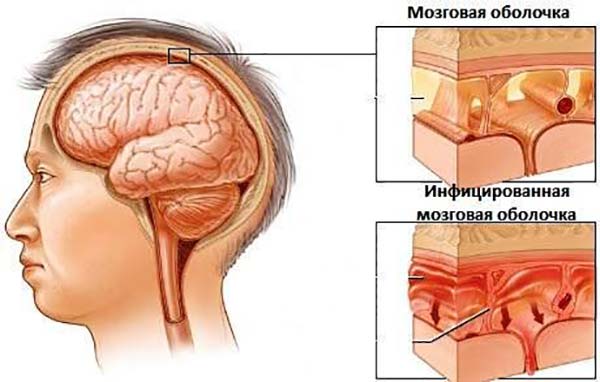
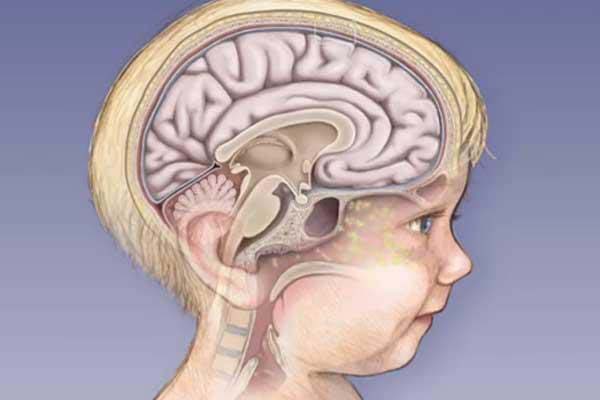
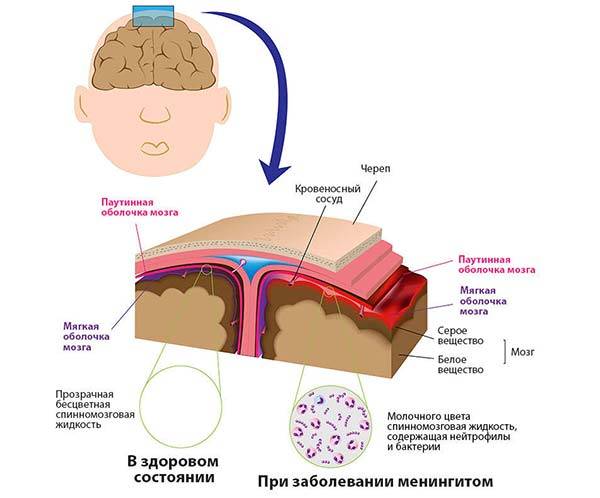
Meningitis is a very dangerous disease for humans that causes inflammation of the soft membrane of the brain.
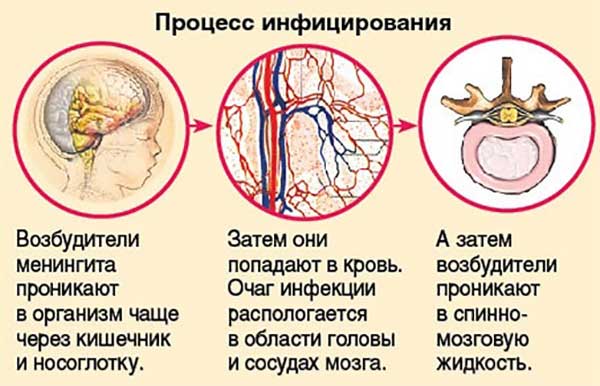
The disease is infectious in nature, that is, it is caused by bacteria and viruses, fungi and protozoa. Infection with meningitis leads to difficulty in the absorption and outflow of cerebrospinal fluid (cerebrospinal fluid). In this regard, intracranial pressure increases.
If you suspect meningitis, you should immediately call an ambulance. Treatment is carried out only in an inpatient setting at an infectious diseases hospital, since meningitis is a contagious disease.
Why does the temperature rise with meningitis?
Meningitis is an infectious and inflammatory disease that affects the soft membranes of the brain. The causative agents of inflammation are viruses, fungi and bacteria of several groups, and the disease itself is often severe, with dangerous consequences for the body.
Temperature during meningitis is a characteristic symptom among others, which you need to pay attention to and take timely measures to help the patient avoid complications. Is meningitis always accompanied by fever, what levels can the thermometer reach during and after the disease, how does the pathology proceed in adults and children - this will be discussed in the article.
Causes and signs of the disease
With meningitis, temperature, general clinical symptoms and the severity of the disease depend on several factors. This is the general state of the immune system, the age of the patient, as well as the pathogen that caused the development of the pathology. Therefore, it is worth talking about each type of disease - for what reasons it occurs, what signs are accompanied, what thermometer marks should be expected.
