Migraine
Pain in a certain part of the head, accompanied by a feeling of nausea, intolerance to light, and sharp sounds, is called a migraine. The disease affects every seventh adult, 3 times more often than others - women under 35 years of age. It can manifest itself even in children and adolescents, is hereditary in nature and is associated with functional disorders in the areas of the brain responsible for processing information about human sensations.
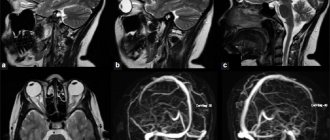
The intricate pathogenesis of migraine is not completely clear. The most recognized are vascular, neurogenic and biochemical theories of the origin of migraine. When the blood vessels in the brain narrow and their tone decreases in the area of the carotid artery, they become over-expanded. The vascular theory explains throbbing pain as a response of the vascular walls to the “beats” of the blood flow.
The neurogenic theory is based on the assertion that the cause of migraine is a failure of the regulatory function of the hypothalamus. The biochemical theory names the cause as a decrease in serotonin levels and disruption of cell membranes. Obviously, a migraine attack occurs with various disorders of brain activity. Migraine on EEG is manifested by cortical overexcitability, deviations in the amplitude and frequency of brain biorhythms.
A migraine attack occurs in two phases. A day before the attack, excessive irritability appears, a drop in mood, and occasionally euphoria. The second phase is characterized by pain - throbbing, concentrated in the frontal or temporal part of the head. Numerous accompanying symptoms occur: photophobia, acoustic phobia, nausea, general weakness. Migraines vary in severity and frequency: mild, moderate or severe. Attacks last 4 hours, sometimes up to 3 days. With organic changes in brain tissue, attacks are characterized by persistence, constancy, and an increase in the intensity of neurological manifestations. Persistent changes in the EEG during migraine confirm gross cerebral changes.
Mental disorders in brain tumors
Brain tumors account for about 6% of organic diseases of the central nervous system. Found in 0.1–5% of patients in psychiatric hospitals. Slightly more common in men. About half of primary tumors are gliomas. In addition, in children, medulloblastomas, astrocytomas, and plexuspapillomas are more often found, and in the elderly, meningiomas, glioblastomas, pituitary adenomas, and acoustic neuromas are more often found. Mental disorders are detected in 25–100% of patients with brain tumors. Sometimes these disorders are the first and for a long time the only symptom complex, especially if the tumor is characterized by slow growth; mental disorders in brain tumors are very diverse. It happens that with tumors of the same localization, different mental disorders develop, and with tumors of different localizations. There are transient and persistent mental disorders, as well as acute postoperative psychoses.
| | Often, symptoms of various mental disorders, such as schizophrenia, also appear with brain tumors. That is why comprehensive diagnostics is necessary to make a diagnosis. |
1. Transient mental disorders
1. Epileptic seizures. Astrocytomas and oligodendrogliomas of frontotemporal localization cause seizures in 90% of patients. Supratentorial slow-growing tumors are accompanied by seizures in more than 40% of cases. Seizures occur much less frequently (4%) with subtentorial tumors. In the structure of seizures, mental, motor and other disorders are not uncommon, which may indicate the topic of the tumor.
2. Hallucinations are observed in the structure of the aura or as part of a partial seizure. Olfactory deceptions are especially often observed with damage to the right temporal region. Usually combined with other disorders, including hallucinations of a different modality. Somewhat later, gustatory deceptions join the olfactory ones. Musical and rhythmic hallucinations are usually characteristic of patients with tumors of the right temporal region; imaginary sounds are heard on the left. Rhythmic auditory deceptions are, for example, the noise of the surf, a running motor, pouring water, the sounds of a bird chirping, repeated calls, etc. With tumors on the left, verbal deceptions of various contents are observed; more often they are combined with anxiety, transient aphasia, memory and thinking disorders. Optical illusions are less common than those mentioned. With tumors on the right, these are elementary hallucinations: dots, flashes of light, sparks, ripples, etc. Photopsia can be accompanied by musical deceptions. With tumors on the left, complex visions are observed - objects, people (often moving); there may be visions “inside the head... eyes”, visions “in the thoughts”. Tactile deceptions are rare and occur with tumors of the right hemisphere. Such deceptions also occur with sleep paralysis. Imaginary sensations related to the sexual sphere are frequent.
