general description
Narcolepsy and cataplexy (G47.4) is a disease of unknown etiology, characterized by frequent, irresistible attacks of falling asleep (2-6 times during the day) and episodes of cataplexy (sudden loss of muscle tone, often with a fall, but with preservation of consciousness - several seconds, minutes ).
Narcolepsy occurs more often in adolescence or young adulthood.
Prevalence: 40 per 100 thousand people, men get sick more often. In 25% of cases there is a hereditary predisposition.
How to treat cataplexy
Therapy of a secondary disease comes down to eliminating the underlying pathology. The treatment method for primary affective adynamia depends on the severity of the clinical picture.
Medicines are prescribed if cataplexy threatens the patient’s health, significantly reduces his quality of life, or interferes with the performance of professional duties. Psychostimulants and tricyclic antidepressants from the subgroup of selective inhibitors, which slow down the reuptake of the hormone serotonin, help block the disease.
Drug treatment as an auxiliary measure is indicated for disorders that have developed as a result of traumatic events. In this case, it is mandatory to undergo a course of psychotherapy and autogenic training based on self-hypnosis, muscle relaxation and self-education.
If attacks last up to 10 seconds and do not lead to traumatic consequences, to neutralize the signs of Löwenfeld-Henneberg syndrome, it is enough to adjust the patient’s lifestyle in accordance with the principles of a healthy lifestyle.
To normalize night sleep, physiotherapy (phototherapy, encephalophonia, hydrotherapy) and folk remedies are used. The most effective are considered:
- lemon balm or fireweed tea;
- oil massage;
- lemon or vinegar-honey mixture;
- pumpkin and cabbage juices;
- honey diluted with a glass of carbonated mineral water or kefir;
- cocktail of sprouted wheat grains and hazelnuts;
- warmed milk with the addition of 2-3 cloves of grated garlic;
- warm aromatic baths with 4-5 drops of rose, chamomile or lavender oil;
- infusions of red hawthorn berries, lavender, alfalfa, hop cones, elderberry, motherwort and lettuce;
- decoctions of dill seeds, unpeeled oats, turnips, chamomile and primrose flowers;
- herbal decoction based on oregano, valerian root, dandelion leaves and mistletoe.
Clinical picture
Patients are concerned about frequent daytime falling asleep in unusual circumstances (while eating, talking, working). There is sleep disturbance at night and daytime sleepiness (80%). Periods of sudden weakness in the entire body or one part of the body (jaw or arm muscles) are triggered by strong emotions (laughter, rage, surprise) (75%). Episodes of cataplexy are accompanied by periodic falls (45%).
35% of patients experience dream-like visions before falling asleep, another 60% complain of the inability to move an arm/leg or say something when falling asleep or waking up.
During an objective examination, the patient’s clear consciousness is noted; paroxysmal daytime falling asleep, cataplexy, hypnagogic/hypnopompic hallucinations, and sleep paralysis can be recorded. During cataplexy, tendon reflexes fade, autonomic dysfunction occurs (changes in pupil size, sweating, bradycardia), consciousness is preserved.
Causes and symptoms of cataplexy
In 70% of cases, the disorder is part of a narcoleptic sympotocomplex - excessive sleepiness during daylight hours. The neurophysiological mechanism of the development of the disease is not fully understood. There are 2 theories of the appearance of primary pathology (it is also called Löwenfeld-Henneberg syndrome).
According to the first, affective adynamia is preceded by depletion or destruction of cells in the posterior and lateral parts of the hypothalamus that produce hypocretin (orexin). This neuropeptide is responsible for maintaining a state of wakefulness; its deficiency causes narcolepsy and related disorders. Proponents of the second version argue that the root cause of the disease is damage to brain receptors sensitive to this substance.
Be that as it may, the sick person’s body acquires a tendency to suddenly transition into a state physiologically reminiscent of the REM sleep phase. The transmission of nerve impulses is inhibited, large muscles relax, and the brain continues to function with the same intensity.
Lowenfeld-Henneberg syndrome is usually accompanied by such abnormalities as:
- hypersomnia (sleep disorders);
- diabetes;
- extreme obesity;
- endocrine-vegetative disorders;
- arterial hypotension;
- lymphocytosis (increased concentration of lymphocytes);
- eosinophilia (increased number of eosinophilic leukocytes);
- amymia (inhibition of facial expressions due to mental and neurological diseases).
