Internal hydrocephalus (or hydrocephalus) of the brain (HHM) is a pathology that is characterized by the appearance of an excess amount of cerebrospinal fluid (also called cerebrospinal fluid), which is not removed anywhere and causes increased intracranial pressure (ICP) and thinning of the walls of the cerebral ventricles and their breakup. The disease is very dangerous, accompanied by neurological disorders and serious complications.
This disease can occur as a result of neoplasms, injuries or other pathologies, or perhaps as an independent disease. Internal hydrocephalus of the brain is diagnosed in adults less often than in children, especially in the first months of their life.
On a note! This serious illness occurs more often in boys than in girls.
A little about liquor and its functionality
In the human skull there are soft tissues, which are nothing more than his brain. A fluid (CSF) circulates between the bone and the meninges, which fills not only the internal ventricles, but also all existing depressions (grooves) on the surface of the main organ of the central nervous system.
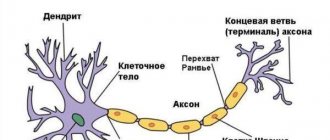
How is cerebrospinal fluid formed? This occurs as a result of a process such as the filtration of plasma (that is, the liquid part of the blood) through the walls of capillaries with the subsequent release of organic and inorganic substances into it. The composition of the cerebrospinal fluid circulating in the subarachnoid space and ventricles of the brain includes minerals, proteins and a very small number of cells such as lymphocytes and leukocytes. That is, in terms of the chemical composition, cerebrospinal fluid is very similar to the composition of blood.
What is the main function of cerebrospinal fluid? First of all, it is to protect the brain and the vessels located at its base from all kinds of mechanical influences (for example, shocks or jolts). Also, cerebrospinal fluid helps create a beneficial environment, which is so necessary for the normal functioning of the human central nervous system; maintains ICP at a certain level; participates in metabolic processes and nutrition of brain cells; and also acts as a protective barrier against bacteria, that is, it helps improve immunity.
Treatment of hydrocephalus of the brain in adults
The most effective treatment for hydrocephalus is shunt surgery. Although, with a compensated course of the disease, you can limit yourself to drug therapy for some time. Drugs used for “dropsy of the brain” are mainly aimed at reducing intracranial pressure by removing “excess” fluid from the body. It is also important to improve microcirculation and metabolism of brain cells.
Conservative therapy is carried out under the supervision of a doctor either in a hospital or on an outpatient basis. Since decompensation of the disease can occur suddenly and be complicated by cerebral edema.
Hydrocephalus treatment includes the following groups of drugs:
- diuretics: loop (Lasix, furosemide, hypochlorothiazide, torsemide, diacarb, acetazolamide), osmotic (mannitol) and potassium-sparing (veroshpiron, spironolactone). When using the first two groups, it is necessary to take potassium supplements (asparkam, panangin) in parallel. These drugs are ineffective in the normotensive form of the disease;
- vascular drugs (cavinton, vinpocetine, nicotinic acid);
- neuroprotectors (Ceraxon, Pharmaxon, Gliatilin, Gleacer);
- metabolic agents (actovegin, cortexin, cerebrolysin, cerebrolysate);
- anticonvulsants (carbamazepine, lamotrigine, valprocom) are used for the development of convulsive syndrome.
Drugs are prescribed and discontinued only by the attending physician, taking into account the individual characteristics of the patient.
Surgery, namely shunt surgery, is the main method of treating hydrocephalus. If the disease is caused by a mass formation in the brain (cyst, tumor, aneurysm), then, if possible, it is removed.
In case of acutely developing hydrocephalus in emergency situations, a lumbar puncture with the removal of no more than 50 ml of cerebrospinal fluid can alleviate the condition, but only in cases of absence of “plus” tissue in the brain. The method of external ventricular drainage is also used, when a catheter is inserted directly into the ventricles of the brain through a burr hole in the skull. The disadvantage of this method is the high risk of developing infectious complications.
In other cases, ventriculoperitoneal, ventriculoatrial or lumboperitoneal shunting is used. When cerebrospinal fluid from the ventricles is drained through a catheter located under the skin into the abdominal cavity, into the atrium, or from the spinal canal into the abdominal cavity, respectively.
Often with this method of treatment a number of complications arise:
- infections;
- violation of shunt patency;
- subdural hematomas and hygromas;
- hemorrhages;
- epileptic seizures;
- rapid outflow of cerebrospinal fluid, which can lead to herniation of stem structures.
In recent years, an endoscopic method has been developed, which consists of forming pathways for the outflow of cerebrospinal fluid from the third ventricle into the cisterns of the brain. The advantage of such surgical intervention is less trauma, restoration of the physiological dynamics of cerebrospinal fluid, and a reduced risk of complications.
How does the outflow of cerebrospinal fluid occur?
In an adult, the amount of cerebrospinal fluid, which is a crystal-clear substance, varies between 140-270 ml. It is updated 4 times during the day. This process largely depends on factors such as water balance, nutrition and physical stress that a person experiences.
