General characteristics of the pathology
Childhood absence epilepsy (CAE) is a fairly common form of the disease, occurring in children under 18 years of age. Accounts for approximately 20% of cases of epilepsy in children. Most often, it first appears at the age of 3-8 years; girls are more predisposed to this pathology. In adults, the pathological process is rarely observed.
When performing an EEG, foci of epileptic activity are observed. Therefore, the disease is classified as a form of epilepsy, although it is accompanied by other symptoms. Parents should be attentive to their child in order to notice absence seizures in time. If treatment is not started, resistant forms of DAE may develop.
Prognosis and prevention
The course of absence epilepsy is favorable in most cases, remission occurs on average in 85% of patients. In children, this figure increases to 90-95%. At the same time, simple absence seizures are more treatable than complex ones.
If motor elements of the disease are added to the attacks, then correction requires more serious measures. In most cases, they can be corrected by introducing a combination of drugs for the treatment of epilepsy. People who have gotten rid of absence pathology should remember about constant relapse prevention:
- it is necessary to adhere to the daily routine, avoid changing the time of sleep and wakefulness;
- you need to limit the intake of stimulant drugs and drinks, food as much as possible: chocolate, caffeine, tea, carbonated drinks;
- in the future, work and human activity should not be associated with acute stress, extreme sports, or stress;
- physical, mental and psychological stress should be moderate;
- physical activity should be light to moderate: yoga, swimming, cycling. Professional sports are contraindicated;
- loud sounds, flashes of light, bright pictures and any flickering with constant exposure often provoke a severe form of epilepsy. Therefore, teenagers and young people should refrain from visiting clubs and discos.
Absence epilepsy is easy to treat in most cases, but people should be mindful of the risks of relapse. This is where the main danger lies, because in the case of repeated epilepsy it becomes more severe and the symptoms are less amenable to correction. This is why it is so important to lead a healthy lifestyle and eat well.
Causes
Most often, childhood absence epilepsy is associated with abnormal intrauterine development of the brain or damage to the fetal nerve cells in late pregnancy. Congenital diseases such as hydrocephalus, microcephaly and others can lead to the disease.
Another reason for the development of the disease is poor heredity. Therefore, if both parents suffer from any form of epilepsy, doctors do not recommend having children with them. In 90% of cases, the born baby will also be sick.
If the first manifestations of the disease appear in adolescence, the following factors may contribute to this:
- Mental overstrain. Epilepsy often develops in children who study very well.
- Increased physical activity. If a child has to do heavy work regularly, this can also cause instability of the central nervous system.
- Frequent stressful situations. For example, if parents constantly quarrel or demand more from the child than he can. Stress can also be caused by constant travel.
- Impaired metabolism.
- Insufficient blood circulation to the brain. Due to hypoxia, nerve cells may begin to die.
- Previously suffered traumatic brain injuries. They lead to disruption of the integrity of blood vessels and nerve endings. Gradually, foci of epileptic activity appear at the site of these pathological changes.
- Drug intoxication. All tablets for children should be given by adults. Otherwise, they may take an increased dosage of the medication.
Stress and mental strain are possible causes of absence epilepsy
All of the above factors can lead to instability of the mechanisms that regulate the ratio of inhibition and excitation processes in the cerebral cortex. As a result, convulsive readiness of neurons occurs, which leads to the appearance of foci of epileptic activity.
Causes of pathology
Childhood or juvenile absence epilepsy is an idiopathic disease, that is, one with no known cause. Scientific research suggests genetic prerequisites for development, but it is not possible to identify specific genes in patients. The following risk factors are called:
- traumatic brain injuries of any severity;
- infectious and non-infectious lesions of the brain and meninges;
- benign and malignant tumors growing within the central nervous system;
- prolonged mental or physical stress in childhood;
- hypoxic conditions of the brain that disrupt the functioning of nervous tissue.
The occurrence of absence seizures is also associated with provoking factors:
- frequent and deep breathing, leading to hyperventilation;
- insomnia and stressful situations;
- visual stimuli characterized by rapid changes in images - television, personal computers, etc.;
- intoxication with chemicals, including drugs.