3. Affective disorders. With tumors of the right hemisphere, attacks with various disturbances are observed, but with the affects of melancholy and horror in the foreground. Attacks with positive affects also occur. With tumors on the left, anxiety and rage may predominate during an attack.
4. The phenomena of depersonalization and derealization. Characteristic for tumors of the right temporo-parietal-occipital region. At the same time, metamorphopsia and disturbances in the perception of time may occur, and very peculiar phenomena occur. For example, the patient feels that “time is going down.” Relatively rare symptoms such as echonesia, palinopsia (“visual perseveration”, when some visual image is exactly repeated several times in a row) or ignoring the space on the left are also observed.
5. Speech phenomena. Presented with attacks of speech loss. They are especially often observed in tumors of the left hemisphere. These may be attacks of motor aphasia, when instead of verbalizing the patient “moos” or utters other inarticulate sounds; the disorder may indicate a tumor of the left frontal lobe. With tumors in the left temporal region, attacks of sensory aphasia occur, i.e., misunderstanding of speech, the patient hears some kind of incomprehensible noise instead of the speech of others. He may react to the sound of speech and say several incoherent phrases. With a tumor of the temporo-parieto-occipital region on the left, the patient may suddenly lose the ability to select the right words - this is an attack of amnestic aphasia.
6. Disorders of thinking and memory occur with tumors of the left temporo-parietal-occipital region; thinking disturbances are represented by attacks of blockage of thinking (sperrung) and an influx of thoughts (mentism). Mnestic attacks occur both in the form of a “memory lapse” for various information, and in the form of a violent influx of memories of something from the past. There are also attacks during which there is an acute need to remember something, but the patient does not know what exactly.
7. Impaired consciousness and epileptiform states, in particular paroxysms of impaired clarity of consciousness: “fainting,” episodes of obnibulation, somnolence. They probably occur more often with subtentorial tumors. These are also episodes of reduplication (states “with two-track experiences” - Dobrokhotova, 1999). The patient freezes in one position and does not make contact. Without disconnecting from reality, in a few seconds he seems to relive certain situations of his past. Usually these are real, sometimes forgotten situations that seem to last for days and even weeks, compressed into such a small period of time. At the same time, there is a doubling of self-perception: the patient feels what he was like a long time ago and how he realizes his Self now. In such states, only the right side of real space can be realized. Sometimes ecmnestic attacks occur when, completely disconnected from reality, the patient feels himself somewhere in the distant past, living it again. It is possible that patients can sometimes be “transported” to a virtual situation (“memory hallucination” - M.B. Krol, 1936). Such episodes are characteristic of tumors of the right hemisphere. With tumors in the depths of the right hemisphere, near the 3rd ventricle, in the sellar-chiasmatic region, oneiric episodes may occur, often with partial congenital amnesia. Tumors of the left frontotemporal region reveal themselves as absence seizures, psychomotor seizures, and twilight states of consciousness. In terms of brain tumors, postictal confusion should also be a concern.
2. Persistent mental disorders
Productive disorders may be more common in tumors of the temporal and chiasmal-sellar regions, while deficient disorders occur in the frontal, especially convexity, regions of the brain.
1. Sleep and dream disorders. There may be changes in the sleep-wake cycle, increased frequency, decreased frequency of dreams, and nightmares. The feeling of sleep is lost, the boundary between dreams and reality is erased.
2. Memory impairment. In severe cases, Korsakov's syndrome develops, including retrograde amnesia. The disorder is usually combined with paresis and loss of sensitivity on the left, less often with left-sided spatial agnosia. A decrease in symbolic memory is observed with a tumor in the left hemisphere.