The space in which the liquor circulates is closed. The outflow of fluid occurs by filtration not only through the arachnoid membrane into the venous system, but also through the nerve sheath into the lymph. In a normal state, the volume of outflow corresponds to the amount of inflow, that is, a balance is maintained. In the case of a neoplasm in the brain, hemorrhage, injury to the spine or skull, the outflow process is disrupted, resulting in an increase in the volume of cerebrospinal fluid (that is, internal hydrocephalus is observed), an increase in intracranial pressure, disruption of the functioning of the central nervous system and, as a result, the occurrence of various pathologies.
Syringomyelia and the army
Syringomyelia is a serious disease in which a cavity appears in the spinal cord due to enlargement of the central canal. This pathology is considered chronic and has a slow progression.
Nervous tissue cells (glia) appear in the spinal cord, which disrupt the transmission of nerve impulses to the brain. The disease can be present throughout life and in rare cases cause a bulbar disorder (changes in heart rate, breathing) leading to death.
This disease can progress quickly due to intense physical exertion, therefore, when passing a medical commission, the conscript may be assigned a category of limited fitness or given a complete exemption (category “B”, “D”).
Classification of dropsy
Patients may experience:
- External HGM, which is characterized by the fact that cerebrospinal fluid is not absorbed into the bloodstream. And this is the big problem.
- Internal GGM. It differs in that there is an accumulation of a certain amount of cerebrospinal fluid in the subarachnoid space and the ventricles of the brain.
- Mixed GGM. It is characterized by the fact that cerebrospinal fluid accumulates not only in the cisterns and ventricles of the brain (that is, inside), but also under its membranes (that is, outside).
- Internal replacement hydrocephalus of the brain, which results in atrophy of brain tissue and its replacement with cerebrospinal fluid. It is very serious. Most often, such “metamorphoses” occur due to age-related factors. But internal replacement hydrocephalus of the brain in an adult can also be caused by other reasons (for example, alcoholism or infections).
- Closed (or occlusive) hydrocephalus. The disease occurs due to the fact that the outflow of cerebrospinal fluid is impossible due to the presence of a neoplasm, with the growth of which the situation only gets worse. Very severe form.
- Internal open hydrocephalus of the brain (or communicating HGM). There is hypersecretion of cerebrospinal fluid and a failure in the process of its absorption.
- Spicy. The disease progresses rapidly and symptoms expand.
- Subacute. The increase in symptoms occurs gradually (over 1-1.5 months).
- Chronic. The development of clearly noticeable manifestations of the disease is observed no earlier than 6-12 months after the onset of the pathology.
- Vicarious hydrocephalus. With this disease, the ventricles become enlarged. Moreover, no changes in the structure of the organ itself in terms of anatomy are observed.
- Internal asymmetric hydrocephalus of the brain. In this case, either an enlargement of one ventricle or all of them may be observed.
- Hypertensive. In this case, there is a significant increase in intracranial pressure.
- Normotensive. The size of the ventricles changes, but the pressure does not differ from normal.
On a note! External and internal hydrocephalus of the brain can be either congenital (that is, appear at the stage of intrauterine development of the fetus) or acquired (that is, appear during a person’s life).
Depending on the reasons for the impossibility of outflow of cerebrospinal fluid, the following forms of the disease are distinguished:
The form of development of the disease can be:
On a note! Moderate internal hydrocephalus of the brain is very poorly recognized, and is generally diagnosed completely randomly. Pronounced symptoms are observed when significant structural brain disorders occur, as well as a failure in the blood circulation of the main organ of the central nervous system. We shouldn't forget about this. And visit a medical facility more often in order to prevent serious pathologies and treat them. Remember: the development of moderate internal hydrocephalus of the brain in adults can lead to serious complications.
Depending on changes in the size of the ventricles, the disease is divided into:
Hydrocephalus can be:
Important! Regardless of what type of dropsy is diagnosed, remember: this is a very dangerous neurological disease that requires observation by a specialist and, if the condition worsens, immediate surgical intervention.
Main types and causes of pathology development
Hydrocephalus is divided into congenital, which develops in the prenatal period, and acquired. The first most often makes itself felt immediately after birth; extremely rarely the symptoms linger for several years.
Considering the mechanism of occurrence of pathology, its following forms are distinguished:
- internal hydrocephalus (closed, occlusive, non-communicating) - occurs as a consequence of a disruption in the normal flow of cerebrospinal fluid due to a block of the pathways. In this case, the liquor accumulates in the ventricles of the brain;
- external hydrocephalus (open, aresorptive, communicating) - develops against the background of dysfunction of the pachyonic granulations, venous sinuses, lymphatic vessels, that is, due to impaired absorption of cerebrospinal fluid into the systemic circulation. Cerebrospinal fluid accumulates mainly under the membranes of the brain;
- hypersecretory hydrocephalus - is a “subtype” of external hydrocephalus and occurs due to increased production of cerebrospinal fluid in the choroid plexuses of the ventricles;
- mixed hydrocephalus, or “ex vacuo” hydrocephalus, consists of the replacement of “empty” space with cerebrospinal fluid, which occurs against the background of primary or secondary atrophy of brain tissue and, accordingly, a decrease in its volume. This condition is otherwise called external replacement hydrocephalus. The amount of cerebrospinal fluid in this case increases mainly on the convexital surface of the brain, to a lesser extent due to the expansion of the ventricles.
