensive).
Congenital pathology and hereditary diseases are practically not amenable to drug correction, so symptomatic treatment is carried out. Physical therapy, which must be constant, is of great importance in restoring coordination problems. Physiotherapy methods, acupuncture, and massage are used.
Treatment of movement coordination disorders
Since problems of the vestibular system are caused by pathologies, it is necessary to eliminate the provoking cause. Treatment of coordination problems when walking begins with gymnastics. Movements help the vestibular system adapt to the existing pathology. The patient is asked to perform corrective exercises that irritate the receptors of the peripheral parts.
With repeated exercise, addiction occurs and the symptoms subside. To normalize blood circulation, the neurologist prescribes appropriate medications - Cinnarizine, Flunarizine, in severe cases - hormones, and massage is prescribed. However, it is not always possible to restore coordination.
(average rating: 5,00
out of 5)