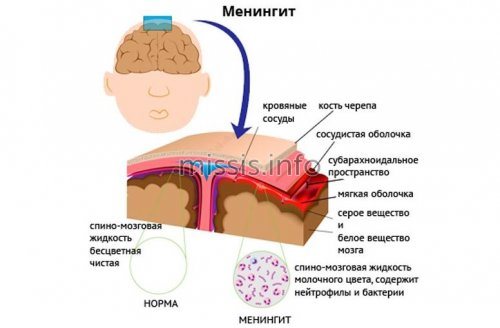
According to the nature of the inflammatory process, meningitis is divided into serous and purulent.
Serous meningitis
The serous variety most often affects children aged 2-7 years. It is characterized by a long prodromal period (the period of time between the incubation period of the disease and its peak) lasting 2-3 weeks. At this stage, general malaise appears, there is no appetite, the patient becomes lethargic and apathetic, and a low-grade fever of 37.1-38 degrees is noted.
After the pathology enters the acute stage, pronounced clinical manifestations begin - vomiting, severe headache, neck tension, constipation. The patient lies on his side or back with his head thrown back, legs bent at the knees and abdomen retracted.
The disease is caused by ECHO viruses, viruses of the Coxsackie family, polio and mumps. You can become infected from a sick person, by swimming in contaminated water, or after eating unwashed vegetables or fruits. Adults are rarely infected; more often the disease affects children of preschool and school age.
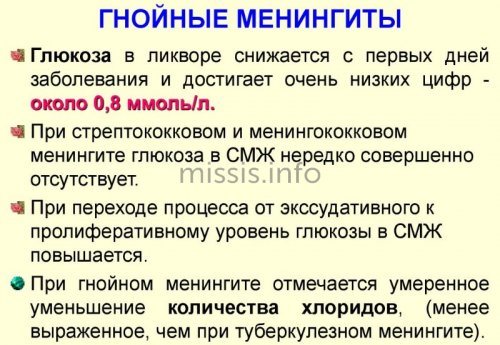
Purulent meningitis
This is an inflammation of the membranes of the brain of a purulent nature. The causative agents of the disease are Escherichia coli and Haemophilus influenzae, staphylococcus, pneumococcus, listeria, streptococci of groups B and D. The risk of getting sick increases after surgical interventions in the head and neck area, as a result of traumatic brain injuries. For pronounced signs of the disease to appear, there must be a focus of chronic infection in the body, from where pathogenic pathogens penetrate into the brain tissue.
The onset of the disease is characterized by chills, fever, and general deterioration of health. In severe cases, the patient experiences delirium, convulsions, and vomiting. Meningeal signs are pronounced - a fever of 39-40 degrees, a change in the rhythm of heart contractions, increased tone of the muscles of the back of the head.
Classification by pathogens
Meningitis is also divided depending on the type of pathogen:
- bacterial - most often the infection is caused by a meningococcal pathogen that penetrates through the circulatory or lymphatic system into the cells of the central nervous system. Meningitis can also be pneumococcal, tuberculous, etc. Manifests itself as toxic, allergic, septic reactions, resulting in damage to blood vessels, kidneys, adrenal glands, liver, brain, heart muscle;
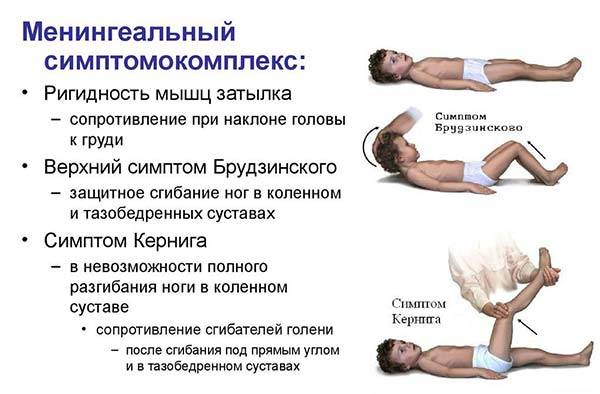
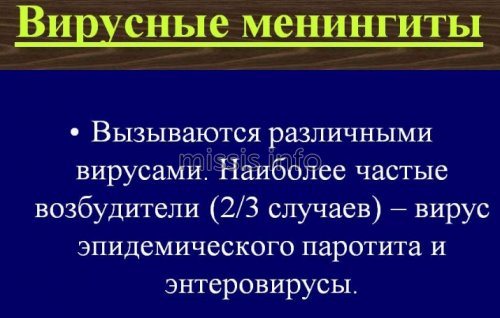
- viral – caused by RNA viruses such as ECHO, Coxsackie and enteroviruses. The disease can develop as a complication of mumps, rubella or other viral infections. It has an incubation period of 2-4 days, after which cough, runny nose, pain in the abdomen and head appear. Lethargy may give way to anxiety, and the thermometer rises sharply. Kernig's symptoms are observed (the patient's inability to fully straighten the leg at the knee joint, which was previously bent at a right angle in the hip and knee joints) and Brudzinski's symptoms (when bending the head, the patient's legs involuntarily bend and are pulled towards the stomach; when pressing on the pubis, the legs bend at the hip joint and in the knees; when pressure is applied to the cheek, the shoulders reflexively rise and the arms bend at the elbows);