According to the course, hydrocephalus is classified into:
- acute - such hydrocephalus develops within 2 - 3 days;
- subacute - this type of hydrocephalus develops within a month (no less than 21 days);
- chronic - hydrocephalus, which occurs within a period of 3 weeks to 6 months, and sometimes longer.
Hydrocephalus may be accompanied by increased intracranial pressure - this is the hypertensive type; with normal cerebrospinal fluid pressure, normotensive hydrocephalus develops. In cases where the pressure of the cerebrospinal fluid decreases, they speak of hypotensive hydrocephalus.
According to the degree of disturbances that occur with hydrocephalus, it is divided into:
- compensated - in this case, hydrocephalus often does not manifest itself with any symptoms and is detected during examinations carried out in connection with other diseases of the nervous system;
- decompensated - when the symptoms of “dropsy of the brain” come to the fore, while hydrocephalus often leads to irreversible changes in brain tissue.
Closed hydrocephalus has the following causes of development:
- volumetric formation of the brain (tumor, cyst, vessel aneurysm, arteriovenous malformation, abscess), especially if localized in the posterior cranial fossa;
- ventriculitis (in other words, ependymitis) - inflammation of the ventricles of the brain, leading to swelling of the adjacent brain tissue and, accordingly, to the blocking of the holes through which cerebrospinal fluid circulates;
- hemorrhage localized in the ventricles or subarachnoid space - the resulting blood clots often block the cerebrospinal fluid pathways;
- granulomatous process - expressed in the formation of granulomas (nodules) in the ventricular system of the brain, which block the outlet openings;
- craniovertebral anomalies, which include Arnold-Chiari syndrome. A condition that develops due to disproportionate growth of the brain and cranium. Due to the large size of the brain, it protrudes through the cerebellar tonsils into the foramen magnum. As a result, the outflow of cerebrospinal fluid from the skull into the spinal canal is disrupted.
External hydrocephalus can occur due to:
- development of inflammatory processes in the membranes and tissues of the brain (meningitis, encephalitis, arachnoiditis), which interfere with the normal absorption of cerebrospinal fluid (bacterial, viral, fungal infection);
- subarachnoid or parenchymal hemorrhage;
- traumatic brain injury, especially complicated by the formation of traumatic hematomas;
- tumor process in the membranes of the brain (meningeal carcinomatosis);
- an increase in oncotic pressure in the cerebrospinal fluid, as a result of an increase in protein content, or any other change in the composition of the cerebrospinal fluid, leading to an increase in its viscosity;
- defects and anomalies in the development of the nervous system, which are accompanied by the accumulation of cerebrospinal fluid at the site of the nervous tissue defect;
- hyperproduction of cerebrospinal fluid due to papilloma of the choroidal plexus in the ventricles;
- impaired absorption of cerebrospinal fluid into the venous system due to thrombosis of the sinuses of the dura mater of the brain.
Mixed hydrocephalus, which is most often normotensive, develops due to cerebral atrophy against the background of degenerative brain diseases: Alzheimer's disease, Parkinson's disease, cerebellar ataxia, chronic encephalopathies (alcoholic, atherosclerotic, hypertension, etc.).
The most common types of hydrocephalus in adults are hypertensive occlusive and external replacement hydrocephalus (ex vacuo).
Inside the skull is the brain, blood and cerebrospinal fluid. Under normal conditions, a balance is maintained between the volumes of these three components. Any violation of it leads to the development of complex pathologies. Thus, an increase in the volume of cerebrospinal fluid compresses blood vessels and the brain, leading to impaired blood supply, tissue death, and increased blood pressure. Hemorrhage, in turn, leads to disruption of the outflow of cerebrospinal fluid and its accumulation.
The mechanism for the development of hydrocephalus is precisely the excess of cerebrospinal fluid. It is formed in the four cerebral ventricles, with up to 70% produced in the glands, the remainder by the exudation of the liquid component of the blood through the walls of blood vessels. The flow of cerebrospinal fluid is carried out from the ventricles into the subarachnoid cavity, which expands and forms the cerebral cisterns.
From these cavities it reaches the outer surface of the brain, and is later absorbed through the villi located in the area of the venous sinuses. Normally, the amount of liquor produced (on average in an adult is 150 ml) corresponds to that absorbed.
However, in any of these areas, obstructions or disturbances can occur, leading to excess cerebrospinal fluid - hydrocephalus.
The disease is caused by the following reasons:
- Inflammation of the brain and its membranes. This group includes meningitis, encephalitis, and tuberculosis.
- Impaired blood supply. Hydrocephalus develops as a result of bleeding in the brain, the appearance of a blood clot, or rupture of a bulging vessel (aneurysm).
- Neoplasms. Regardless of their nature - benign or malignant, they lead to blockage of cerebrospinal fluid circulation.
- Intoxication. The effects of alcohol, drugs, heavy metal salts.
- Injuries. This group includes not only traumatic brain injuries that led to brain swelling and destruction of blood vessels, but also consequences after operations.
- Diseases of the central nervous system.
- Infectious diseases. This is rubella, syphilis.
- Age-related changes. Replacement hydrocephalus is associated precisely with how the body and its tissues change with age.
What is the danger of hydrocephalus for adult patients?
Internal hydrocephalus of the brain in adults can be expressed in the development of:
Important! If treatment for the disease is not started in a timely manner, disability may occur.