3. Affective disorders. Hypothymic states, melancholy depression, and bipolar mood disorders occur in right-hemisphere tumors. With tumors on the left, anxious depression and loss of emotions (combined with lack of spontaneity) are possible. Euphoria as part of the pseudoparalytic syndrome and mori-like states often occurs with frontobasal tumors; At the same time, disturbances of smell, vision (up to blindness unconscious to patients), and hemiparesis can be detected. Euphoria in the structure of Korsakov's syndrome is observed with tumors in the region of the 3rd ventricle. Significant emotional depression, anosognosia and left-sided spatial agnosia develop with tumors of the posterior parts of the right hemisphere and in the region of the 3rd ventricle. At the same time, there may be left-sided hemiparesis with hypoesthesia and hemianopia on the left; the gaze is directed to the right. Similar violations occur after operations to remove tumors of the specified localization.
4. Long-term disturbances of consciousness. Usually these are states of stunned consciousness of varying degrees. May occur in patients with rapidly growing tumors, as well as brain tumors in elderly patients.
3. Acute postoperative psychoses
They appear on the 2nd–3rd day after surgery and can last for several weeks. One of the causes of psychosis is cerebral edema. After removal of tumors of the frontotemporal region on the left, as well as neuritis of the 8th cranial nerve, hallucinatory-delusional psychoses are observed. After intervention in the posterior parts of the right hemisphere, near the 3rd ventricle, in the chiasmatic-sellar region, oneiric states, Korsakoff syndrome with euphoria and confabulations may occur. A state of akinetic mutism with congealing has been described in tumors of the 3rd ventricle (epidermoid cyst). Psychoses with severe euphoria, motor restlessness, disinhibition and foolishness, as well as euphoria and dyspraxia, when one hand did the opposite of the other, have been described. Age-related features of mental disorders in brain tumors are described. Thus, children with “dysontogenetic” tumors (for example, with craniopharyngioma) under the age of 5–10 years may have symptoms of progeria (these are children of the “little old men” type). As they grow older, stunted growth, sexual development, a tendency to be overweight, weakness, fatigue, and thirst become more and more noticeable. In grades 6–7, they compare academically with their peers, and then begin to lag behind them. In adulthood, they are characterized by lethargy, conservatism, and decreased creativity.
In older people, brain tumors are often not detected during life. In psychiatric hospitals, such patients are often considered as vascular patients, especially since every seventh of them has apoplectiform disorders. Focal paroxysmal phenomena are relatively rare; often after a single paroxysm, paresis and paralysis develop. Metastatic tumors of the frontal and frontotemporal region on the left predominate, causing dementia similar to Pick's and Alzheimer's diseases.
In all cases where patients experience paroxysmal headaches, congestion in the fundus, paroxysmal disorders, increasing psychoorganic decline and progressive neurological symptoms, a thorough examination is necessary in order to eliminate doubts about the volumetric process. Tumor failure still occurs on average in almost half of patients, especially the elderly.
Back to contents
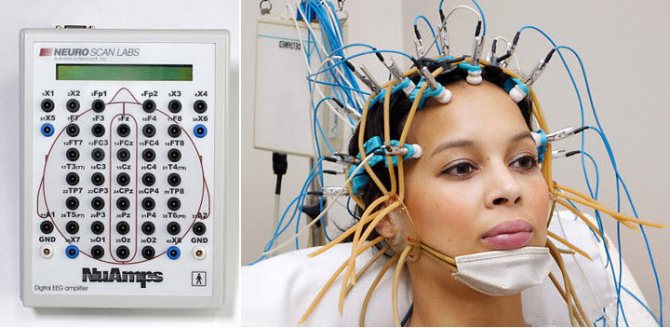
What is this procedure
After an MRI, which will show whether there are any organic brain abnormalities (for example, tumors), it is necessary to undergo an EEG (electroencephalogram). This is a modern examination method that allows you to assess the condition of neurons in the cerebral cortex. Each of the many neurons has bioelectrical activity and generates an electrical impulse transmitted along its processes to other cells. These impulses can be detected by special devices and the functionality of nerve cells can be analyzed.