These risk factors must be identified in the patient. Without eliminating them, it is difficult to achieve high effectiveness of treatment and a positive prognosis.
Kinds
Absence seizures can be simple or complex. With simple absence seizures, consciousness switches off briefly for 2-5 seconds, and there are no other symptoms. At the same time, the person may even continue to stand, but his gaze freezes.
Also, with absence epilepsy in children, complex absence seizures can be observed. They are accompanied by accompanying symptoms. They can occur with muscle relaxation, increased muscle tone, urinary incontinence and other symptoms.
In addition, typical and atypical absence epilepsy are distinguished separately.
Typical
Typical absence epilepsy in children is characterized by short seizures that begin suddenly and end quickly. The age of first manifestations varies from 9 months to 17 years, but is most often observed in the period of 0.9-4 years. With proper therapy, complete remission of the disease can be achieved in 85% of cases.
Atypical
Atypical absence seizures have the characteristics of generalized seizures, but according to the mechanism of development they are focal. Accompanied by disturbances of consciousness, changes in the motor activity of patients, and lethargy. They begin gradually and end the same way, which distinguishes them from typical absence seizures.
Common symptoms of epilepsy
Unlike many other types of epilepsy, absence seizures occur spontaneously and are not characterized by warning signs (auras). In rare cases, you can find out about an upcoming seizure by the following symptoms:
- Increasing headache;
- Increased sweating;
- Cardiopalmus;
- Nausea;
- Panic attacks;
- Excessive aggressiveness;
- Hallucinations (mainly sound and taste).
You can distinguish the attack itself from reverie by the following signs:
- Complete cessation of any activity;
- Fixed gaze;
- Lack of response to external stimuli.
After the child's seizure ends, he may continue talking or doing certain things he was doing previously without being aware of the momentary loss of consciousness. In the case of atypical forms, various spontaneous movements are added, which can be used to understand the presence of epilepsy.
Teachers should be especially vigilant during classes, since children with this pathology can be extremely absent-minded. Sometimes their handwriting deteriorates and there are gaps in their notebooks for no reason. It is unacceptable to shout at children for such changes, and the teacher should call the parents and advise them to examine the child.
The baby's parents should be no less attentive. Too frequent thoughtfulness in the form of freezing in one place should be a signal to go to the hospital. Indeed, if left untreated, childhood epilepsy can develop into other forms of pathology, which are characterized by seizures.
Absence seizures are accompanied by certain symptoms, the main one of which is a disturbance of consciousness for 10-20 seconds. Sometimes epilepsy occurs only with this symptom, but most patients have additional signs of a neurological disorder:
- blank stare or blinking with motionless eyes;
- short-term freezing of the patient, cessation of activity;
- interruption and slowing of speech if the patient spoke before the attack.

You can interrupt the attack verbally by addressing the person. After an absence seizure, there is no fatigue or weakness that is characteristic of generalized epilepsy. There is no inhibition or disorientation.
Typical and atypical absence seizures present differently. Simple ones, as already mentioned, are accompanied only by short-term loss of consciousness. The attack comes suddenly, nothing predicts it, there are no warning signs. It’s just that a child who was playing or was busy talking suddenly stops moving quickly, “turns to stone,” looks straight ahead, the facial muscles do not contract, so the child’s facial expression does not change throughout the entire attack. The child may not react in any way to external stimuli - voices, sounds, light. After about half a minute the condition returns to normal. The child does not remember the attack; for him, these half a minute seem to disappear from his life.
Such paroxysms can be repeated several times a day, and several times a month. At high frequency, typical attacks reach a frequency of several tens per day. Each lasts no more than half a minute, the child with his eyes open is in a detached state, external stimuli do not bring him out of the attack. Such typical seizures are marked on the electroencephalogram as a peak-wave with a certain frequency of 3 Hz.