- protozoal - characterized by severe muscle and joint pain, a rash on the body of the papular-macular type, swollen lymph nodes, intermittent fever, vomiting, meningeal syndrome. The latter is a tonic tension of the body muscles in combination with cerebral symptoms. The development of the disease is facilitated by toxoplasmosis, caused by Toxoplasma (a protozoan, i.e. protozoan intracellular parasite);
- fungal is a rather rare form of the disease that affects patients with pathologies of the immune system. Caused by cryptococci, Candida fungus, coccidia. After the pathogen enters the membranes of the brain, there is an increase in temperature to 37.2-37.9 degrees, loss of appetite, vomiting, drowsiness, lethargy, and lethargy. In severe cases, disturbances of consciousness and anxiety occur. In this case, meningeal syndrome is completely absent or mildly expressed.

Symptoms that appear in any form of the disease are fever, increased breathing, and irregular heart rhythm.
Meningitis can occur instantly, acutely or chronically. The severity is divided into mild, moderate, severe and extremely severe.
How to diagnose meningitis: home tests and hospital tests

Meningitis is a severe inflammatory disease that affects the membranes of the spinal cord and brain. To avoid unpleasant consequences, you must be able to diagnose it in time. The article will talk about how to get tested for meningitis and what needs to be done for this.
In most cases, this disease is diagnosed in children. For a variety of reasons, 85% of the incidence falls on them. In most cases, infants are most often affected. Until the early 20th century, the mortality rate from meningitis exceeded 90%. However, after antibiotics and other drugs became available, this figure decreased significantly. Recently, there has been an increase in the incidence rate again.
Description and symptoms
How the disease manifests itself depends on the pathogenetic type of infection.
Typically, the incubation period for meningitis is 5-6 days.
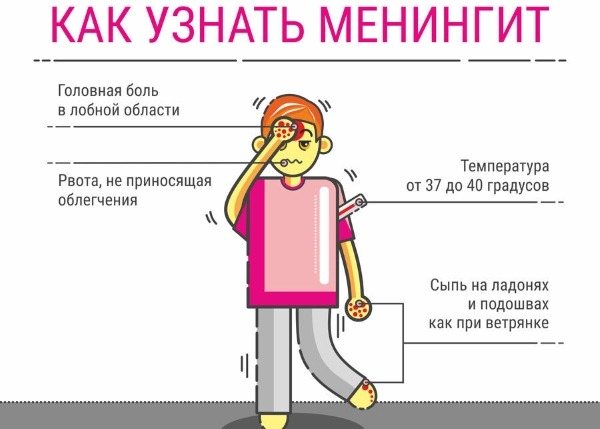
The main symptoms of the disease are:
- heat;
- headache;
- intolerance of light and sound;
- numbness in the neck;
- disturbance of consciousness;
- convulsions;
- vomit;
- fever;
- skin rashes.
The causes of the disease are called fungi, bacteria and viruses. Meningitis often appears as a result of a complication of a number of infectious diseases. Meningitis can also be fatal . Treatment of the disease should be carried out exclusively in a hospital setting under the strict supervision of a doctor.
The incidence of meningitis peaks in autumn, winter and spring. The following factors contribute to it:
- avitaminosis;
- hypothermia of the body;
- sharp temperature fluctuations;
- abnormal ventilation in rooms where there are a huge number of people.
Reference! Scientists have noticed that there is a 10-15 year cyclicality of the disease, when the number of patients in particular increases. The disease mainly develops in countries with poor sanitary conditions.
First of all, the presence of meningitis can be determined in advance using special tests that you can perform even at home.
Due to specific symptoms, they can immediately show whether a person is sick.
Kernig syndrome
A person is unable to straighten his legs bent at the knees. The patient is placed on his back and his leg is bent at the knee and hip joint at an angle of 90 degrees. If a person is sick with meningitis, he will not be able to straighten his legs after this.
What is the temperature with meningitis?