The sensors of the EEG device detect the electrical waves of the brain, and an electroencephalogram is plotted on the monitor. Based on the curves obtained on the screen, the neurophysiologist can analyze the state of the brain and make a conclusion. The method is safe, non-invasive (non-invasive - without going inside).
The scan allows you to assess the usefulness of the functioning of individual areas of the brain. The doctor pays special attention to changes in brain biorhythms in the EEG during migraine. The EEG clearly records the impulses of the brain, which makes it possible to track the rhythm and consistency of all neurons in certain parts of it. The data received from the sensors is processed by a special computer program, displaying several graphs on the monitor.
The age of the patient, the period of activity (sleep, wakefulness), and the condition of the person being examined are taken into account. The rhythms reflect a person’s mood, medication intake, anxiety, etc. For more complex studies, various tests are used (flashes of light, sharp sounds, mental stress) in which biorhythms are recorded.
Indications for EEG
A painless and absolutely safe examination can be performed for adult patients and children. Using an EEG of the brain, the doctor can write a referral if various abnormalities are detected:
- various types of sleep disorders (sleepwalking, insomnia);
- skull injuries;
- vascular pathologies of the brain;
- psychical deviations;
- tumor-like formations;
- uncontrollable panic attacks;
- frequent unexplained fainting;
- epileptic seizures.
The EEG procedure is necessary for:
- stroke;
- endocrine system failures;
- examination of children with cerebral palsy. autism;
- VSD;
- encephalitis;
- headaches;
- meningitis;
- mental retardation;
The appointment is conducted by doctors:
Golitsyna Oksana Sergeevna
Neurologist, epileptologist, highest category
Eroshina Ekaterina Sergeevna
Neurologist, epileptologist, cephalologist, acupuncturist, candidate of medical sciences, highest category
Zaitsev Alexey Valerievich
Neurologist, ultrasound diagnostics doctor, highest category
Irishina Yulia Anatolevna
Neurologist, parkinsonologist, candidate of medical sciences, highest category
Kolyada Alexander Alexandrovich
Neurologist, epileptologist, candidate of medical sciences, highest category
Krivova Tamara Anatolyevna
Neurologist, acupuncturist, functional diagnostics doctor, first category
Ponedelko Tatyana Sergeevna
Neurologist, vertebrologist, acupuncturist, first category
Ten Maya Viktorovna
Neurologist, functional diagnostics doctor
Kholyavin Andrey Ivanovich
Neurosurgeon, Doctor of Medical Sciences, highest category
Tsinzerling Natalya Vsevolodovna
Neurologist, Candidate of Medical Sciences
Contraindications
There are no serious contraindications for performing an electroencephalogram. You should refrain from the procedure or postpone it if there are:

unhealed surgical sutures;- focal dermatitis;
- unhealed wounds;
- various skin inflammations or lesions.
Close medical supervision is required during EEG for persons with neurological abnormalities and involuntary movements of the limbs.
Electroencephalogram rhythms
The main type of oscillation in the encephalogram is the alpha rhythm
. In adults, its maximum frequency is present in the parietal and occipital regions of the cortex. And the minimum frequency is recorded in the temporal and frontal (8-14 Hz). The amplitude is up to 100 µV. Zonal differences decrease significantly with age. When the eyes open, the amplitude of the rhythm decreases; when the eyelids close, it is restored or increased. Instability of frequency, rhythm, paroxysms and arches signal pathologies (traumas, strokes, tumors). Alpha rhythm disruptions in children are a sign of developmental delay and psychopathology.
Beta rhythm
in the anterior, temporal zones of the GM, with a frequency of 14-40 Hz, depends on the functional activity of sensorimotor neurons. Deviations from the normal amplitude (asymmetry, paroxysms) indicate diseases.
