Maltseva Marina Arnoldovna
Neurologist of the highest category, specialist in the field of extrapyramidal pathologies, doctor of the highest category
Shabunina Ekaterina Mikhailovna
Neurologist, category 2
Temporal lobe lesions are brain injuries that in most cases are not accompanied by any characteristic or severe symptoms.
With damage to the temporal lobes, the following deviations may be observed:
- neurological disorders;
- epileptic seizures
- psychopathological and neuropsychiatric disorders.
Neurological disorders may manifest as homonymous loss of visual pathways. With unilateral brain damage, any serious impairment of hearing or smell is usually not detected. With various lesions in the temporal lobes of the brain, the patient may experience impaired coordination of movements. In some cases, involuntary choreoathetoid movements are observed.
In addition, patients with lesions in the temporal lobes may experience psychomotor epileptic seizures. In some cases, paroxysmal auditory, olfactory or gustatory hallucinations are observed.
It is worth noting that with lesions in the temporal lobes, patients may experience both psychological and neuropsychological disorders. For example, patients may experience impaired attention or may suffer from verbal memory. The patient may subsequently suffer from bouts of irritability and other mood disorders. There is also a disturbance in the sense of time and a decrease in musical abilities.
Clinic of damage to the temporal lobe.
General cerebral symptoms in VDP are not fundamentally different from those with damage to other lobes of the brain (they are described in detail in the article “Frontal lobe damage”): quantitative changes in consciousness from moderate stupor to deep coma; headache with nausea, dizziness, vomiting; congestion in the fundus; psychomotor outbursts, etc.
Among the local signs of VDP, the phenomena of sensory aphasia dominate - from difficulty understanding complex turns of addressed speech to the complete loss of analysis of both audible and one’s own speech, which is figuratively referred to as “verbal okroshka”. In intermediate degrees of sensory aphasia, literal and verbal paraphasias are observed; tests of auditory-speech memory, alienation of the meaning of words, recognition and reproduction of similar-sounding phonemes in syllables and words help. With damage to the angular gyrus, located at the junction with the parietal and occipital lobes, i.e., the zone that integrates auditory, visual and sensory afferentation, the phenomena of alexia, agraphia, and acalculia develop. The described symptoms are observed with VDP of the dominant, usually left, hemisphere. Damage to similar zones of the subdominant (right) hemisphere causes a violation of the recognition and reproduction of “primary signal” sounds - household, street, natural noises, as well as familiar melodies, intonation and emotional structure of speech, which can be checked if the general condition of the victim allows.
Damage to the posterior third of the inferior temporal gyrus causes the development of amnestic aphasia, although this symptom after TBI can also act as a general cerebral one, especially in older people.
Deep traumatic processes (hematomas, contusion lesions) cause contralateral homonymous hemianopsia: lower quadrant - with selective damage to the visual pathway running above the lower horn of the lateral ventricle, and upper quadrant - when this path is damaged under the lower horn.
A whole range of symptoms can occur with damage to the medial part of the VD, which develops not only during the primary traumatic impact, but also as a result of herniation into the tentorial opening of the gyrus near the seahorse with its hook in the case of a volumetric increase in the VD. Irritation of the ancient cortex causes disruptions in the regulation of visceral and autonomic functions, which is manifested by both subjective (feelings of heaviness, discomfort, weakness, heart palpitations, heat, etc.) and objective symptoms (heart rhythm disturbances, angiotic attacks, flatulence, hyperemia or pallor of the integument, etc.). The background of the patient’s mental state changes in the form of a predominance of negative emotions, often of the type of constrained depression. Along with this, paroxysms of fear, anxiety, melancholy, and foreboding may occur. The most noticeable to the patient are disturbances of taste and smell in the form of perverted perception and deception.
Medial temporal injuries in TBI often manifest exclusively as epileptic seizures or their equivalents. The latter may include olfactory and gustatory hallucinations, sensory-visceral paroxysms, vestibular attacks, states of “previously seen”; Classic “streams of memories” are relatively rare in temporal lobe epilepsy. Epileptic discharges are also possible when the convexital sections of the VD are damaged; then simple or complex (with extended speech) auditory hallucinations act as equivalents or auras.