Treatment
Mild external hydrocephalus is amenable to drug therapy. If the disease progresses and the prognosis is poor, surgery is prescribed.
Conservative methods
Drug treatment must be comprehensive. If minimal external hydrocephalus of the brain appears due to infection or head injury, then drugs are prescribed to eliminate the inflammatory process: anti-inflammatory, antibacterial agents, desensitizing therapy.
To reduce the inflammatory process, medications of the NSAID group (ketoprofen, ketorolac, ibuprofen) are prescribed. They have a complex effect: they reduce temperature, inflammation, and pain. They disrupt the synthesis of prostaglandins by inhibiting COX activity.
For neuroinfections, antibacterial therapy is carried out. Broad-spectrum drugs are prescribed: tetracyclines, cephalosporins.
Additionally, desensitizing therapy is carried out using antihistamines (diphenhydramine, suprastin, tavegil) to reduce sensitivity to any antigens.
The basis of conservative treatment is the use of diuretics. They help reduce ICP and intraocular pressure; promote the elimination of sodium and water as quickly as possible (diacarb, brinaldix, lasix). The therapeutic effect is short, the drugs reduce potassium and magnesium in the blood, so they should be used in emergency cases.
Surgical methods
Surgery is the basic method of treatment. It is indicated if the pathology appeared from birth, with a progressive form of HC, as well as in cases where the prognosis for psychological and motor activity without surgical intervention is unfavorable.
For many years, bypass surgery was practiced to treat HC. The purpose of the operation is to create an outflow of CSF. Various shunt systems are used (special drainage tubes with a valve), which ensure the outflow of excess CSF into the subarachnoid cisterns, the abdominal cavity, or outside.
The operation is quite complex; the slightest errors in the technique lead to serious consequences:
- infection, traumatization;
- mechanical damage to the shunt;
- valve obstruction with cessation of cerebrospinal fluid flow;
- overdrainage - excessive CSF flow, as a result of which the patient’s blood pressure decreases and dizziness occurs;
- hypodrainage - insufficient, slow cerebrospinal fluid flow; surgery in this case is not effective enough.
Patients who have undergone this operation must be constantly monitored by a doctor; they become shunt dependent forever. It is necessary to follow the recommendations of the rehabilitation period.
As practice shows, bypass surgery causes complications in 50% of cases. In this case, parts of the shunt or the entire mechanism must be replaced.
A more modern and priority method of treatment for HC is endoscopic intervention. There are several types of such operations:
- septostomy (to open the transparent septum of the brain);
- aqueductoplasty (stenting of the cerebral aqueduct);
- endoscopic bypass surgery, etc.
Endoscopic surgery allows the surgeon to shape the path for the outflow of CSF, while monitoring the progress of the intervention using a miniature video camera, which is inserted into the skull through a small hole.
If unexpressed HC is caused by developmental abnormalities, then surgical intervention is aimed at eliminating the root cause of the pathology. According to indications, the following may be prescribed:
- Removing clots and blood from the hematoma cavity.
- Removal of tumor formations.
- Removal of a brain abscess.
- Dissection of adhesions for decompression of the optic nerves, etc.
The danger of hydrocephalus for children
The development of internal hydrocephalus of the brain in children largely depends on the age of the baby. What the disease can lead to:
That is, the impact on mental development of the consequences of such a pathology as internal hydrocephalus of the brain in children is obvious: it is difficult for them to concentrate and adapt normally in society.
On a note! Statistics say that 30% of children who have suffered from the disease have impaired speech function; and 20% of patients find it very difficult to express positive emotions such as happiness and joy.
But don't despair. Remember: if operational measures are carried out on time, then you can avoid mental retardation in your child. And one more thing: most children who suffer from hydrocephalus grow up to be quite happy and friendly people who communicate with others with great pleasure.
Symptoms
The disease is popularly called dropsy of the brain. This is due to the external signs that the pathology exhibits.
In adults
In adults, the bone tissue of the head is already formed, so there may be no external symptoms. The disease may not manifest itself for a long time.
Headaches that periodically bother every person can be minor. But HC will still manifest itself, since the accumulation of CSF leads to disruption of the blood supply to the brain and the development of symptoms characteristic of this condition.
Excessive accumulation of CSF leads to increased ICP, but in chronic external replacement hydrocephalus it can be normal.
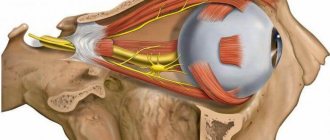
The patient is bothered by an intense throbbing headache that is not relieved by medications. It appears mainly after sleep and may subside during the day. Against this background, nausea may develop, including vomiting. The hallmark of headaches associated with HC is ocular discomfort. The patient feels increased pressure on the eyeballs. With a slight tilt of the body, this feeling intensifies.
