Toxoplasmosis on MRI of the brain Magnetic resonance imaging is a painless and informative way to study the brain. Layer-by-layer MR scanning allows you to examine in detail all parts of the organ and evaluate their structure. Using certain sequences, it is possible to study in detail the white and gray matter, blood vessels, and ventricular system.
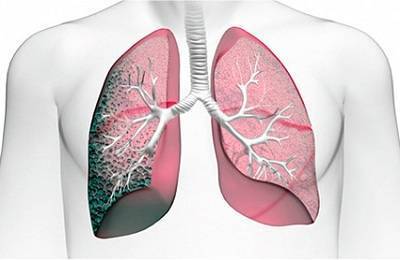
What are polymorphic lesions in the lungs?
If the doctor, based on the results of the examination, the patient’s complaints or other signs, suspects any pulmonary disease, it is likely that a CT scan of the chest organs will be prescribed. Let's consider the main indications for this study:
- the doctor suspects the presence of a formation in the lungs or in the area of the mediastinum, pleura;
- if the x-ray showed darkening of an unclear nature in certain areas of the lungs;
- for pneumonia, pulmonary tuberculosis;
- detection of a tumor in the lungs at the initial stage, if the patient has malignant cells in the sputum;
- after surgery to remove a cancerous tumor to identify a recurrent process.
There are many other indications for performing a CT scan of the chest. This is a very effective study; it is often prescribed after an x-ray if the image is uninformative.
What do lesions in the lungs look like on a CT scan?
Computed tomography of the chest allows you to diagnose many diseases. Based on its results, the specialist will be able to:
- make a more precise diagnosis;
- determine the localization of the process, its stage;
- prescribe effective treatment;
- monitor the dynamics of therapy by prescribing repeat tomography;
- assess the condition of the lungs, tissue density, appearance of the alveoli, measure tidal volume;
- consider most of the pulmonary vessels, pulmonary artery, superior vena cava, trachea, bronchi, lymph nodes.
In order for an ignorant person to be able to understand the results of a CT scan, one should know about the nuances of reading images. Let's look at the most relevant ones:
- Focal formations appear as white areas on a black background (in the negative image). In reality, the affected area is likely to be darker in color than healthy lung tissue.
- If the doctor notices areas of calcification or calcification (capsules impregnated with calcium salts) around the lesion in the image, this may be a sign of a benign formation. The calcifications are similar in color to the skeletal bones seen in this image. Such phenomena are often detected after prolonged colds, bronchitis or already cured tuberculosis and represent a kind of scar on the lungs. A patient with a formation that shows signs of calcification is usually asked by pulmonologists to take control images every six months.
- In the case where the formation is a so-called “cloud” or a “frosted glass” type lesion, a more detailed examination is required. Outwardly, it looks like a foggy area with blurred boundaries. In a number of countries, patients with such formations are immediately recommended to undergo surgery, even if it is not growing. It has already been proven that in 80% of cases such lesions are a precancerous condition of the lungs. An alternative to immediate surgery is constant monitoring with control images every six months to a year.
In conclusion, we note that there is no need to panic if the image shows changes in the lungs in the form of foci. More often, these phenomena turn out to be fibrous formations that do not require treatment. However, you should definitely undergo a full examination and consult with a pulmonologist to rule out more serious diseases.
It is typical that pathological formations may not manifest themselves in any way. Many patients do not complain - they have no cough, weakness, or chest pain.
A single lesion is defined as a compaction of lung tissue, the diameter of which is 1-10 mm. More often, changes in lung tissue are visualized in the following conditions:
- pneumonia;
- primary or chronic focal tuberculosis;
- pulmonary embolism;
- tumor diseases, their consequences (metastases, lymphogranulomatosis, reticulosis);
- swelling as a result of allergies;
- chest injuries, bleeding.
Subpleural lesions are limited areas of altered tissue located under the pleura, which is the lining of the lung. As a rule, this type of formation is invisible on routine fluorography or x-ray, but it is detected on CT.