With atypical absence seizures, the child not only loses consciousness during the attack, but other phenomena also occur, which are the same for a particular child every time. For example, with the same movements of the lips, tongue, some specific repetitive gesture, constant adjustment of the hairstyle. That is, the child continues the action even when unconscious, which is why such paroxysms often go unnoticed for a long time.
Very often, atypical absence seizures occur against the background of changes in muscle tone. The child can move his head back with his eyes rolling, or he can bend back and at the same time maintain balance due to the leg laid back. If the tone changes towards hypotonicity, a fall is still inevitable, since the muscles, regardless of the posture, quickly weaken.
Often such attacks are accompanied by taste, auditory or visual hallucinations. The child remembers the attack itself, but regards as something unusual what just happened to him and which he cannot explain.
Clinical manifestations
The disease debuts at 4-10 years, but its peak occurs at 3-8 years. Manifests itself in paroxysms with specific symptoms. During a simple seizure of childhood absence epilepsy, the following signs and symptoms may appear:
- The attack may begin suddenly. During it, the child freezes and becomes motionless.
- There is general inhibition - the baby does not respond to speech addressed to him.
- Immediately after the attack, the child cannot remember what happened to him. Even if he answered the questions posed by adults, he forgets about it.

Freezing of a child is one of the symptoms of absence epilepsy
During an attack there are no convulsive movements. It seems as if the child was simply thinking about something. This phenomenon does not last long - from a few seconds to minutes. After the attack there is no weakness or drowsiness. Simple absence seizures occur in approximately 30% of patients.
But complex attacks of childhood absence epilepsy are much more common. In this case, additional symptoms are observed:
- There is a tonic component, in which the child throws his head back and rolls his eyes.
- An atonic component is often observed, manifested by impaired sensitivity in the hands, due to which the baby cannot hold objects.
- Automatisms can also join. The following signs appear - smacking, licking lips, repeating sounds and words.
- The so-called attention deficit disorder may occur.
Simple and complex absence seizures are typical. Atypical ones are less common. During them, the child’s consciousness is gradually and partially lost. This lasts quite a long time - up to several minutes. And after the attack, the child looks exhausted and weak.
In childhood absence epilepsy, paroxysms are repeated very often - up to several dozen times a day. In the first year, there are only 2-3 attacks per day, and gradually their frequency increases. Despite this, such a disease is considered benign, since there are no neurological changes and the child’s intelligence is not impaired.
Types of absence epilepsy in children
Childhood absence seizures are divided into 2 forms according to the time of onset of the first symptoms:
- Children's (from 2 to 8 years);
- Youth (from 8 years and older).
The nature of the attacks is as follows:
- Simple absence seizures (typical);
- Complex (atypical).
The first variety usually lasts no more than 10 seconds. An attack is characterized by freezing in one place and lack of response to external stimuli. After its completion, the child continues to go about his business as if nothing had happened.
Atypical absence seizures can last up to 20-30 seconds and differ from typical seizures in the following manifestations:
- Sudden movement of the body;
- Strange gestures;
- Constant licking of lips and adjusting clothes;
- Throwing the head back;
- Movement of the tongue.
In the most severe cases, in addition to the listed symptoms, atypical absence seizures also manifest themselves in the form of a sharp bending of the body backwards. At the same time, the baby can make movements with his hands to normalize balance, but sometimes falls occur. Such seizures are quite noticeable and patients often realize that clouding of consciousness has occurred.
Features of absence epilepsy by age
At different ages, childhood absence epilepsy can occur differently and has specific features.
In childhood
Childhood absence epilepsy is the most favorable form. It makes its debut at 6-7 years of age and appears more often in girls. Mostly typical absence seizures are observed (in 35% of cases - simple, in 43% - complex, and in 22% of cases they are combined). The attacks occur mainly in the first half of the day and are repeated very often - up to several dozen times a day.
In adolescence
Absence epilepsy that occurs in adolescence is called juvenile. Unlike DAE, it has some features. The disease begins at a later age - at 8-14 years. In such patients, simple absence seizures predominate, occurring in 66% of cases.