Compression of brain structures provokes a number of disorders:
| Type of disorder | Description |
| Mental | Emotional lability, neurasthenia, mood swings. When symptoms worsen, unreasonable aggressive behavior is possible. |
| Vestibular | There is a lack of coordination, unsteadiness in standing and sitting positions, loss of orientation in space. There is no control of body movements, limbs, handwriting is disrupted. The patient is bothered by systemic vertigo, in which he experiences rotation of the body to a state of rest or movement of surrounding objects. Symptoms intensify when turning the body, head, and eyes, which forces the patient to avoid these movements or perform them at a slow pace. |
| Vegetative | During exacerbations, the complexion changes. Due to the lack of control of movements, a feeling of fear appears, panic develops, tachycardia, lack of oxygen, and discomfort in the heart. |
| Visual | Violation of visual control: blurred vision, color perception disorder, narrowing of the field of vision (lack of lateral), the appearance of dark spots, decreased pupil response to a light stimulus, twitching of the eyeballs, downward gaze shift. |
| Muscular | Paresis, paralysis, increased muscle tone, increased tendon reflexes, decreased sensitivity. |
In children
Children have external signs of HC, because the process of formation of the bone tissue of the head is incomplete, moderate external hydrocephalus is manifested by an increase in the size of the cranial cavity. Visually, the brain region significantly predominates over the facial region.
In infants, newborns, and young children, the head size exceeds the norm. On palpation, arterial pulsation of the large fontanelle is absent, and its bulging is observed. The cranial sutures may come apart. Its covering bones are thinning. The saphenous veins of the head swell. The eye sockets become deformed, the optic nerves swell, and upward movement of the eyeballs is limited. In advanced cases, strabismus develops.
Children whose pathology is diagnosed at an early age are lagging behind in motor and physical development. They later begin to hold their head up, roll over, crawl, sit, walk, and talk. Forced to tilt your head back. Physical activity is low, so there is a tendency to obesity. Behavior: the child is irritated, sleeps poorly, cries often, refuses to breastfeed, sleeps often and for a long time.
Unlike HC in adults, in children the disease mostly manifests itself not as neurasthenic disorders, but as a lack of intelligence. But it may be insignificant. School-age children may have excellent mechanical memory, verbosity, and musical abilities. An exception is HC due to meningoencephalitis.
Initial symptoms that may indicate increased ICP are:
- anxiety;
- disturbance of sleep and wakefulness;
- headache.
Older children more often have an acquired form of the pathology, in which they constantly suffer from headaches, blurred vision, nausea, and vomiting. Epilepsy attacks, loss of consciousness, convulsions, hallucinations, and delirium may be present.
Causes of illness in adult patients
Internal hydrocephalus of the brain in adults can occur due to the following reasons:
Normal pressure hydrocephalus
This type of hydrocephalus, which was described by S. Hakim and R. D. Adams in 1965, is often classified as a separate nosological entity. Normal pressure hydrocephalus manifests itself as a gradual increase in the size of the ventricles of the brain with constant cerebrospinal fluid pressure and the development of walking disorders, dementia and disorders of the pelvic organs in the form of urinary incontinence. This symptom complex is also called the Hakim-Adams triad.
Normal pressure hydrocephalus of the brain in adults does not have treatment, which results in complete recovery. Surgery (bypass surgery) for this disease brings a short-term effect. In 55 - 70% of cases, it is impossible to influence the progression of the pathology. This hydrocephalus occurs in the elderly (0.42% of cases among people over 60 years of age), in patients suffering from dementia (0.4 - 0.62%) and in 15 - 16% of patients who have a walking disorder.
The causes and mechanisms of formation of this disease are not completely clear. It is believed that the stage of production and absorption of cerebrospinal fluid is disrupted. Normal pressure hydrocephalus is communicating, external.
Disruption of the outflow of cerebrospinal fluid into the venous sinuses of the dura mater through Pachionian granulations occurs due to fibrous changes in the membranes of a post-infectious (meningitis, arachnoiditis), post-traumatic or non-traumatic (subarachnoid hemorrhage, carcinomatosis, vasculitis) nature. Although almost 60% of patients did not have a history of any of the pathologies listed above.
Hydrocephalus, which persists for many years, leads to degenerative and ischemic irreversible damage to the white and gray matter of the brain. The fact that walking impairment and dementia are often “frontal” in nature is associated with a significant increase in the anterior horns of the lateral ventricles, as a result of which the periventricular tissue of the brain becomes thinner and the corpus callosum and pathways are damaged.
Normal pressure hydrocephalus symptoms gradually increase over several months and sometimes years. The following symptoms are characteristic of this pathology:
- frontal type walking disorder. This is the very first and most striking manifestation of normotensive hydrocephalus, in some cases it is the only one. At first, the patient's gait becomes slow, uncertain, and unsteady. It is difficult for patients to start moving in an upright position (gait apraxia) and to stand. Despite the fact that in a lying or sitting position, they easily imitate walking, cycling, etc. The patient moves slowly, shuffles his feet, and spreads them wide. At times the patient seems to forget how to walk, then he stops and stomps around in one place. Purposeful movements in the hands are occasionally impaired. A phenomenon such as “trunk apraxia” also occurs: balance is disturbed, even to the point of falls. In the later stages of the disease, the patient is not even able to sit independently. During a neurological examination, attention is drawn to muscle hypertonicity in the legs and rigidity. It is possible that pyramidal insufficiency may occur, manifested by spasticity, revitalization of tendon reflexes and the appearance of pathological foot signs (Babinsky reflex, etc.);
- disorders of higher mental functions in the form of frontal-type dementia, which grows rapidly over 4 to 12 months against the background of existing walking disorders. It is manifested by apathy, decreased criticism of one’s condition, lack of spontaneity, euphoric mood, and disorientation. In rare cases, hallucinations, delusions, depression and seizures occur;
- difficulty urinating in the early stages of the disease. First, complaints appear about frequent urination during the day and, especially, at night. Urgency then develops, followed by urinary incontinence. Due to cognitive impairment, patients cease to be critically aware of this pathology. The so-called frontal type of pelvic disorders is formed.