Causes of subpleural lesions:
- tuberculosis;
- malignant formations;
- focal fibrosis.
Types of pathological foci in the lungs
Lesions that are found in the lungs are classified according to various criteria. First of all, in size:
- small – up to 2 mm;
- medium – up to 0.5 cm;
- large – up to 1 cm.
If the size of the lesion exceeds 1 cm, it is classified as another type of formation - infiltrate. The lesions are also systematized by density (dense, loose, medium density). Note that MSCT will help detect both small and loose lesions, which may not be available with radiography.
The structure of the lesion can be different - homogeneous, mixed with tubercles, with fatty or air inclusions. The listed signs are nonspecific and do not indicate any specific disease. The exception is the accumulation of fat cells in the lesion, which indicates a phenomenon such as hamartoma. This is a congenital benign formation that occurs on lung tissue.
The next type of classification of outbreaks is their number:
- Single areas of compaction (visualized from 2 to 6) may be a sign of a malignant tumor or represent typical age-related changes in the lungs (usually fibrous in nature).
- Multiple foci most often turn out to be symptoms of pneumonia or tuberculosis. However, in rare cases, lesions of more than six may indicate the development of oncology.
If pathology of the lower respiratory organs is suspected, the doctor will refer the patient for x-rays, tests and computed tomography. All these methods help to identify changes in the lung tissue and make an accurate diagnosis.
The advantages over other examination methods can be highlighted as follows:
- In a short time and with maximum accuracy, it is possible to determine what caused the disease. Lesions in the lungs are clearly visible on CT, and the doctor is able to determine their location and structure.
- Thanks to this type of examination, it is possible to determine at what stage the disease is.
- Helps give an accurate assessment of the condition of the lung tissue. Its density and condition of the alveoli are determined, in addition, the volume of the respiratory organs is measured.
- Thanks to CT, it is possible to analyze the condition of even the smallest vessels located in the lungs, as well as evaluate the aorta, heart, vena cava, trachea, bronchi and lymph nodes located in the chest.
Focal changes
Focal changes in the lungs can be of different sizes. Foci of small diameter 1-10 mm are detected in various diffuse pathologies of lung tissue.
Foci with high density and fairly clear edges are mainly observed in the interstitium of the lung.
Various low-density foci, resembling frosted glass, with unclear contours occur with pathological changes in the respiratory parts of the respiratory organs.
It should be taken into account that the density and size of the lesions have little diagnostic value. To make a diagnosis, the distribution of pathological processes in the lung tissue may be more important:
- Perilymphatic focus - often observed in the bronchi, vessels, interlobular septa and layers of the pleura. In this case, uneven contours of the anatomical structures are visible, while the septa and walls of the bronchi are somewhat thickened, as are the walls of the blood vessels. Similar pathological changes are often found in tuberculosis, silicosis, sarcoidosis and carcinomatosis. With these pathologies, the lesions are small and do not exceed 2-5 mm. Such foci consist of granulomas or metastatic nodules; they are observed along the lymph nodes in the lung tissue and pleura.
- Polymorphic focus. Such focal formations in lung tissue occur during tuberculosis. In this case, CT allows you to see areas of different densities and sizes. In some cases, such a picture is observed in oncological pathologies.
- Centrilobular lesions. Observed in the arteries and bronchi or in close proximity to them. They can be quite dense, well defined and uniform. Changes in lung tissue of this type are observed in pneumonia, endobronchial tuberculosis and various types of bronchitis, mainly of bacterial origin. There is another type of centrilobular lesions, in which case the lung tissue has small compactions and looks like frosted glass.
- Perivascular lesions are pathological formations that are located in close proximity to blood vessels. This condition is observed in oncological pathologies and tuberculosis. The lesions can be either single or multiple.