The temperature during meningitis in an adult and a child can vary depending on the form, severity of the disease, and its cause. Thus, the highest thermometer readings are recorded in purulent forms of the disease. They can reach 39-42 degrees, and the risk of dangerous complications for the body increases. Fever with purulent meningitis is resistant to the action of antipyretics, and the serous form is characterized by a subfebrile temperature when the thermometer shows 37-38.
There are several types of body temperature during meningitis:
- moderate (low-grade) – 37-38 degrees Celsius;
- high (pyretic) – 39-41;
- ultra-high (hyperpyretic) – 41-42.
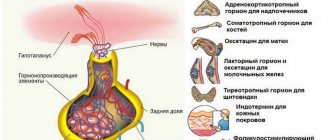
Fever is caused by the body's natural reaction to the penetration of the pathogen. To destroy it, the processes of producing pyrogens - substances that cause heat - are launched. Due to their production, the body heats up. And a part of the brain called the hypothalamus is responsible for the amount of pyrogens and their activity.
Low-grade fever
An increase in temperature to 37 with meningitis is observed at the stage of the incubation period, when the pathology is just developing. Basically, low-grade fever marks are characteristic of the following types of disease:
- serous meningitis at the initial stage - the thermometer shows values in the range of 37-37.5;
- tuberculous meningitis - low-grade fever is combined with general malaise, apathy, loss of appetite, and mild headaches. Such symptoms persist for 15-20 days, until the acute onset of the disease;
- protozoal - characterized by unstable fever, the thermometer may show 37-37.5, after which the thermometer may fall, or a sharp rise is noted;
- fungal meningitis - low-grade fever within 37.2-37.9 degrees appears in subacute and chronic forms of the disease, against the background of moderate clinical manifestations (drowsiness, weakness, vomiting).
Beware of meningitis!
The day before yesterday I asked for magic fists for my thirteen-year-old nephew, whose mother (my sister) suspected meningitis due to some circumstances and rang all the bells. Once again I thank everyone for their participation and warm wishes, despite the fact that the disease was, after all, confirmed. I want to bring up the topic and talk about it here and now for only one reason, to warn parents to be more attentive to their children and play it safe! My nephew had only one symptom out of many described on the Internet - he just had a headache. And only a happy coincidence made it possible to immediately suspect a dangerous disease.
Now in chronological order, as it was for us: 1. August 22, Thursday - returns from training camp at sea. 2. August 26, Monday - the temperature rises and the head begins to hurt. The temperature is brought down with antipyretics, headaches are relieved with painkillers. 3. August 27, Wednesday - the temperature jumps from 36.5 to 37.5 (with the help of antipyretics). The headache continues to hurt and does not hurt as much as usual. The boy is an athlete and has a training session scheduled for that day, which can be missed only for a good reason and after mandatory notification of the coach by the parents. The sister calls the coach and explains the reason for her absence. The coach will clarify what it hurts, how it hurts, how long it hurts, and whether there is a fever, and then gives information that one child from the team, upon arrival in Moscow, was hospitalized with meningitis. 4. My sister calls me in a panic and I immediately sent me to call an ambulance with the obligatory notification of a possible diagnosis. And then the fun begins. 5. The ambulance arrives instantly (in fact, incredibly quickly for Moscow - 5-7 minutes after the call). 6. The doctor examines the guy and diagnoses him with high cranial pressure. 7. Mother (my sister) insists on hospitalization, the emergency doctor is not sure of its necessity, etc. denies meningitis. But my sister (Thank God) insisted. 8. They brought me to the hospital and the doctor in the waiting room, even before taking the test, said: “our client.” Two doctors. One of them is the one on which human life primarily depends. And if there had not been knowledge of a case of meningitis in one of the team members, the sister would not have insisted on going to the hospital and the child would have been treated for high blood pressure. At home. In our case, we were incredibly lucky. I was lucky that my sister did not extend the child’s vacation and did not take a break from training until September (some children are still on vacation). And if she had taken this challenge, then, of course, she would not have needed to notify the coach about the failure to appear and would not have immediately learned about the precedent with the other boy. But this is all lyrics. But the truth is that the discrepancy between the symptoms and what is described on the Internet in no way excludes the disease.
And now about the symptoms (in black - from the Internet, in red - my comments, as we had):
Most often, meningitis is characterized by a sudden and acute onset. The first symptoms of meningitis resemble a severe cold or flu:
Fever (temperature more than 39 C) - on the first day the temperature was 37.5, which was brought down by antipyretics. The second one is the same and with the same reaction to the pills. Only in the hospital did it rise to 38.5, but the boy is terrified of doctors and such an increase in the rate could be at the vegetative level.
Weakness, lack of appetite - if there were any, they were not obvious. The child ate, but did not move much because of the headache.
Pain in muscles and joints - no complaints. Moreover, the nurse and the emergency doctor tested him for muscle stiffness and did not notice any abnormalities. At the specialized hospital we saw it right away!