Theta rhythm (4-8 Hz) –
weakly expressed in adults (in the frontal areas), more characteristic of the EEG of children, as a sign of the developing cerebral cortex. In adults, an increase in rhythm rather signals pathology.
Delta rhythm (1-4 Hz)
should not be present in an awake patient in adults. Registered during drug intoxication or coma. Its presence is a sign of deep sleep or pathology. With the help of EEG, it is possible to exclude or confirm brain pathologies, clarify the diagnosis and decide on therapeutic therapy for central nervous system pathologies.
In an adult patient, the predominance of alpha and beta rhythms (during wakefulness) is considered normal. Their electrical activity in both hemispheres should be the same; abnormal bursts mean pathology.
EEG is the most informative and unique of all methods for assessing the functionality of the brain. It allows you to identify complex pathologies developing in brain tissue. After an EEG for migraine, the conclusion is handed to the patient on paper or electronically. It can be shown to another neurology specialist. The conclusion states:
- type of waves, their activity and characteristics;
- description of indicators, their interpretation;
- compliance with the expected diagnosis.
Types of EEG and their differences
There are 5 modifications of the method.
- The classic method is electroencephalography - a non-invasive diagnosis that is based on measuring the electrical potentials of the brain and the total activity of cerebral structures. This is the most accurate way to study the condition of nerve tissue.
On the other hand, he is very sensitive. An awkward micro-movement is enough to blur the results.
At the same time, the results are affected by stress factors and the patient’s tension. And decoding is very difficult when the doctor is not experienced enough. There is a high risk of error.
- If classical EEG examines the electrical activity of the brain, rheoencephalography (abbreviated REG) focuses on the state of blood vessels. The essence of the technique is the effect on cerebral structures of a low-power current.
Based on the response, the doctor draws conclusions about the condition of the vascular walls, their conductivity and other characteristics. This is a very specific examination method.
- Echoencephalography (EchoEG) is used to assess the anatomical state of the brain. The technique is based on the reflective ability of the tissues of cerebral structures and the density of the substance.
Using echoEG, you can diagnose tumors and other space-occupying formations, and displacement of brain tissue. Which is very important in the early stages, because later treatment becomes unlikely.
- Pneumoencephalography (PEG) is extremely specific. The technique is based on filling the drainage system of the brain with air. It is injected in small quantities through a puncture in the lumbar region.
The technique allows you to measure pressure in the conduction system, assess the likelihood of ventricular dislocation and intracranial hypertension. These are indirect signs of several possible pathologies.
- Finally, magnetoencephalography (MEG), a visual method for assessing the electrical activity of the brain. Using special sensors, the desired indicator is recorded, after which, in visual form, the doctor receives a full-format picture of the distribution of impulses.
This is very convenient, since both foci of increased activity and shifts relative to the norm are visible. The method is used both in medicine and in theoretical scientific research.
As can be judged from the descriptions, none of the methods practically overlaps with the other. They face completely different goals and objectives.
Therefore, these methods can be prescribed in a system determined by a doctor.
How to prepare for an encephalogram
The accuracy of the examination data will be ensured by the correct preparation of the patient for the EEG and his responsible behavior during the procedure. Preparatory stage rules:
- 2-3 days before the EEG, you need to stop taking certain medications (anticonvulsants, tranquilizers) to avoid distortion of the indicators. Tell your doctor what medications you regularly take.
- During the day you cannot drink carbonated drinks (Coca-Cola), tea, all kinds of energy drinks, and alcohol. Avoid stimulating coffee and chocolate.
- Do not smoke 3-5 hours before the EEG.
- You should wash your hair without using conditioners, foams, or masks.
- You need to eat (light meals), when the stomach is empty, the blood sugar level increases.
- Immediately before the procedure:
- remove all jewelry (earrings, hair clips, piercings);
- loosen restrictive clothing parts (tight belts, neck scarves);
- take a comfortable position, close your eyes;
- try not to make unnecessary movements, not to be nervous, not to react to light flashes or noises of the device.