- Chaotically located foci. Such formations are characteristic of pathological hematogenous processes. This may be a hematogenous infection, tuberculosis or hematogenous metastases. Large multiple lesions, about 10 mm in size, are often observed with septic emboli, granulomatosis, fungal infections and metastases. All these diseases have some differences by which they can be differentiated.
- Subpleural lesions are pathologically changed areas located under the pleura. Observation of such areas in the image always indicates the development of tuberculosis or cancer.
- Pleural lesions. Such pathological formations are located on the pleura. Observed in inflammatory and infectious pathologies of the lower respiratory organs.
- The apical lesion is an excessive proliferation of fibrous tissue, which over time replaces healthy cells.
- Lymphogenic carcinomatosis. This concept includes two types of pathological changes in the lungs. On the right side there is alveolar infiltration, with visible lumens of the bronchi. On the left side, the density of the lung tissue is slightly increased. In the area of compaction, the walls of the bronchi and blood vessels are observed.
In focal diseases, areas of pathologically altered tissue can be different in size. They can be small, no more than 2 mm in size, medium - up to 5 mm in diameter, and large, the latter exceeding 10 mm in size.
Pathological foci can be dense, medium density, or loose. If single compactions are observed in the lungs, then this can be either an age-related change that does not pose a danger to humans, or a dangerous disease. If multiple foci are observed, then we are talking about pneumonia, tuberculosis or rare forms of cancer.
Focal changes in the lung tissue almost always indicate a pathological process. In most cases, doctors refer patients for a CT scan if the x-ray does not help make the correct diagnosis. Usually the diagnosis has already been made in advance and is only confirmed by the results of tomography.
Quite often, based on the results of a CT scan, a diagnosis of tuberculosis or lung cancer is made. For these diseases, it is very important to start therapy in a timely manner. At an early stage, these dangerous diseases respond well to treatment and the prognosis for patients is very good.
CT scanning also has its weaknesses. Thus, this method does not always allow us to see focal changes, the size of which is less than 5 mm and the tissue density is low. If the diameter of the lesion does not exceed 0.5 cm, then the chance of detecting it is about 50%. If the size of the changed area is about 10 mm, the chance of seeing it is equal to 95%.
In conclusion, health workers indicate the likelihood of developing a particular disease. The localization of the pathologically altered tissue does not play a role, but close attention is paid to the contours. If they are unclear and the lesions are more than 1 cm, then this always indicates a malignant process. If the edges are clear, we can talk about tuberculosis or benign neoplasms.
If the doctor has doubts when making a diagnosis, he may refer the patient for a computed tomography scan. This research method is quite accurate, but even with CT it is not always possible to see small focal changes in the lungs.
You may also like
Source: https://sarpages.ru/polimorfnye-ochagi-legkikh/
What are induced lesions in the lungs?
Lesions in the lungs on CT are local areas in which the transparency of the lung tissue is reduced. These may be areas of darkening or compaction of various sizes, which are detected during a computed tomography scan.
The cause of this pathological phenomenon can be various diseases of the respiratory organs. Despite the fact that CT is one of the most accurate diagnostic methods, it is impossible to make a diagnosis based on its results alone.
The patient must undergo a series of tests, which include blood and sputum tests.
Features of computed tomography
If pathology of the lower respiratory organs is suspected, the doctor will refer the patient for x-rays, tests and computed tomography. All these methods help to identify changes in the lung tissue and make an accurate diagnosis.
The advantages over other examination methods can be highlighted as follows:
- In a short time and with maximum accuracy, it is possible to determine what caused the disease. Lesions in the lungs are clearly visible on CT, and the doctor is able to determine their location and structure.
- Thanks to this type of examination, it is possible to determine at what stage the disease is.
- Helps give an accurate assessment of the condition of the lung tissue. Its density and condition of the alveoli are determined, in addition, the volume of the respiratory organs is measured.
- Thanks to CT, it is possible to analyze the condition of even the smallest vessels located in the lungs, as well as evaluate the aorta, heart, vena cava, trachea, bronchi and lymph nodes located in the chest.