With juvenile absence epilepsy, the frequency of attacks is lower - they are observed up to several times a day. In adolescence, the disease may appear due to changes in lifestyle, which can provoke various stressful situations. In addition, young men often imitate adults, adopting their habits - they start smoking and drinking. This can cause alcohol intoxication, which leads to disorders in the cerebral cortex, provoking epilepsy.
Diagnostic methods
To diagnose the disease, you need to consult a neurologist. The pathology is accompanied by fairly specific symptoms, so there are usually no difficulties in making a diagnosis. With DAE, the doctor asks the parents for symptoms, and with juvenile absence epilepsy, the doctor asks the child directly.
During the examination, the doctor reviews the patient's hospital records to see if there were any factors that might have contributed to the development of epilepsy (such as head trauma). The doctor also conducts special tests to determine whether the child’s intelligence corresponds to his age.

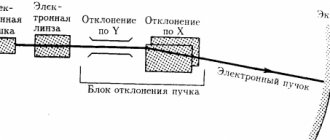
EEG is one of the methods for diagnosing absence epilepsy
The obligatory method is electroencephalography (EEG) - it is performed in 100% of cases. But sometimes the procedure does not show any changes in a normal state, but during an attack it is possible to record the pathological activity of the cerebral cortex in 90% of cases. Sometimes, on the contrary, foci of epileptic activity are detected, but there are no symptoms of the disease.
Other studies (CT, MRI) are not mandatory. But the doctor may prescribe them to exclude symptomatic epilepsy caused by tumors, cysts and infectious lesions of the brain.
Possible complications and consequences in childhood
If absence epilepsy has been diagnosed and doctors have prescribed adequate treatment, then in 80% of cases the disease disappears by 10-15 years. More precisely, attacks and additional symptoms of the disease disappear. But the risk of relapse in adulthood remains. In this case, the disease takes on a severe form, becomes generalized, and the patient experiences seizures and convulsions.
If not treated correctly, absence epilepsy progresses and soon develops into severe forms of the disease. Rarely, this type of epilepsy leaves complications in the form of mental impairment for life.
According to statistics, about 60% of patients with absence seizures achieve a positive effect with drug therapy. And as a result, they achieve final remission.
As a rule, attacks cease to occur in children after puberty, subject to therapy. If the prescribed medications do not produce results, then juvenile myoclonic epilepsy may appear. And sometimes in such cases even pharmacoresistance develops.
Then generalized attacks occur, which are characterized by a severe course.
Preventive measures against absence seizures:
- introduce the correct daily routine;
- eliminate as much as possible factors that provoke an attack (stress, hypothermia, bright light, etc.);
- the child should eat healthy food; if the doctor has prescribed a special diet, then you need to strictly adhere to it;
- There should be moderate physical and mental stress. If a child has epilepsy, this does not mean that motor activity needs to be completely limited;
- You should protect your child from too bright cartoons and computer games.
Parents should carefully monitor their child's behavior. If there are any changes, you should consult your doctor.
Treatment options
Treatment for absence epilepsy is aimed at eliminating seizures or reducing their frequency and intensity. Basically, drug therapy is prescribed. One antiepileptic drug is prescribed. At first, reduced dosages are selected, but they are gradually increased until the required dose is reached. The use of several drugs at once does not make sense, since this slightly increases the effectiveness of therapy: adding one more drug - by 10%, adding two drugs - by 15%.
In addition, the drugs may begin to interact with each other. This can lead not only to decreased effectiveness, but also to allergic reactions.

Absence epilepsy is treated with Topiramate
Succinimides are most often prescribed to children. Basic drugs (Carbamazepine) and new ones (Topiramate, Pregabalin and others) can also be used. Volproate is also effective for childhood absence epilepsy. They can also be prescribed if the type of epilepsy is not determined - they are suitable for all generalized forms.
The medications must be taken over a long period of time. Cancellation is recommended only after three years of remission. If infrequent seizures occur, it is best to wait 4 years of remission before stopping the medication.
Ketogenic diets
These are low-carb diets, but high in fat and protein. They represent the main dietary method of treating absence epilepsy in children. However, it is not recommended to include them in treatment if the disease is treated with valproic acid drugs. In addition, during therapy it is necessary to be regularly examined by a neurologist and nutritionist.