Within a few hours or days, against a background of elevated temperature, specific (characteristic) symptoms of meningitis appear. Common signs and symptoms of meningitis include:
Strong headache. With meningitis, the headache is diffuse (the whole head hurts). Over time, the pain increases and becomes bursting. After some time, the pain becomes unbearable (adults groan from such pain, and children scream). Further, most often the pain is accompanied by nausea and vomiting. As a rule, headaches with meningitis intensify with changes in body position and the effect of external stimuli (noise, loud sound). The rash is characteristic of meningococcal meningitis. With a mild form of meningitis, the rash is represented by small pinpoint rashes of a dark cherry color. The rash with meningococcal meningitis disappears by 3-4 days of illness. In more severe forms of meningitis, the rash consists of large spots and bruises. The rash in severe meningitis disappears within 10 days. Confusion. Repeated vomiting that does not bring relief. Meningeal symptoms: severe tension in the muscles of the back of the head, severe pain that occurs when trying to tilt the patient's head to the chest or straighten his knees (patients with meningitis usually prefer to lie on their side with their knees brought to the stomach and their head thrown back). Strabismus (sometimes due to meningitis, cranial nerves are affected). we only had two days and thank God, we didn’t find out what was happening during the next days. Rash, vomiting, confusion, etc. we managed to avoid.
Our boy is now in the hospital. In the best case scenario, in 10 days he will be punctured again, and if no cells are found, then in another two days he will be discharged home. If they find it, they will treat it further. The doctor's prognosis for our case is good. Thanks to early treatment, the number of cells is low. But there will still be consequences. Albeit temporary. The child called and cried today. He is a sportsman. He takes part in tournaments, including international ones. Finally, he began to like what he was doing and began to succeed at it. At the last tournament in Spain he was the best in his team. In the new season, literally in a few days his candidacy was supposed to be nominated for the position of captain. But now, for at least six months, sports and even physical education lessons are strictly prohibited.
But this can all be fixed! The main thing is a timely diagnosis!
Take care of your children and loved ones. And thank you again for your fists and participation.
How long does the temperature last for meningitis?
Meningitis occurs with fever in most cases, but normally it should subside after 3-6 days of treatment. The exception is cases with a purulent form of the disease, when symptoms persist for 8-9 days.
It is impossible to give an unambiguous answer to the question of how long the elevated thermometer readings will persist; it depends on a number of factors:
- form of the disease - bacterial meningitis is more severe than viral meningitis, and the fever may last longer;
- general health condition and age of the patient - in children the clinical picture is more severe, as well as in older people: their hyperthermia lasts longer, which can prolong the length of hospitalization;
- timely start of treatment - the sooner the patient contacted a specialist, the higher the chance of stopping the infection in time, which is the cause of the fever.
The meningococcal form of the disease is considered the most severe. With it, swelling of the brain often occurs, the temperature rises sharply and seals form on the surface of the brain matter. The heat can persist for a long time, which delays the healing process.
Also, the duration of the temperature symptom depends on the timely identification of the pathogen. If you act on a specific bacterium, a decrease in temperature will be observed within 2-3 days.
Prevention
Prevention can be specific and nonspecific. Specific prevention includes vaccination.
The main vaccines to prevent bacterial and viral meningitis are: Meningococcal vaccine - provides protection against a number of bacteria that can cause meningitis. This vaccination is given to children 11-12 years old, and is also recommended for first-year students living in a dormitory, military recruits, tourists visiting places where there are epidemics of this disease;
- Vaccine against Haemophilus influenzae type B – intended for children aged two months to five years;
- Pneumococcal vaccine can be of two types: conjugation and polysaccharide. The first category of vaccine is intended for children under two years of age, as well as for at-risk children whose age does not exceed five years. The second type of vaccine is recommended for older people, as well as for middle-aged people whose immunity is weakened or there are certain chronic diseases;
- Vaccines against measles, measles rubella and mumps - are administered to children in order to prevent meningitis, which can develop against the background of these diseases;
- Vaccination against chickenpox.
Vaccinated children and adults may experience a variety of side effects, such as weakness, flushing, or swelling at the injection sites. In most cases, these symptoms disappear after one to two days. In a small percentage of patients, vaccines can provoke severe allergic reactions, which manifest themselves in the form of swelling, shortness of breath, high fever, and tachycardia. In such cases, you should consult a doctor, stating the date of vaccination and the time of occurrence of side effects.
Nonspecific prevention of meningitis is a series of measures aimed at increasing the body's immunity and preventing contacts with possible pathogens of the disease.