Such a study helps to examine all segments in the lungs, due to which it is possible to reliably determine where exactly the pathological focus is localized.
Tomography is carried out in medical centers and the cost is quite high. However, if it is necessary to clarify the diagnosis, this procedure is simply irreplaceable.
Why are focal changes dangerous?
Focal changes in the lung tissue almost always indicate a pathological process. In most cases, doctors refer patients for a CT scan if the x-ray does not help make the correct diagnosis. Usually the diagnosis has already been made in advance and is only confirmed by the results of tomography.
Source: https://dyhanie-legkih.ru/legkie/indurirovannye-ochagi-v-legkih-chto-eto
Cases from blogs related to the head
Levin Russian Medical Academy of Postgraduate Education, Moscow Discirculatory encephalopathy is one of the main causes of the development of cognitive dysfunction in the elderly. Early recognition of this disease, including an adequate assessment of neuroimaging changes, complex therapy based on a modern understanding of the mechanisms of its development, can create conditions for curbing the progression of the pathological process and long-term improvement in the quality of life of patients. Key words: dyscirculatory encephalopathy, diagnosis, therapy. Pathology of white substance in dyscirculatory encephalopathy: diagnostic and treatment aspects O. Levin Russian Medical Academy for Postgraduate Training, Moscow Dyscirculatory encephalopathy is one of the main reasons for the development of cognitive dysfunction in the elderly.
Lesions in the lungs on CT - what they can be and what focal changes look like
CT is one of the modern and effective diagnostic methods. The essence of the procedure is that, using X-rays and a computer program, a layer-by-layer image of the desired organ is performed. An X-ray tube is fixed inside the tomograph.
During the session, part of the machine rotates around the patient and can take a thousand pictures per second. A computer program combines them into one picture and creates a three-dimensional image. A full cycle of examination of the chest organs is performed in 5-10 minutes.
Computed tomography is prescribed to study any organs and systems of the body. A tomogram of the chest organs (chest organs) is the most informative, because according to its results, the pulmonologist sees the bronchi, blood vessels in the lungs, the shape of the alveoli, the trachea and the size of the lymph nodes. Let's look at how the image is deciphered, what the lesions on the lungs mean, and let's understand their varieties.
In what cases is a lung CT performed?
If the doctor, based on the results of the examination, the patient’s complaints or other signs, suspects any pulmonary disease, it is likely that a CT scan of the chest organs will be prescribed. Let's consider the main indications for this study:
- the doctor suspects the presence of a formation in the lungs or in the area of the mediastinum, pleura;
- if the x-ray showed darkening of an unclear nature in certain areas of the lungs;
- for pneumonia, pulmonary tuberculosis;
- detection of a tumor in the lungs at the initial stage, if the patient has malignant cells in the sputum;
- after surgery to remove a cancerous tumor to identify a recurrent process.
There are many other indications for performing a CT scan of the chest. This is a very effective study; it is often prescribed after an x-ray if the image is uninformative.
What can a lung tomography image show?
Computed tomography of the chest allows you to diagnose many diseases. Based on its results, the specialist will be able to:
- make a more precise diagnosis;
- determine the localization of the process, its stage;
- prescribe effective treatment;
- monitor the dynamics of therapy by prescribing repeat tomography;
- assess the condition of the lungs, tissue density, appearance of the alveoli, measure tidal volume;
- consider most of the pulmonary vessels, pulmonary artery, superior vena cava, trachea, bronchi, lymph nodes.
Reasons for the appearance of subpleural foci in the lungs
It is typical that pathological formations may not manifest themselves in any way. Many patients do not complain - they have no cough, weakness, or chest pain.
A single lesion is defined as a compaction of lung tissue, the diameter of which is 1-10 mm. More often, changes in lung tissue are visualized in the following conditions:
- pneumonia;
- primary or chronic focal tuberculosis;
- pulmonary embolism;
- tumor diseases, their consequences (metastases, lymphogranulomatosis, reticulosis);
- swelling as a result of allergies;
- chest injuries, bleeding.