Neurosurgical methods
For absence epilepsy, neurosurgical methods are rarely used. The indication for surgery is a high probability that the disease will develop into a more severe form. Various surgical techniques may be used at the discretion of the treating physician.
Treatment of epilepsy in a child
Despite the mildness of the form, absence epilepsy requires mandatory medical intervention and treatment. In adults, the most common drug is ethosuximide, as well as valproic acid. The latest generation drug Lamotrigine is also used in children.
First aid for absence seizures is practically not required - they occur in a mild form. If a person becomes ill, you can open the window, free him from tight clothes and lay him on the bed.
If a child has had at least two attacks, then he needs to take drugs such as valproate (Convulex), phenobarbital or carbamazepine, as well as Topomax and Keppra.
Taking these drugs is long-term; regularity is very important; if regularity is not observed, attacks may recur.
Most often, one drug is enough to prevent seizures. Antiepileptic drugs cause decreased attention, drowsiness, and lower school performance, but in no case should they be canceled or skipped, because withdrawal can immediately cause an attack. Each attack pushes the child’s development back.
The drug Convulex is used under the control of valproic acid in the blood. If valproic acid in the blood is more than 100 mcg/ml, then the dosage of the drug cannot be increased; if it is less than 50 mcg/ml, then the therapeutic dosage has not been achieved and the dose must be increased.
If a child has had at least one attack, then for a month he is strictly prohibited from any massage, drugs that stimulate the central nervous system, as well as classes with a speech therapist.
In case of symptomatic epilepsy, the tumor is removed, after which the attacks completely stop.
A new method has also appeared in the treatment of epilepsy - stimulation of the vagus nerve. To do this, the patient is implanted with a special electrical device. Stimulation of the vagus nerve improves the patient's emotional state.
Forecast
Absence epilepsy can resolve on its own with age. However, it is necessary to regularly see a specialist and take special medications to avoid various complications.
This is a harmless form of the disease. It is not accompanied by seizures, so its mortality rate is very low.
Juvenile absence epilepsy does not tend to self-heal. However, if you follow medical recommendations, you can achieve almost complete remission.
Prevention
To prevent the disease in children:
- It is necessary to avoid stressful situations.
- You need to love your child and yell at him less.
- You can only give those medications that the doctor has prescribed, observing the exact dosage.
- You also need to ensure that the baby does not hit his head, and treat any infectious diseases in a timely manner.
Particular attention should be paid to the baby's diet. He should eat more fresh fruits and vegetables. The amount of sweets must be reduced, as excessive amounts of sugar can cause metabolic disorders.
Childhood epilepsy is a favorable form of the disease. Therefore, if such a diagnosis is made, there is no need to despair. Parental love and care will help the baby cope with the disease faster.
Impact of external factors
The following factors can provoke another attack:
- Excessive visual stress resulting from prolonged sitting at a computer, TV, telephone, etc.;
- Exposure to bright light or flickering light, for example, from garlands or at discos;
- Physical and mental overload;
- Stressful situations;
- Disturbed sleep rhythm;
- Sudden change of weather.
Lack of sleep or interrupted sleep. The body seems to be trying to make up for lost REM sleep, as a result of which the electrical activity of the brain changes and an attack may begin.
Stress and anxiety can contribute to attacks.
Medicines that stimulate the central nervous system (Ceraxon, Cerebrolysin) can cause an attack of epilepsy, as well as an increase in the dose of insulin due to hypoglycemia.
Any serious illness, such as pneumonia, can contribute to an attack.
An attack can also be triggered by flashing bright light, for example, when watching cartoons. There is so-called television epilepsy - this is a special state of photosensitivity, which is based on the movement of spots that make up the picture. Sensitive children may react to watching TV with an attack.
If your child has epiactivity on the EEG, but there are no seizures, then you need to keep in mind that under any stress factors, be it illness or hormonal changes, they may appear. And once you enter stable remission, you need to be prepared.