Features of temperature during meningitis in a child
Fever during meningitis in children is a dangerous phenomenon, as is the pathology itself. Whether the form of the disease is viral or bacterial, it requires emergency care, including the elimination of hyperthermia. Indeed, when the thermometer rises above 41, the child may experience hemorrhagic convulsions, which are often followed by a coma.
The temperature for meningitis caused by streptococcus, pneumococcus and meningococcus rises sharply in a child to 38-41 degrees and lasts for at least 5 days, because the child’s body is more sensitive to the effects of pathogenic microbes. When the membranes of the brain become inflamed, severe intoxication develops, which can be overcome by prescribing antibiotics and antipyretics. This will prevent the occurrence of seizures and other dangerous complications. Children with weakened immune systems may not have a fever, but if there are no symptoms, the consequences are even worse due to delays in seeking medical attention.
During the incubation period of the bacterial form of the disease, there may not be a high fever, since bacteria multiply more slowly than viruses. In the prodromal period (the stage of initial signs of the disease), the thermometer values rise to subfebrile, and at the stage of acute development of symptoms they reach 39-41. If antibiotics are prescribed on time, the temperature will subside after 3-5 days. With reduced immunity and an unknown type of pathogen, the child will feel worse, and the fever will last longer.
Types of meningitis in adults
Meningitis occurs for many reasons; there are several types, depending on the pathogen.
- Viral
. In most cases, the causative agent of the disease is enterovirus, flavivirus, varicella zoster virus, and herpes virus. Also recorded as causes are cytomegaloviruses, adenoviruses, lymphocytic choriomeningitis viruses, HIV, and Epstein-Barr virus. At the initial stage, the symptoms are similar to the flu, they can be confused, but after a few days headaches appear. The disease is mild and complications are extremely rare. - Bacterial
. Penetration of bacteria into the body causes a sharp deterioration in health, sometimes within the first 24 hours. The main pathogens are the following bacteria: meningococcal, Haemophilus influenzae, streptococcus. There are cases of infection with E. coli and Klebsiella. - Purulent
. Complications as a result of the disease may be accompanied by the appearance of accumulations of pus. Haemophilus influenzae, meningococci and pneumococci most often precede purulent meningitis.
- Tuberculous
. The onset of fever is the first sign; after a few days, vomiting and headache appear. After two weeks, the brain begins to suffer. - Meningococcal
. The dangerous disease is caused by the bacterium Neisseria meningitides. Signs of the disease include rash, fever and chills. The bacterium actively influences changes in blood composition and leads to inflammation.
Viral meningitis
As a result of the penetration of viral pathogens, damage to the membranes of the brain or spinal cord occurs. The most common cause of this type of disease is enteroviruses. A type is serous meningitis, which primarily affects children. Develops against the background of consequences after infectious diseases, such as measles, syphilis and others.
Often, outbreaks of mass diseases occur in the summer - while swimming in bodies of water with stagnant water. Water becomes a favorable environment for the proliferation of dangerous bacteria.
Viral meningitis occurs in different age groups, but is more common in children. Despite the risks of getting infected and getting sick, the chances of recovery with timely initiation of treatment are the highest and there are minimal side effects.
When the immune system works well, microorganisms die at the stage of penetration into the body; they do not manage to get to the membranes of the brain. Only when they enter a weakened body do the viruses become viable and are delivered to the head through the blood.
The first manifestations and reaction of the body are similar to ordinary viral infections: fever and gastrointestinal upset, myalgia, redness of the throat are typical signs familiar to the parents of every child. Later, the fever intensifies and the head begins to hurt severely. When you try to tilt your head forward, acute pain appears in the back of the head and in the cervical region.
Bacterial or meningoencephalitis
An inflammatory process occurs in the membranes of the brain. In some cases, a similar process occurs in the spinal cord. The cause of inflammation is pathogens such as meningococci, pneumococci or Haemophilus influenzae. Less commonly, staphylococci, enterococci and listeria act as pathogens.
Bacterial meningitis most often occurs in the age group over 55 years, children and youth from 16 to 25 years. A distinctive feature of the sick is a weakened immune system and a sedentary lifestyle, smoking, and drinking alcohol.
In rare cases, outbreaks of meningoencephalitis are recorded in individual territorial entities and are classified as an epidemic.
An infected person can infect a large number of people:
- bacteria are transmitted by airborne droplets during conversation, coughing, sneezing;
- through dirty hands;

- when sharing common household items, for example, cups;
- There are cases of infection while swimming in dirty stagnant water;
The first symptoms of the disease appear on the 2nd day; in some cases, the incubation period is 10-12 days. After 24-72 hours, there is a sharp increase in body temperature to 380C, and acute nasopharyngitis appears.