Secondary stem symptoms are woven into the clinical picture of UDP more than with any other localization. Basically, we are talking about dislocations of the oral part of the trunk in cases of increasing the volume of the VD - with massive edema, hematomas, cysts of traumatic origin. The diencephalon and midbrain are displaced contralaterally from the pathological focus, are injured on the opposite edge of the tentorium, and secondary dysgemia often develops in the brainstem and axonal damage to the conduction systems. Acute displacements and deformation of the trunk at the time of TBI are extremely life-threatening. With subacute or slowly growing dislocations, there are more opportunities for therapeutic measures; the doctor’s increased attention to the dynamics of brainstem symptoms is necessary (see the article “Midbrain syndrome in TBI”). A number of vegetative and visceral disorders of the same type as medial-temporal disorders occur when diencephalic structures are displaced, and disturbances in sleep rhythm, thermoregulation, and vascular microcirculation are also observed; hormetonic convulsions develop. Of the secondary symptoms in VDP, the pons and medulla oblongata syndromes and craniobasal symptoms are less common and less pronounced.
Anatomy
Lobes of the cerebral hemispheres
The cerebral cortex covers the surface of the hemispheres and forms a large number of grooves of varying depth and length (lat. sulci cerebri). Between the grooves there are cerebral gyri of varying sizes (lat. gyri cerebri) [5].
In each hemisphere the following surfaces are distinguished:
- convex superolateral surface (lat. facies superolateralis), adjacent to the inner surface of the bones of the cranial vault
- the lower surface (lat. facies inferior), the anterior and middle sections of which are located on the inner surface of the base of the skull, in the area of the anterior and middle cranial fossae, and the posterior ones - on the tentorium of the cerebellum
- the medial surface (lat. facies medialis), directed towards the longitudinal fissure of the brain [5].
These three surfaces of each hemisphere, passing one into another, form three edges. The superior edge (lat. margo superior) separates the superolateral and medial surfaces. The inferolateral edge (lat. margo inferolateralis) separates the superolateral surface from the bottom. The inferomedial edge (lat. margo inferomedialis) is located between the lower and medial surfaces [5].
https://www.youtube.com/watch?v=ytcopyrightru
In each hemisphere, the most prominent places are distinguished: in front - the frontal pole (Latin polus frontalis), in the back - the occipital pole (Latin polus occipitalis), and on the side - the temporal pole (Latin polus temporalis) [5].
The hemisphere is divided into five lobes. Four of them are adjacent to the corresponding bones of the cranial vault:
- frontal lobe (lat. lobus frontalis)
- parietal lobe (lat. lobus parietalis)
- occipital lobe (lat. lobus occipitalis)
- temporal lobe (lat. lobus temporalis)
- insular lobe (lat. lobus insularis) (islet) (lat. insula) - is located deep in the lateral fossa of the cerebrum (lat. fossa lateralis cerebri), separating the frontal lobe from the temporal lobe [5].
In the book by Godefroy J. “What is Psychology,” the sixth lobe, the corpus callosum, is highlighted, located on the inner side of the hemisphere under the corpus callosum. [6]
Diagnosis of damage to the temporal lobe.
VDP is based on an analysis of the mechanism of TBI, a combination of primary focal and secondary cerebral symptoms. It must be remembered that in the conditions of emergency diagnosis of TBI, the doctor often fails to recognize damage to the right (subdominant) AC, and the presence of general cerebral and brainstem symptoms can generally lead the diagnosis down the wrong path. Here, invaluable help is provided by the use of modern imaging methods such as CT and MRI, and in their absence, echoencephalography. X-rays of the skull and EEG retain their value. Lumbar puncture should be performed with maximum precautions (danger of herniation!). If you suspect the formation of a hematoma, you should refrain from lumbar puncture.
Histology
Structure
Cytoarchitecture (cell arrangement)
- molecular layer
- outer granular layer
- layer of pyramidal neurons
- inner granular layer
- ganglion layer (inner pyramidal layer; Betz cells)
- layer of polymorphic cells
Myeloarchitecture (arrangement of fibers)
- molecular layer strip
- strip of outer granular layer
- strip of inner granular layer
- strip of the ganglion layer [7].
The cerebral cortex is represented by a layer of gray matter with an average thickness of about 3 mm (1.3 - 4.5 mm). It is most strongly developed in the anterior central gyrus. The abundance of furrows and convolutions significantly increases the area of gray matter in the brain. The cortex contains about 10-14 billion nerve cells.
Its various sections, which differ from each other in certain features of the location and structure of cells (cytoarchitectonics), the arrangement of fibers (myeloarchitectonics) and functional significance, are called fields. They represent places of higher analysis and synthesis of nerve impulses. There are no sharply defined boundaries between them. The cortex is characterized by an arrangement of cells and fibers in layers [8].