External risk factors include:
- prolonged stay in a zone of natural disasters or military operations;
- alcohol or drug addiction;
- psychotraumatic events: getting into an accident, armed attack, street robbery, falling from a great height, etc.
As a rule, affective adynamia of the primary type makes itself felt in adolescence and disappears as one grows older. Secondary cataplexy occurs under the influence of pathologies such as:
- multiple sclerosis;
- traumatic brain injuries;
- congenital anomalies of the structure of the vascular system of the brain;
- metastases of breast, lung or thyroid cancer;
- infections that damage brain structures (encephalitis, viral meningitis);
- tumors of the brain in the hypothalamus region.
The disease of both types manifests itself paroxysmally - in the form of atonic muscle attacks, that is, complete relaxation of the muscles while maintaining consciousness, normal breathing, level of intelligence and the ability to understand what happened.
An attack can be triggered by various emotional experiences (surprise, fear, rage), including positive ones (laughter). Most often, patients experience the following signs of cataplexy :
- throwing back the head;
- drooping of the lower jaw;
- bending the legs at the knees;
- inability to maintain an upright position;
- bradycardia (irregular heart rhythm with slow pulse);
- pallor or redness of the skin around the face and neck;
- dilated pupils;
- increased sweating;
- slurred speech or temporary numbness;
- decreased reflexes of the mucous membranes;
- weakening of the grip of objects in the hands;
- blurred vision (defocus, double vision).
According to the severity and area of distribution of the disease, it is customary to distinguish 3 forms of cataplexy seizures:
- total (general, generalized) is characterized by the presence of all the above symptoms;
- partial (partial) covers the muscles of individual parts of the body (head, upper or lower extremities);
- Awakening cataplexy (sleepy stupor, post-hypnoplegia) includes an anxious state when falling asleep, up to auditory and visual hallucinations, a persistently negative (“nightmare”) emotional coloring of dreams, an inability to speak and control coordination after a sudden awakening.
Treatment of narcolepsy and cataplexy
Treatment is prescribed only after confirmation of the diagnosis by a medical specialist. "Meridil", "Indopan", "Sidnocarb", "Modafinil", tricyclic antidepressants ("Imipramine", "Clomipramine") are shown.
Essential drugs
There are contraindications. Specialist consultation is required.
- Meridil (psychostimulant). Dosage regimen: orally, in the first half of the day, 0.01-0.015 g per dose. Daily dose is 0.01-0.03 g. The course of treatment is from 2 weeks to 4 months.
- Sidnocarb (psychostimulant). Dosage regimen: prescribed orally, at a dose of 5 mg 1-2 times a day, in the first half of the day, before meals. Then the dose is gradually increased to 15-25-50 mg/day; maintenance dose - 5-10 mg/day.
- Clomipramine (tricyclic antidepressant). Dosage regimen: 25 mg orally 1-3 times a day.
Diagnosis of cataplexy
To make a diagnosis, you need to consult a neurologist. After collecting anamnesis, it is necessary to undergo a comprehensive examination:
- polysomnography (hardware sleep study);
- multiple sleep latency test (MSLT testing) to assess the biological need for daytime sleep - the procedure is carried out no later than 1-2 hours after the patient wakes up;
- electroencephalography (measurement of the total electrical activity of the brain);
- magnetic resonance and computed tomography of the brain;
- Epworth sleepiness scale questionnaire.
Differentiation with atypical epileptic seizures, hypokalemic paralysis, neurotic motor dysfunctions, drop attacks, paroxysmal myoplegia, vertebral artery syndromes, Pickwick syndrome, periodic hibernation and sleep apnea, acute intermittent porphyria and iatrogenic intoxication is required.
Recommendations for narcolepsy and cataplexy
Consultation with a neurologist and polysomnography are recommended.
| • | Leading specialists and institutions for the treatment of this disease in Russia: |
| Doctor of Medical Sciences, head of the department of the Russian State Medical University, professor, academician of the Russian Academy of Medical Sciences Evgeniy Ivanovich Gusev. | |
| • | Leading specialists and institutions for the treatment of this disease in the world: |
| G. AVANZINI, Italy. |
Treatment of cataplexy
The course of basic therapy will depend on the underlying factor, if any. The medicinal part of treatment in most cases is combined with the doctor’s general recommendations regarding nutrition, work and rest.
Medications that may be prescribed include:
- selective inhibitors;
- tricyclic antidepressants;
- psychostimulants;
- vitamin-mineral complex and restorative preparations.