Subpleural lesions are limited areas of altered tissue located under the pleura, which is the lining of the lung. As a rule, this type of formation is invisible on routine fluorography or x-ray, but it is detected on CT.
Causes of subpleural lesions:
- tuberculosis;
- malignant formations;
- focal fibrosis.
Clinical picture, diagnosis and consequences
The healing process of the primary tuberculosis complex with the formation of a Ghon lesion is characterized by a long duration. As a rule, it is not affected by timely diagnosis and adequate chemotherapy.

Ghon's lesions in the lungs rarely manifest themselves clinically. During its formation, a person may experience:
- slight weakness;
- slight increase in body temperature for short periods of time;
- periodic dry cough.
More severe symptoms are observed in children. This is due to the imperfection of the immune response, which is manifested in the appearance of primary tuberculosis complexes and their simultaneous transition to the active process and focus of Gon. Therefore, most often such formations are diagnosed in a timely manner in young patients.
These include:
- plain radiography of the chest organs in two projections: frontal and lateral;
- computed tomography (CT);
- magnetic resonance imaging (MRI).
In X-ray studies, Hohn's lesion appears as a darkened oval (less often round) shape with sharp outlines, measuring up to 5 mm. Formations can be single or multiple. Their favorite localization is the lower and middle sections of the lungs. Sometimes the contours of the lesion may be uneven. The pulmonary pattern is unchanged, the root is not expanded.

At different stages of petrification (calcification) of the Gon lesion changes, its structure can be:
- homogeneous (homogeneous);
- inhomogeneous: has a granular or lobular structure, uneven boundaries.
Identifying a Gon's lesion on X-ray images is not difficult. However, due to the absence of clinical manifestations, it is often discovered by chance.
As a result of such studies, residual effects of perifocal inflammation, caseous masses, and changes in the lymph nodes can be detected. Such examinations are prescribed if a relapse of tuberculosis is suspected in the case of a completely unformed focus of Gon.
Complications after identifying this pathology are very rare. With a large number of Gon lesions and their large sizes (for example, after disseminated tuberculosis), the following may develop:
- fibrosis and cirrhosis of the lung;
- relapse of tuberculosis infection;
- displacement of mediastinal organs.
Such conditions lead to disruption of the normal functioning of the lungs, which is accompanied by the development of respiratory failure.
The identified pathology does not require any specific therapy. The doctor can give general recommendations:
- to give up smoking;
- in case of harmful production factors affecting the condition of the lungs, transfer to another job;
- walks in the open air;
- breathing exercises;
- swimming in the pool.
People with a Ghon lesion identified in the lungs are advised to undergo annual X-ray examinations to assess the dynamics of the process. It is advisable to undergo such examinations in the same place with one doctor. The focus of Gon is not a death sentence and is not a sign of developing tuberculosis. It only indicates that the infection has been defeated by the body.
Lesions in the lungs: what they can be and how they affect the body
Focal formations in the lungs are tissue compactions, which can be caused by various ailments. Moreover, to establish an accurate diagnosis, a doctor’s examination and radiography are not enough. The final conclusion can be made only on the basis of specific examination methods, including blood tests, sputum tests, and tissue puncture.
Important: the opinion that only tuberculosis can be the cause of multiple focal lung lesions is erroneous.
We can talk about:
- malignant neoplasms,
- pneumonia,
- disorders of fluid exchange in the respiratory system.
Therefore, diagnosis must be preceded by a thorough examination of the patient. Even if the doctor is sure that a person has focal pneumonia, it is necessary to perform a sputum analysis. This will identify the pathogen that caused the development of the disease.
Now some patients refuse to undergo certain specific tests. The reason for this may be reluctance or inability to visit the clinic due to its distance from the place of residence, or lack of funds. If this is not done, then there is a high probability that focal pneumonia will become chronic.