Typical of the new cortex (lat. neocortex) is the presence of six layers, differing from each other mainly in the shape of the nerve cells included in them. At the same time, on the medial and lower surfaces of the hemispheres, sections of the old (lat. archipallium) and ancient (lat. paleopallium) cortex, which has a 2-layer and 3-layer structure, have been preserved [1].
Cytoarchitecture
Multipolar neurons of the cerebral cortex are very diverse in shape. Among them are:
- pyramidal
- stellate
- fusiform
- arachnids
- horizontal
Pyramidal neurons constitute the main and most specific form for the cerebral cortex (80-90% of all neurons). Their sizes vary from 10 to 140 microns. They have an elongated triangular body, the apex of which faces the surface of the bark. Dendrites extend from the apex and lateral surfaces of the body, ending in various layers of gray matter.
https://www.youtube.com/watch?v=ytpolicyandsafetyru
Pyramidal cells of different layers of the cortex differ in size and have different functional significance. Small cells are interneurons, the axons of which connect individual areas of the cortex of one hemisphere (associative neurons) or two hemispheres (commissural neurons). These cells are found in varying numbers in all layers of the cortex.
The neurons of the cortex are located in vaguely delimited layers. Each layer is characterized by the predominance of one type of cell. There are 6 main layers in the motor cortex:
- Molecular (lat. lamina molecularis)
- External granular (lat. lamina granularis externa)
- Pyramidal neurons (lat. lamina pyramidalis)
- Internal granular (lat. lamina granularis interna)
- Ganglionic (layer of Betz cells) (lat. lamina ganglionaris)
- Layer of multiform (polymorphic) cells (lat. lamina multiformis) [8]
The cerebral cortex also contains a powerful neuroglial apparatus that performs trophic, protective, supporting and delimiting functions [8].
On the medial and lower surface of the hemispheres, sections of the old, ancient cortex have been preserved, which have a two-layer and three-layer structure.
Treatment of damage to the temporal lobe.
Depressed fractures, supra- and intrathecal hematomas of temporal localization require surgical intervention as soon as the diagnosis is established. The operation should be performed for large intracerebral hematomas (maximum diameter <4 cm) and foci of contusion softening with a volume not only of over 50 cm3, but also for smaller ones if they are combined with cerebral edema and cause significant displacement of the brainstem. In the absence of threatening clinical symptoms and instrumental data, a patient with UDP should be prescribed dehydrating, sedative, vasoactive, anticonvulsant, anti-inflammatory and other types of therapy depending on the indications.
Parietal
In order to understand the functions of the parietal lobes, it is important to understand that the dominant and non-dominant side will do different jobs.
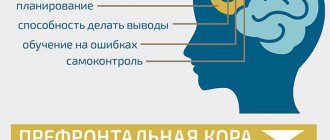
The dominant parietal lobe of the brain helps to understand the structure of the whole through its parts, their structure, order. Thanks to her, we know how to put individual parts into a whole. The ability to read is very indicative of this. To read a word, you need to put the letters together, and you need to create a phrase from the words. Manipulations with numbers are also carried out.
The parietal lobe helps to link individual movements into a complete action. When this function is disrupted, apraxia is observed. Patients cannot perform basic actions, for example, they are not able to get dressed. This happens with Alzheimer's disease. A person simply forgets how to make the necessary movements.
The dominant area helps you feel your body, distinguish between the right and left sides, and relate parts and the whole. This regulation is involved in spatial orientation.
The non-dominant side (in right-handed people it is the right side) combines information that comes from the occipital lobes and allows you to perceive the world around you in three-dimensional mode. If the non-dominant parietal lobe is disrupted, visual agnosia may occur, in which a person is unable to recognize objects, landscapes, or even faces.
The parietal lobes are involved in the perception of pain, cold, and heat. Their functioning also ensures orientation in space.
Prognosis for damage to the temporal lobe.
The prognosis of UDP is favorable in most cases if it is possible to avoid the dangers of general trauma and those specific to UDP (bleeding from large arteries, dislocations of the brain stem) in the acute period. Disability in the residual period of TBI can be caused by recorded defects of higher cortical functions - sensory aphasia, alexia, agraphia, acalculia; paresis of the limbs - with damage to the internal capsule to the depth of the internal capsule; hemianopic defects, usually partial; epileptic syndromes. Timely and systematic rehabilitation measures and rational anticonvulsant therapy are important.