Physiotherapeutic procedures may also be prescribed:
- phototherapy;
- hydrotherapy;
- encephalophonia.
In addition, you should pay attention to general recommendations that will help not only eliminate attacks, but also prevent them in the future:
- exclude physical and psycho-emotional shock;
- maintain a daily routine and rest schedule;
- eat properly and in a timely manner;
- exclude alcohol abuse and do not resort to drugs.
The same recommendations can be used as prevention. Patients with this diagnosis need to systematically undergo a medical examination and not work in conditions where increased attention is required.
If you think you have cataplexy
and symptoms characteristic of this disease, then a neurologist can help you.
Source
Did you like the article? Share with friends on social networks:
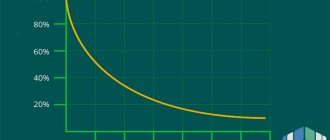
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
Causes
The REM sleep dissociation hypothesis proposes that cataplexy is a muscle paralysis that typically occurs during REM sleep intrusion into waking hours.
The exact cause of this invasion is unknown, but loss of neurons that produce hypocretin (also known as rudexin) is thought to be a major contributing factor to the invasion. Hypocretin is a neurotransmitter involved in promoting wakefulness during the sleep cycle.
Certain human leukocyte antigens, variations in T-cell receptors, or immune system responses to certain exposures to antigens have been found in people with cataplexy. It is believed that narcolepsy may be an autoimmune disorder, but more research is needed.
A study published in the Journal of Clinical Investigation in 2010 found that the loss of hypocretin is caused by an autoimmune response directed at autoantigens of tribbles homolog 2 (tribbles 2). This autoimmune response causes the formation of trib 2 antibodies that target and kill the hypocretin-producing neurons in the brain.
The frequency of cataplexy episodes ranges from less than once a year to several times a day. The average person with cataplexy has one or more episodes each week.
Symptoms
| Occurrence (how often a symptom occurs in a given disease) | |
| Daytime sleepiness | 100% |
| Other various forms of sleep disorders | 80% |
| General weakness (fatigue, tiredness, weakness of the body) | 80% |
| It is difficult to move or say something when falling asleep or waking up | 60% |
| Decreased sleepiness in the evening | 50% |
| Frequent stumbles and falls | 45% |
| Dream-like visions before falling asleep | 35% |
Classification
Cataplexy is classified depending on the severity of the pathological process and can be of the following types:
- total or general - in this case, there is a loss of muscle tone of the entire body, and the person cannot move at all;
- partial or partial - tone disappears in certain muscle groups: legs, arms, stomach, neck, and so on.
Depending on the cause of occurrence, the following types of this syndrome are distinguished:
- gelastic cataplexy - an attack occurs as a result of a strong emotional shock - both positive and negative;
- after waking up - in this case, an attack of cataplexy occurs immediately after sleep and rarely lasts longer than one minute.
Cataplexy status is distinguished separately - attacks follow each other.
Cataplexy attacks - causes, symptoms, danger, treatment
Cataplexy mainly occurs due to sleep disorders of various etiologies. Accompanied by short-term severe muscle weakening. The person falls but remains conscious. The pathological condition is associated with severe psychological shock. Often occurs in connection with narcolepsy.
What it is
Cataplexy is a disorder of muscle tone control. Mainly associated with strong, pleasant emotions. Happiness is one of the typical triggers. But they can also occur due to excitement, irritation, extreme surprise, or stress.
In most cases, the condition is associated with narcolepsy. Rarely appears against the background of pathologies: Prader-Willi syndrome, Wilson's disease and Niemann-Pick. These diseases are rare in medical practice.
A similar condition can occur with stroke, multiple sclerosis, head injury and encephalitis.
Why is it dangerous?
Uncontrolled muscle condition poses a danger to the person himself and others. If the victim cannot stay on his feet, there is a high probability of injury. Especially on the street, production and other work areas.
There is great danger when driving a car. If there is no control of the leg muscles, an emergency situation on the road may occur.
Who experiences
People who suffer from alcoholism and drug addiction are at risk of developing this pathology. In other cases, the disease appears very rarely. Sometimes this is encountered after an accident or a fall from a height.
Age and gender do not affect the pathological process.
Patients who are too emotional and have an unstable psyche are more likely to experience this disorder. It can be provoked by pleasant and negative feelings, especially strong fear.