How is an EEG performed?

A cap with attached sensors filled with electrically conductive gel is placed on the patient’s head. They are connected by wires to an encephalograph, which builds graphs on the monitor in accordance with the obtained indicators.
The examination is carried out while the patient is awake (the person being examined must close his eyes with his eyelids and relax), less often - while sleeping. The procedure lasts about an hour, sometimes all night under the supervision of a doctor.
If the patient needs an encephalogram during the sleep phase, he must remain awake for a day and a half in order to fall asleep at the time of testing. Before the procedure, the doctor will give you a sedative to take, which will put you to sleep during the examination.
The brain waves detected by the sensors are amplified and displayed as a graph on the monitor. Subsequently, the graphs are printed on paper. Deciphering the received graphs will take several days. Experts, having analyzed the frequency and amplitude of the waves, make a conclusion, as evidenced by the electroencephalogram.
Examination technique
Sound waves are formed during the deformation of the diagnostic plate, the main purpose of which is to receive and reflect sound waves. Head tissues react differently to ultrasound. The dermis and subcutaneous fatty tissue form one type of signal, and tumors and cysts form another, and therefore are distinguishable against the background of the overall picture.
The brain encephalogram records waves reflected from intracranial structures and environments with excellent sound resistance. Bone and brain tissue differ in density. The method was introduced into practice by the Swedish neurologist Lars Leksell back in the 50s of the 20th century. The device generates a pulse and allows you to register the received echo signal. Data is recorded and reproduced.
ECHO-EG (echoencephalography) can be one- and two-dimensional, which is reflected in the presentation of the final result:
- a graph depicting several lines that correspond to the pulsation of various internal structures;
- in the form of a two-dimensional picture.
To make an encephalogram of the brain, no preliminary examination or tests are needed. This technique has no contraindications, therefore it is allowed for infants and pregnant women. The only obstacles are open wounds and fresh scars on the head after injuries and surgical interventions. Magnetic resonance imaging is recommended for patients with these limitations.
The examination is carried out in a lying or sitting position. When working with an infant, parents hold him. The only inconvenient point is the requirement to lie still, and the application of a conductor gel can also cause discomfort in children. Sensors are attached to two sides of the head, starting from the forehead to the occipital region. A constant signal is formed by the midline structures. This pulse is called M-echo.
There are several encephalogram modes:
- Transmission - involves installing two sensors at the same level on both sides of the head. One of them will send the signal, and the other will receive. After data processing, the midline of the head is compared with anatomical indicators. In case of pathologies (bruises, cysts or hematomas), the line deviates from the norm.
- Emission - involves connecting one sensor that sends waves directly to the area under study.
- A two-dimensional study involves placing sensors around the entire perimeter of the head. A flat image is displayed on the screen, which is important for determining skull asymmetry and post-traumatic deformation.
Classical electroencephalography of the brain is inferior to modern and accurate methods - computer and magnetic resonance imaging - in detecting small pathological foci.
The differences in signal decoding are that in the emission mode, one sensor sends and receives a signal, and in the transmission mode, the encephalogram of the head includes several echo signals:
- from soft tissues and bones directly below the source;
- from the intracerebral substance and structures between the hemispheres;
- from the inner layers of the skull and the meninges covering it on the opposite side.
Conducting an EEG for children

During the examination, a small child will need the mother's presence nearby to calm the baby. A child under one year old should be held in her arms by the mother during an EEG. The procedure is performed for children during sleep. While awake, the examination is carried out on balanced, calm children from 1 to 3 years old.
For babies and older children, parents should present a trip to the EEG office as an interesting and responsible adventure. Explain that you will need to put an “astronaut helmet” on your head and sit quietly and calmly.
Come up with other options that are acceptable to your child. Before the examination, you need to wash the child’s hair, feed him, and take a toy with him as a distraction.