Normotensive hydrocephalus is not characterized by symptoms such as headache, nausea and vomiting, congestion in the area of the optic nerve head, etc. That is, the symptoms that accompany the hypertensive form of “dropsy of the brain” do not occur.
Causes of hydrocephalus in children
Hydrocephalus in children can be congenital or acquired. The first form is quite common. Its development occurs while the fetus is inside the womb and may be due to the following reasons:
The second form can develop as a result of:
Diagnostics
If you suspect HC, you should contact a neurologist. To clarify/refute the pathology, as well as to determine the characteristics of its course, the following may be prescribed:
- Transillumination of the skull. Helps assess the degree of thinning of the brain substance and detect local accumulation of CSF.
- Survey radiography. Helps to identify secondary changes in the bone tissue of the cranium (thinning, suture dehiscence, etc.).
- Echoencephalography. Determines the degree of increased pressure in the skull.
- MRI and CT are the most informative diagnostic methods. Layer-by-layer scanning gives a complete picture of the disease: the nature of the GC, the exact location, etc.
MR signs of mildly expressed HC are clearly visible even at the initial stage of the disease. The study helps verify minimal atrophic changes in brain cells. The MR picture of moderate external hydrocephalus reveals an increase in subarachroidal spaces, the presence of subdural hematomas, an increase in the density of the cerebrospinal fluid due to the accumulation of cells, etc.
To identify the etiological factor of the disease, the following may be prescribed:
- lumbar puncture;
- MRI of cerebral vessels;
- PCR diagnostics.
If the clinical picture is severe, you may additionally need to consult an endocrinologist, ophthalmologist, or psychotherapist.
Symptoms of the disease in adults
What symptoms may indicate the presence of internal hydrocephalus of the brain in adults:
Important! The feeling of heaviness and headache intensify while a person sleeps and in the morning (immediately after waking up). Moreover, in a horizontal position the symptom only intensifies.
Important! Very often, patients do not pay attention to all the symptoms listed above, mistaking them for signs of senility. This is a big mistake, since if the disease is not treated, its consequences can lead to dementia or encephalopathy. Remember this and promptly seek qualified help from medical institutions.
Increasing ICP and military service
In fact, there is a significant difference between these concepts.
For example, this is how hypertension syndrome most often occurs in children. The bones of the skull and the ventricular system of the brain experience fluid pressure, and the cerebrospinal fluid is practically incompressible. Therefore, an enlargement of the skull and ventricles of the brain occurs.
As for the sudden rise in ICP, this can be illustrated by a picture of a growing space-occupying formation, when the cerebrospinal fluid pressure increases very quickly. This hypertension syndrome in adults is manifested by the following symptoms:
- bursting headaches that bother you at night and in the morning, but disappear in the afternoon and evening, when the outflow of “fluid from the head” is normalized due to the vertical position of the body;
- vomiting that occurs without previous nausea, the so-called “cerebral vomiting”.
In this case, these signs of hypertension syndrome arise due to irritation by high cerebrospinal fluid pressure of the rhomboid fossa, or the bottom of the 4th ventricle, where the nuclei of the caudal group of cranial nerves are located. Vomiting does not bring relief and is not associated with food intake. It is also called “fountain vomiting” because of its suddenness; - congestive optic discs. If this process continues for several weeks or months, then ophthalmoscopy can reveal a uniform, “stagnant” fundus of the eye.
All this should alert not only a neurologist, but also any doctor. An examination, such as an MRI of the brain, should be urgently carried out. Most often, treatment of acute hypertension syndrome, due to its secondary nature, is carried out by removing the corresponding tumor, restoring the patency of the cerebrospinal fluid tract.
How does hypertension syndrome occur in newborns? What should parents pay attention to?
Hypertension syndrome in infants manifests itself differently than in adults. The fact is that the relatively soft and pliable bones of the skull and the presence of fontanelles make it possible for quite a long time to compensate for the increase in intracranial pressure, which can be caused by various diseases, as well as perinatal trauma.
The most common signs of chronic increased ICP in children include the following symptoms:
- bulging fontanel;
- increase in head circumference;
- the appearance of a subcutaneous venous network on the surface of the skull;
- restlessness and crying, especially worse at night when the baby is lying down;
- sleep disorders;
- frequent regurgitation and vomiting;
- refusal to feed and loss of appetite;
- as a result, there is a lack of weight gain.
Also a symptom of long-term hydrocephalus is the “setting sun symptom”, or Graefe’s symptom. The white sclera becomes visible when looking down. Normally, the eyelid covers the sclera, but with hydrocephalus, the eyeball stands anteriorly, due to increased pressure, and the eyelid does not cover the sclera.