What are foci and how to identify them?
Now focal formations in the lungs are divided into several categories based on their number:
- Singles.
- Single – up to 6 pieces.
- Multiple – dissemination syndrome.
There is a difference between the internationally accepted definition of what lung lesions are and what is accepted in our country. Abroad, this term refers to the presence of areas of compaction in the lungs of a round shape and a diameter of no more than 3 cm. Domestic practice limits the size to 1 cm, and the remaining formations are classified as infiltrates, tuberculomas.
Important: a computer examination, in particular tomography, will allow you to accurately determine the size and shape of the lesion in the lung tissue. However, it is necessary to understand that this examination method also has its own error threshold.
In fact, a focal formation in the lung is a degenerative change in the lung tissue or the accumulation of fluid (sputum, blood) in it. Correct characterization of single pulmonary lesions (SLP) is one of the most important problems of modern medicine.
The importance of the task lies in the fact that 60-70% of such formations that were cured, but then reappeared, are malignant tumors. Among the total number of AOLs identified during MRI, CT or radiography, their portion is less than 50%.
An important role here is played by how lesions in the lungs are characterized on CT. Using this type of examination, based on characteristic symptoms, the doctor can make assumptions about the presence of serious diseases such as tuberculosis or malignant neoplasms.
However, to clarify the diagnosis, additional tests are necessary. A hardware examination is not enough to issue a medical report. Until now, everyday clinical practice does not have a unified algorithm for differential diagnosis for all possible situations. Therefore, the doctor considers each case separately.
Tuberculosis or pneumonia? What can prevent, with the modern level of medicine, from making an accurate diagnosis using the hardware method? The answer is simple - imperfect equipment.
In fact, when undergoing fluorography or radiography, it is difficult to identify OOL, the size of which is less than 1 cm. Interposition of anatomical structures can make larger lesions practically invisible.
Therefore, most doctors advise patients to give preference to computed tomography, which makes it possible to view tissue in section and from any angle.
This completely eliminates the possibility that the lesion will be obscured by the cardiac shadow, ribs, or roots of the lungs.
That is, radiography and fluorography simply cannot consider the whole picture as a whole and without the possibility of a fatal error.
It should be taken into account that computed tomography can detect not only AOL, but also other types of pathologies, such as emphysema and pneumonia. However, this examination method also has its weaknesses. Even with a CT scan, focal formations may be missed.
This has the following explanations for the low sensitivity of the device:
- The pathology is in the central zone – 61%.
- Size up to 0.5 cm – 72%.
- Low fabric density - 65%.
It has been established that with a primary screening CT scan, the probability of missing a pathological change in tissue, the size of which does not exceed 5 mm, is about 50%.
If the diameter of the lesion is more than 1 cm, then the sensitivity of the device is more than 95%. To increase the accuracy of the obtained data, additional software is used to obtain 3D images, volumetric rendering and maximum intensity projections.
Anatomical features
In modern domestic medicine, there is a gradation of lesions based on their shape, size, density, structure and condition of the surrounding tissues.
An accurate diagnosis based on CT, MRI, fluorography or radiography is possible only in exceptional cases.
Usually in the conclusion only the probability of the presence of a particular disease is given. In this case, the location of the pathology itself is not given decisive importance.
A striking example is the presence of a lesion in the upper lobes of the lung. It has been established that this localization is characteristic of 70% of cases of detection of a primary malignant tumor of this organ.
However, this is also typical for tuberculous infiltrates. With the lower lobe of the lung there is approximately the same picture.
Here, cancer that has developed against the background of idiopathic fibrosis and pathological changes caused by tuberculosis are detected.
Great importance is given to the contours of the lesions.
In particular, a fuzzy and uneven outline, with a lesion diameter of more than 1 cm, signals a high probability of a malignant process.
However, if clear margins are present, this is not sufficient reason to stop diagnosing the patient. This picture is often present in benign neoplasms.