The presence of bacteria in the bloodstream is accompanied by chills, attacks of fever and headache, and an increase in body temperature up to 400C. A characteristic feature of this type of disease is that the temperature is practically impossible to reduce with antipyretic drugs. In this case, the general condition of the patient deteriorates, to which weakness, nausea and vomiting are added. The headache intensifies with loud sounds and bright light, and the patient is unable to press his chin to his chest. A rash appears on the body in the area of the buttocks, abdomen and legs in the form of pink spots, quite large in size - up to 20 mm.

There is a proven way to determine meningitis at home, which is used by medical professionals. To do this, the patient is asked to lie on his back and turn his head with his hands. If involuntary bending of the leg at the knee or pulling towards the stomach occurs, this is a clear sign of a progressive disease. As an alternative method, the reaction to light and sound is checked - painful sensations also serve to confirm the diagnosis.
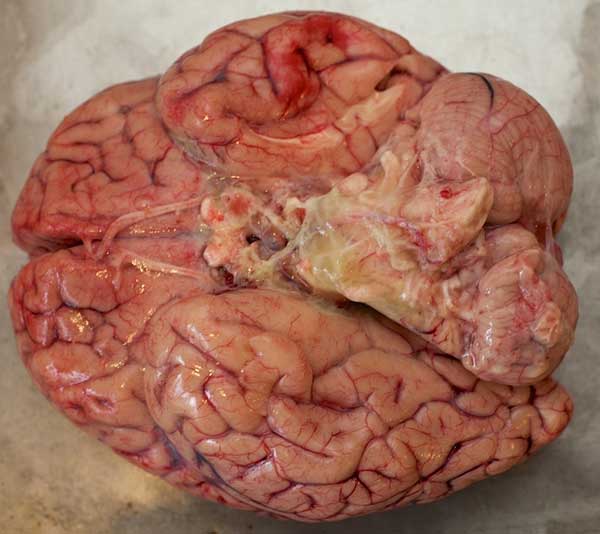
Purulent meningitis
As a result of the disease, the membranes of the brain are affected - the formation and accumulation of pus occurs. It is characteristic that all groups of the population are at risk - from birth to death.
The causative agent is microorganisms that penetrate the membranes of the brain. The most common are staphylococci, which is why this type of meningitis is sometimes called staphylococcal. Streptococci, pneumococci and Pseudomonas aeruginosa also often act as dangerous pathogens.
Purulent meningitis affects people with weakened immune systems and is dangerous for children.
Methods of infection:
- airborne;
- food;
- domestic;
The peculiarity of the course of the disease after infection is its gradual penetration into the body. At the initial stage, microorganisms enter the body through the mucous membrane or with food. Penetrating into the blood, microorganisms do not manifest themselves until they reach the membranes of the brain. Only at the last stage of transportation does the development of an infectious disease begin.
Tuberculous meningitis
In modern society, this type of inflammation of the meninges is rare. The disease develops against the background of tuberculosis, acting as a secondary disease, typical for the adult population. Tuberculosis is spread not only by sick people, but also by animals and birds.
The cause is microorganisms that cause inflammatory processes in the lungs - tuberculosis microbacteria. The circulatory system serves as a kind of transport for them to enter the brain area. Only after reaching the membranes does the development of tuberculous meningitis begin.

After 14 days, the brain is affected, after which death occurs or the person becomes disabled. The mortality rate from this type of meningitis due to late recognition is about 20%.
Methods of infection with tuberculous meningitis:
- airborne;
- food;
- domestic;
- contact.
The peculiarity of tuberculous meningitis, like tuberculosis itself, is that with strong immunity, microorganisms are destroyed immediately. At risk are people with chronic diseases, weakened immune systems and children.
Meningococcal meningitis
The danger lies in the high mortality rate from meningitis of this type. In every second case, the patient dies if treatment is delayed. Medical care from the first days reduces mortality by up to 20%.
The onset of the disease is provoked by past pneumonia or sinusitis. The danger is that symptoms appear late and are masked by signs of underlying diseases. The disease, discovered at an early stage, develops rapidly. A distinctive feature is convulsions, incoherent speech, and impaired consciousness even in the first days.

Treatment of meningitis with fever
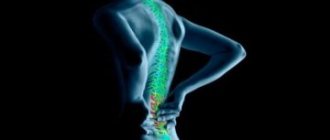
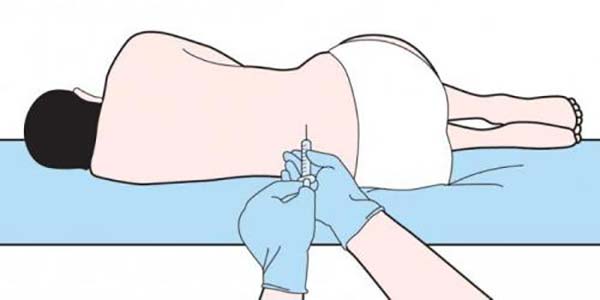
If there is a high temperature with meningitis and dangerous symptoms develop, then the patient needs hospitalization. The clinic performs diagnostics, which consists of examining cerebrospinal fluid, determining sugar and protein levels.