When and who to contact
At the first suspicious sensation, you should consult a doctor. The disease manifests itself in varying degrees of complexity. Therefore, it is important to diagnose it in a timely manner.
Initially, you will need to consult a neurologist. Additionally, they are examined by an endocrinologist and a psychologist.
It is important not to confuse this condition with epileptic seizures or hyperkalemic paralysis.
Treatment methods
The mild and moderate stage, which is not accompanied by the risk of injury, usually does not require drug therapy. The patient is recommended to make lifestyle adjustments.
Simple rules for the health of the body will help with this:
- prevention of emotional and physical fatigue;
- rejection of bad habits;
- eating healthy, nutritious food and drinks;
- avoid the use of sedatives and hypnotics;
- limit the influence of irritating factors.
If it is not possible to do without drug therapy, the patient is prescribed the following medications:
- tricyclic antidepressants;
- psychostimulants;
- selective inhibitors;
- drugs to strengthen the body.
Additionally, you will need to undergo psychotherapy courses. They prescribe training for self-hypnosis and control of one’s own emotions. If sleep has returned to normal, then physiotherapy is used.
Nasal drops with hypcretin are at the development stage. Perhaps they will be an effective medicine in the future.
Prevention and recommendations
Narcolepsy and cataplexy are conditions that have similar symptoms but different etiologies. The patient must learn to control his own emotions, consciousness, and prevent severe shock. It is important to be able to react calmly to sudden situations.
The attacks are accompanied by a threat to the life and health of the patient. Pathology affects the usual rhythm of life and work activity. Significant restrictions appear. Sometimes you have to change jobs.
Therefore, if suspicious symptoms develop, you should consult a doctor to avoid complications. Consultation with a neurologist, somnologist, or psychologist will help get rid of the progression of the disease.
Source: https://zason.ru/katapleksiya/
What is cataplexy
This pathology is characterized by a sudden disappearance of muscle tone - from barely noticeable to short-term total atony. That is, a person cannot hold his body in a certain position. In medicine, it is customary to consider cataplexy as one of the symptoms of a neurological disease such as narcolepsy.
Excerpt characterizing cataplexy
“Well, what can we do? If you can’t do without it! What to do! So, this is how it should be,” he said to himself and, hastily undressed, went to bed, happy and excited, but without doubts and indecisions. “We must, strange as it may be, no matter how impossible this happiness is, we must do everything in order to be husband and wife with her,” he said to himself. Pierre, a few days before, had set Friday as the day of his departure for St. Petersburg. When he woke up on Thursday, Savelich came to him for orders about packing his things for the road. “How about St. Petersburg? What is St. Petersburg? Who's in St. Petersburg? – he asked involuntarily, albeit to himself. “Yes, something like that a long time ago, long ago, even before this happened, I was planning to go to St. Petersburg for some reason,” he remembered. - From what? I'll go, maybe. How kind and attentive he is, how he remembers everything! - he thought, looking at Savelich’s old face. “And what a pleasant smile!” - he thought. - Well, don’t you want to go free, Savelich? – asked Pierre. - Why do I need freedom, Your Excellency? We lived under the late count, the kingdom of heaven, and we see no resentment under you. - Well, what about the children? “And the children will live, your Excellency: you can live with such gentlemen.” - Well, what about my heirs? - said Pierre. “What if I get married... It could happen,” he added with an involuntary smile. “And I dare to report: a good deed, your Excellency.” “How easy he thinks it is,” thought Pierre. “He doesn’t know how scary it is, how dangerous it is.” Too early or too late... Scary! - How would you like to order? Would you like to go tomorrow? – Savelich asked. - No; I'll put it off a little. I'll tell you then. “Excuse me for the trouble,” said Pierre and, looking at Savelich’s smile, he thought: “How strange, however, that he does not know that now there is no Petersburg and that first of all it is necessary for this to be decided. However, he probably knows, but he’s only pretending. Talk to him? What does he think? - thought Pierre. “No, someday later.” At breakfast, Pierre told the princess that he had been to Princess Marya yesterday and found there - can you imagine who? - Natalie Rostov. The princess pretended that she did not see