Particular attention is paid to tissue density: based on this parameter, the doctor is able to distinguish pneumonia from scarring of lung tissue, for example, caused by post-tuberculosis changes.
The next nuance is that CT allows you to determine the types of inclusions, that is, determine the structure of the OOL. In fact, after an examination, a specialist can tell with high accuracy what kind of substance accumulates in the lungs. However, only fatty inclusions make it possible to determine the ongoing pathological process, since all the others do not belong to the category of specific symptoms.
Focal changes in the lung tissue can be provoked by both a fairly easily treatable disease - pneumonia, and more serious ailments - malignant and benign neoplasms, tuberculosis. Therefore, it is important to identify them in a timely manner, in which a hardware examination method - computed tomography - will help.
Loading…
Source: https://prof-medstail.ru/bolezni-legkih/simptomy-i-lechenie/obrazovanie-ochagov-v-legochnoj-tkani
Lesions in the lungs are subpleural and polymorphic - what could they be - Website about hernias and their treatment
The density of lung tissue in the basal segments may decrease to –900…–950 HU, which indicates the development of emphysema.
Emphysematous bullae can also form in the upper lobes along the surface of the costal, mediastinal and interlobar pleura. They lead to the displacement of foci and infiltrates in the central pulmonary tissue, to the root of the lung.
In the final stage, these changes can be defined as “honeycomb lung” (Fig. 8).
Rice. 8. High-resolution CT. The outcome of chronic hematogenously disseminated tuberculosis is in the “honeycomb lung” with fibrosis and a large number of polymorphic foci on both sides.
-11-
Lymphogenic tuberculosis disseminations are distinguished by features on the basis of which their pathogenetic mechanism of development can be assumed. These include the predominance of focal rashes (usually miliary) in the middle sections, at the level of the roots, and their lesser severity in the apical and basal segments of the lungs.
The greatest changes are localized in the anterior and posterior segments of the upper lobes, in the apical segments of the lower lobes, as well as in the lingular segments and middle lobe. Another distinctive sign of the lymphogenous nature of dissemination is the unevenness of lung damage with alternation of altered and normal areas.
In this case, the location of the foci and the predominance of interstitial changes correspond to the boundaries of a certain deep or superficial lymphatic collector.
In most cases, the deep lymphatic network of the lung is involved in the pathological process, as a result of which changes are localized deep in the lung tissue, along the vessels and bronchi (Fig. 9).
Rice. 9. High-resolution CT. Lymphogenic disseminated tuberculosis. On both sides there are multiple small foci against the background of interstitial changes. The distribution of foci in the lung tissue is uneven, with predominantly the deep lymphatic network involved in the pathological process (arrows).
In each lobe, one or several isolated areas of focal compaction of the lung tissue of irregular shape can be identified, with a wide base facing the pleura and an apex towards the root of the lung. Fuzzy outlines of blood vessels, Kerley lines in combination with magnification
-12-
venous lymph nodes of the roots of the lungs and mediastinum, as well as signs of lymphogenous dissemination.
In those cases where pathological changes are located predominantly in the cortical parts of the lungs, at the border of the superficial and deep lymphatic networks, the lesions are located in the form of a wide strip along the chest wall and mediastinum. At the same time, the deep and hilar sections of the lungs remain little changed.
FOCAL TUBERCULOSIS
Focal pulmonary tuberculosis is characterized by the presence of a few foci, mostly productive, in a limited area and occupying 1-2 segments of one or both lungs.
It includes both recently emerged, fresh processes with focal sizes less than 10 mm, and older (fibrous-focal) formations, but with clearly expressed signs of process activity.
The use of CT is necessary in cases where, with a conventional X-ray tomographic examination, the presence of foci is doubtful or it is not possible to assess their nature in detail. The lesions are located in the respiratory section and in the depths of the lung tissue peribronchially.
Their typical localization is the apical and posterior segments of the upper lobe, less often in the apical segment of the lower lobe. More often, the lesions are polymorphic in nature, typically a combination of one or two large lesions with a large number of small and medium ones (Fig. 10).