In conclusion, one more issue needs to be considered - the attitude of the military medical commission to intracranial hypertension. Are hypertension and the army compatible? If there is confirmation of ventricular enlargement according to MRI data, but there are no complaints, the outpatient card does not contain a history of the disease (missing school, hospitalization due to deterioration of health, consultations with neurosurgeons, progression of vision loss), then category “B” will be assigned. , that is, “fit for military service with minor restrictions.” In other words, a conscript who has mild hypertension, and even complaints, but not documented, will serve.
Also, the conscript must be ready to challenge the commission’s decision right up to the court, presenting strong evidence of unfitness for military service in peacetime.
Hydrocephalus of the brain in an adult has symptoms that are not as pronounced as hydrocephalus in children. In a child, “dropsy of the brain,” accompanied by an increase in cerebrospinal fluid pressure, causes not only headaches, crying, anxiety, and impaired consciousness, but also in infancy leads to a change in the configuration of the cranium, a rapid increase in head circumference, and bulging of the fontanelle.
The average person often does not pay attention to such manifestations of pathology as headaches and sleep disturbances. All this is attributed to overwork at work and constant stress. And the already developed hydrocephalus clinic, which includes the following symptoms, forces you to seek help:
- headache of a bursting nature, occurring most often in the morning immediately after sleep. The rate of increase in pain depends on the rate of development of hydrocephalus;
- nausea and vomiting at the height of headache. Vomiting with hydrocephalus rarely brings relief and does not depend on food intake. Sometimes this is the first symptom of hydrocephalus, especially with tumors located in the posterior cranial fossa;
- sleep disturbance (drowsiness during the day and insomnia at night);
- persistent hiccups;
- impairment of consciousness of varying degrees (from stupor to coma);
- visual disturbances, most often manifested by double vision. This symptom develops as a consequence of compression of the abducens nerves. Paroxysmal disorders also occur in the form of limitation of visual fields, which arise due to a decrease in venous outflow from the eye and damage to the optic nerve;
- a congestive optic disc is formed, which is detected during examination of the fundus by an ophthalmologist. This symptom is characteristic only of chronic and subacute hydrocephalus, since during the development of acute “dropsy of the brain” it is often delayed;
- pyramidal insufficiency, manifested by symmetrical pathological foot signs (Babinsky's symptom, Rossolimo, etc.);
- Cushing's triad, which includes increased blood pressure against the background of bradycardia and bradypnea (decreased breathing).
It must be remembered that the severity and speed of onset of symptoms in hydrocephalus depends on the type of disease, namely the rate of increase in intracranial pressure. With an acute increase in cerebrospinal fluid pressure, the symptoms will be pronounced, but some may be “late” (for example, changes in the fundus).
Symptoms of hydrocephalus in children
In children, the skull bones are not yet completely strong, so the manifestations of the disease are more pronounced than in adults suffering from the same disease. Symptoms of dropsy in newborns are as follows:
With age, the pathology progresses, and the symptoms only get worse:
Symptoms by age
Typical symptoms of hydrocephalic syndrome are visual disturbances.
The symptoms are caused by intracranial hypertension and hydrocephalus.
General signs of HS:
- nausea;
- vomit;
- headache;
- personality changes or epileptic seizures.
However, in children and adults, the symptoms of hydrocephalic syndrome differ significantly.
In infants
In a child under one year old with hydrocephalic syndrome, decreased muscle tone, weak tremor, and a positive Graefe sign (“setting sun”) are noted.
There is an increased increase in head circumference (about 1-2 cm monthly). The baby's head looks disproportionately large.
Sometimes a baby with hydrocephalic syndrome exhibits swelling of the optic disc.
Symptoms of HS in adolescents and children;
- visual impairment (strabismus, loss of visual field), decreased visual acuity to the point of blindness;
- fine motor skills disorders;
- disturbances in concentration;
- personality changes, behavioral problems (anxiety, impatience, categoricalness), hypersensitivity to noise;
- respiratory, speech and swallowing disorders;
- endocrinological (metabolic) disorders;
- early puberty before 8 years of age (very rare).
In adults
Symptoms of HGS in adult patients:
- cephalalgia, vomiting, dizziness in the morning;
- visual impairment (diplopia - double vision);
- convulsive conditions;
- severe fatigue;
- restless behavior.
Symptoms of hydrocephalus with normal intracranial pressure:
- moderate gait disturbances;
- dementia and/or personality changes (forgetfulness, increased irritability);
- hydrocephalic cry;
- urinary and fecal incontinence.
Diagnostic methods
HGM can cause disruption in all systems of the human brain. To cope with the disease, it is necessary to determine what was the root cause of the ailment. To do this, the neurologist, after carefully listening to the patient (that is, identifying the history of the disease) and examining him, takes the following measures:
Next, the specialist must have information about DCH. Its level can be determined using the following instrumental studies:
Methods for diagnosing the disease
It is more difficult to determine moderate hydrocephalus, which does not have pronounced indicators. Often, specialists detect the disease by chance, but it disrupts the internal circulation of the brain, resulting in disorders of the nervous system.
In adults, moderate hydrocephalus of the brain can be a separate disease or occur in the form of complications after tumors, traumatic brain injuries, stroke, infections and meningitis. The disease often develops with hypertension, atherosclerosis, and damage to the musculoskeletal system.