anything more extraordinary in this news than in the fact that Pierre had seen Anna Semyonovna. - Do you know her? – asked Pierre. “I saw the princess,” she answered. “I heard that they were marrying her to young Rostov.” This would be very good for the Rostovs; They say they are completely ruined. - No, do you know Rostov? “I only heard about this story then.” Very sorry. “No, she doesn’t understand or is pretending,” thought Pierre. “It’s better not to tell her either.” The princess also prepared provisions for Pierre's journey. “How kind they all are,” thought Pierre, “that now, when they probably couldn’t be more interested in this, they are doing all this. And everything for me; That’s what’s amazing.” On the same day, the police chief came to Pierre with a proposal to send a trustee to the Faceted Chamber to receive the things that were now being distributed to the owners. “This one too,” thought Pierre, looking into the police chief’s face, “what a nice, handsome officer and how kind!” Now he deals with such trifles. They also say that he is not honest and takes advantage of him. What nonsense! But why shouldn’t he use it? That's how he was raised. And everyone does it. And such a pleasant, kind face, and smiles, looking at me.” Pierre went to dinner with Princess Marya. Driving through the streets between the burned-out houses, he was amazed at the beauty of these ruins. The chimneys of houses and fallen walls, picturesquely reminiscent of the Rhine and the Colosseum, stretched, hiding each other, along the burnt blocks. The cab drivers and riders we met, the carpenters who cut the log houses, the traders and shopkeepers, all with cheerful, beaming faces, looked at Pierre and said as if: “Ah, here he is! Let's see what comes out of this." Upon entering the house of Princess Marya, Pierre was filled with doubt as to the justice of the fact that he was here yesterday, saw Natasha and spoke with her. “Maybe I made it up. Maybe I’ll walk in and not see anyone.” But before he had time to enter the room, in his entire being, after the instant deprivation of his freedom, he felt her presence. She was wearing the same black dress with soft folds and the same hairstyle as yesterday, but she was completely different. If she had been like this yesterday when he entered the room, he could not have failed to recognize her for a moment.
Recommendations
The patient needs to learn to control his consciousness, to predict situations that can cause emotional outbursts.
Attacks of cataplexy pose a threat to the life and health of the patient, significantly affect his quality of life, and do not allow him to fully perform his professional duties.
If the slightest symptoms appear, you should consult with specialists - a neurologist, somnologist, this will allow you to start treatment on time and avoid progression of the disease.
Literature
- Levin Ya. I.
Parasomnias: current state of the problem: [arch. June 12, 2020] // Epilepsy and paroxysmal conditions. - 2010. - T. 2, No. 2. - Lazareva A. A.
Brownie, the walking dead man and the soul that has left the body: interpretations of sleep paralysis in East Slavic culture: [Russian] / Khristoforova O. B., Antonov D. I. - V International Scientific Conference “Demonology as a Semiotic System”. - M., 2020. - May. — ISBN 978-5-7281-2044-5. - Brian A Sharpless.
A clinician's guide to recurrent isolated sleep paralysis : [English] : [arch. June 7, 2020] // Neuropsychiatric Disease and Treatment. — 2020. — Vol. 12 (July). — P. 1761–1767. — ISSN 1176-6328. - doi:10.2147/NDT.S100307. - PMID 27486325. - PMC 4958367. - Brian A. Sharpless, Karl Doghramji.
Sleep Paralysis: Historical, Psychological, and Medical Perspectives. - Oxford University Press, 2020. - 287 p. — ISBN 0199313806. — ISBN 9780199313808. - Esther Olunu.
Sleep Paralysis, a Medical Condition with a Diverse Cultural Interpretation : [English] : [arch. June 7, 2020] / Esther Olunu, Ruth Kimo, Esther Olufunmbi Onigbinde ... [et al.] // International Journal of Applied and Basic Medical Research. — 2020. — Vol. 8, no. 3. - P. 137–142. — ISSN 2229-516X. - doi:10.4103/ijabmr.IJABMR_19_18. - PMID 30123741. - PMC 6082011. - Dan Denis, Christopher C. French, Alice M. Gregory.
A systematic review of variables associated with sleep paralysis : [English] : [arch. June 7, 2020] // Sleep Medicine Reviews. — 2020. — Vol. 38 (April). — P. 141–157. — ISSN 1087-0792. - doi:10.1016/j.smrv.2017.05.005. - PMID 28735779.
additional literature
- Revonsuo A.
Psychology of consciousness. - 2012. - 338 p.
Links
Sleep disorders Parasomnias Catathrenia • Nightmare • Night terror • Sleep talking • Sexsomnia • Somnambulism • Sleep paralysis Sleep culture Alarm Clock • World Sleep Day • Inemuri • Lullaby • Sleep Mask • Lucid Dreaming • Dream Book • Bedroom • Snoring