Fig. 10. High resolution CT. In the upper lobe of the left lung there are polymorphic foci with unclear contours, some of them merge with each other (arrow).
-13-
The lesions usually have a homogeneous structure; in the center of some large ones, transverse lumens of the bronchi may be visible, which differ from the cavities of destruction by the correspondence of the size of the clearing to the caliber of the bronchi of the same order on axial images and by a change in shape during reconstructions. True cavities in the lesions are larger in size, eccentric in location, and can only be detected with high-resolution CT. When the tuberculosis process intensifies, the contours of large lesions become uneven and unclear, small lesions with a diameter of 1-3 mm are located around. They are localized mainly in the walls of the secondary pulmonary lobes and intralobular septa (interlobular septa). The development of lymphostasis leads to thickening and compaction of these interstitial structures, increasing the density of lung tissue during densitometry.
Rice. 11. High-resolution CT. Targeted reconstruction of the right lung. In S 1-2, polymorphic foci tend to merge and have unclear contours, in some with a subpleural location there are small cavities of decay (arrow).
Long-term course of focal tuberculosis, especially against the background of antibacterial therapy, leads to a significant change in the computed tomographic picture. Along with focal changes in the lung tissue, areas of panlobular and paraseptal emphysema, small emphysematous bullae, as well as fibrous linear cords appear, directed from the area of pathological changes to the pleura.
-14-
Rice. 12. High-resolution CT. Targeted reconstruction of the left lung. Focal tuberculosis, chronic course. Large lesions with clear contours against the background of areas of swelling of the lung tissue (arrows).
The volume of the affected segments gradually decreases due to the development of local pneumosclerosis. In resolving the issue of the duration of the tuberculosis process, high-resolution CT has significant advantages over conventional x-ray examination.
Objective measurement with a cursor of a decrease in the size of large lesions, the disappearance or reduction in the number of small lesions during dynamic observation, indicate the positive dynamics of the pathological process.
The outcome of focal tuberculosis in most patients is the formation of small linear scars, inclusions of lime in the lesions, cavities of bullous emphysema and local thickening of the costal pleura.
In contrast to the initial changes, there are no small foci in the interstitium of the walls of the lobules, which is important for determining the activity of the tuberculosis process.
Source:
Lesions in the lungs: what they can be and how they affect the body
Focal formations in the lungs are tissue compactions, which can be caused by various ailments. Moreover, to establish an accurate diagnosis, a doctor’s examination and radiography are not enough. The final conclusion can be made only on the basis of specific examination methods, including blood tests, sputum tests, and tissue puncture.
Important: the opinion that only tuberculosis can be the cause of multiple focal lung lesions is erroneous.
We can talk about:
- malignant neoplasms;
- pneumonia;
- disorders of fluid exchange in the respiratory system.
Therefore, diagnosis must be preceded by a thorough examination of the patient. Even if the doctor is sure that a person has focal pneumonia, it is necessary to perform a sputum analysis. This will identify the pathogen that caused the development of the disease.
Now some patients refuse to undergo certain specific tests. The reason for this may be reluctance or inability to visit the clinic due to its distance from the place of residence, or lack of funds. If this is not done, then there is a high probability that focal pneumonia will become chronic.
Questions about diseases
The general name for a set of syndromes of various, functionally significant structures of the frontal lobe of the cerebral hemispheres. From the point of view of topical diagnostics, the frontal lobe is divided into the following sections: In addition, the characteristics of the neurological syndrome are influenced by the law on the functional asymmetry of the cerebral hemispheres; the syndromes of the left and right hemispheres have significant differences. In accordance with this law, right-handed people:. Occurs when Brodmann's fields 6, 8 and 44 are affected, uniting, as it were, three independent subsyndromes: There are 4 clinical variants of motor aphasia. Occurs when 9, 45, 46 and 47 Brodmann fields are affected.