During hydrocephalus, the size of the brain is reduced, and this area is filled with cerebrospinal fluid, which is not absorbed by the venous system. It is classified as atrophic brain disease.
The pathology has two stages: acute and chronic. In the acute stage, the main signs of the disease appear, and in the second stage, the symptoms of hydrocephalic syndrome are revealed.
Diagnosis of hydrocephalus consists not only in detecting its signs, but also in trying to establish what disease of the nervous system it was caused by. This usually does not cause difficulties, given modern examination methods.
The tactics of further treatment of the patient depend on the correct diagnosis. The methods used in examining adults and children differ somewhat, because in children a clear clinical picture comes to the fore: changes in the shape of the skull, depression of consciousness, convulsive seizures, and impaired psychomotor development.
Therefore, an MRI or CT scan of the brain may not be needed; neurosonography will be enough. Since neuroimaging diagnostic methods require lying still, this will require the use of sedatives or light anesthesia, which is not always possible due to the child’s health condition.
So, diagnostic methods for hydrocephalus are divided into instrumental and non-instrumental.
Non-instrumental diagnostics includes the following methods:
- interviewing the patient, asking for anamnesis of life and illness. If the patient is in clear consciousness, the neurologist clarifies his complaints, previous diseases and injuries to the nervous system, how quickly the symptoms developed, and what the first of them was. In case of depression or impairment of consciousness, this information is obtained from the patient’s immediate environment;
- neurological examination - allows you to identify focal changes that arise as a result of neoplasms in the brain, leading to a block of the cerebrospinal fluid pathways; signs of increased intracranial pressure (pain when pressing on the eyeballs, trigeminal points, changes in visual fields, etc.); pyramidal insufficiency and gait disturbance, changes in the shape of the skull (in older people this may occur during osteoporotic processes);
- neuropsychological testing reveals signs of dementia, affective disorders (depression, etc.);
- examination by an ophthalmologist - examination of the fundus often reveals congestive changes in the area of the optic nerve head.
It is impossible to confirm the diagnosis based on complaints and physical examination, so they resort to the use of instrumental methods:
- radiography of the skull (craniography) – in adults this examination method is not very informative. With its help, the size of the skull, the condition of the sutures and bones are determined. With a long-term increase in intracranial pressure, signs of porosity and destruction of the sella turcica may be detected;
- echoencephaloscopy is an ultrasound method that allows you to identify signs of hydrocephalus and indirectly confirm the presence of a space-occupying lesion in the brain by the displacement of its midline structures;
- lumbar (spinal) puncture followed by biochemical and cytological analysis of the cerebrospinal fluid - is performed only in the absence of a space-occupying formation in the cranial cavity. With hypertensive hydrocephalus, cerebrospinal fluid flows out under pressure and extraction of 35 - 50 ml of fluid leads to a significant improvement in the patient's condition. Subsequent analysis may reveal signs of hemorrhage, increased protein levels;
- CT or MRI of the brain - changes detected using these examination methods confirm not only the presence of hydrocephalus, but also “explain” the reason for its formation. That is, in addition to the expansion of the ventricles, an increase in the size of the grooves and subarachnoid space, the following is detected: a block of the cerebrospinal fluid pathways with a space-occupying formation, damage to the meninges and choroid plexuses in the ventricles, or signs of neurodegenerative diseases are visualized.
Only a qualified neurologist can establish the correct diagnosis. When the first symptoms of the disease appear, you should immediately contact a specialist, since rapidly increasing hydrocephalus can lead to dislocation of the brain stem structures and death.
Therapy
The method of treating internal hydrocephalus of the brain depends on the stage of development of the disease:
Diet
Diet for pathology is complementary and helps to stop the progression of pathology. The first step is to avoid foods that cause fluid accumulation in the body. Doctors strictly prohibit the use of:
- sweet products: cakes, chocolates, cookies;
- smoked meats and sausages;
- freshly baked flour products;
- fatty varieties of meat products;
- foods rich in calcium gluconate.
When you are sick, simple food that is easily digested and absorbed by the body is useful. The majority of your diet should include vegetarian food. Recommended:
- lemons;
- cucumbers;
- pumpkin;
- parsley;
- bee products;
- cabbage;
- celery;
- zucchini;
- watermelon;
- black currant;
- grape;
- black radish.
Only the attending physician should determine the diet after determining the exact cause of the disease. With a rapidly developing pathology, it is important to eat diuretic foods. The body must receive a sufficient amount of amino acids, proteins, carbohydrates, and vitamins. Experts highly recommend avoiding salt intake. Thanks to this, the water-salt balance will not be disturbed.
These products should not be included in the diet. Their use will have a negative impact on the patient’s health, and can also increase unpleasant symptoms and contribute to exacerbations.
Diagnosis
An experienced pediatric neurologist can easily identify a disease in a child based on visual signs - the appearance of the pupils, an enlarged skull.
Methods for diagnosing the disease in adults:
Magnetic resonance imaging is an informative study that allows you to accurately determine the shape and characteristics of the pathology;
Angiography is an x-ray of blood vessels using a contrast agent to evaluate disorders of the circulatory system of the brain;
Examination of cerebrospinal fluid taken as a result of puncture.
The data obtained from the study forms the basis of the treatment strategy prescribed by the doctor.