The basis of treatment is the prescription of antibiotics - they will help kill germs and lower the thermometer readings. Sulfonamides “Etazol”, “Norsulfazol” or penicillin drugs are used. In severe cases, benzylpenicillin is infused intralumbarally, i.e. into the spinal cord.
If the fever does not decrease during the first three days of therapy, the drugs are replaced with semi-synthetic ones. A combination of ampicillin, oxacillin or carbenicillin with gentamicin or nitrofurans is effective. This combination can be used for 10-14 days, after which they switch to administering one type of drug, provided that the temperature and general clinical picture are normalized.
For mild viral meningitis, you can limit yourself to prescribing general restorative drugs plus those designed to eliminate general symptoms. These are vitamin complexes, glucose, Methyluracil, antipyretics and drugs from the NSAID group (non-steroidal anti-inflammatory drugs).
If the temperature continues to rise, a repeat puncture of the cerebrospinal fluid is performed to determine the layer of bacterial infection. Then corticosteroids, diuretics and strong medications against hyperthermia are prescribed.
What does temperature after meningitis mean?
The presence of low-grade fever after meningitis may indicate an untreated disease if antibiotics were stopped ahead of time and the pathogen remained to multiply in the body. Also, a symptom may indicate a severe weakening of the body, when even a minimal negative impact (ARVI, hypothermia, stress, fatigue) is responded to by a temperature reaction.
The reason for the increase in thermometer readings during the recovery period may be a disruption of the central nervous system. In this case, the functioning of the nerve centers responsible for temperature control of the body is disrupted. Doctors also talk about disturbances in the functioning of the endocrine system, in which hormonal imbalances cause hyperthermia syndrome.
In any case, if the patient has even a slight fever within 10-14 days after treatment of meningitis, it is better to consult a specialist to find out the causes of this phenomenon.
Conclusion
Meningitis is a dangerous disease that leads to the death of the patient due to lightning-fast development and a sharp increase in temperature to critical levels. To prevent death and other unfortunate complications (loss of vision and coordination in space, neurological and mental problems), you should pay attention to the symptoms in time. Fever is one such sign. If you experience severe headaches, repeated vomiting with a strong jump in temperature, you should urgently consult a doctor. These symptoms often indicate meningitis.
source
Why is urgent help needed?
Having heard from the doctor: “The child has a suspicion of meningitis,” any mother, without further ado or argument, begins to get ready for the inpatient department of the infectious diseases hospital. And this is not surprising, because less than 50 years have passed since doctors learned to treat meningitis. And the mortality rate among children from this disease was reduced by only half. Compared to other childhood diseases, this is a very modest figure.
Meningitis is a real threat to life, so there is no need to wait for the most severe symptoms of this disease to appear. And if there is a rapid increase in temperature, headache and rash on the body, consult a doctor immediately.
Does the temperature increase with meningitis?
Very often, patients suffering from meningitis mistake it for a simple migraine. Most of them do not even realize that they are developing a serious disease that poses a real threat to human health and life. But how to diagnose the inflammatory process in order to prevent serious consequences and what is the temperature for meningitis accompanied by a febrile state.

Types of pathological syndrome
Meningitis is an inflammation of the lining of the brain and spinal cord. Pathology in 50% of cases occurs in childhood, but despite this, an adult can also get sick.
Depending on the cause of the development of the inflammatory process, the following types of meningitis are distinguished:
- Infectious.
- Traumatic.
- Infectious-allergic: microbial and neuroviral (herpes, influenza, serous meningitis, tuberculosis).
- Fungal.
By location: panmeningitis, leptomeningitis, pachymeningitis. Meningitis is also divided into purulent and serous types, secondary (against the background of the underlying disease, the infection spreads to the membranes of the brain) and primary (the disease immediately affects the “gray matter”).
In almost all cases, meningitis occurs in an acute form, with the exception of the tuberculosis type of pathology; it can develop gradually over 2 weeks or several months.
According to the methods of infection, meningitis is classified as:
- perineural;
- hematogenous;
- contact;
- lymphogenous.
Meningeal symptoms - high intracranial pressure, observed with any type of inflammatory process, characterized by severe pain in the head, a feeling of “pressure” on the eyes, ears, a feeling of nausea and vomiting, a reaction to extraneous noise, photophobia, most often meningitis is accompanied by fever.
Consequences
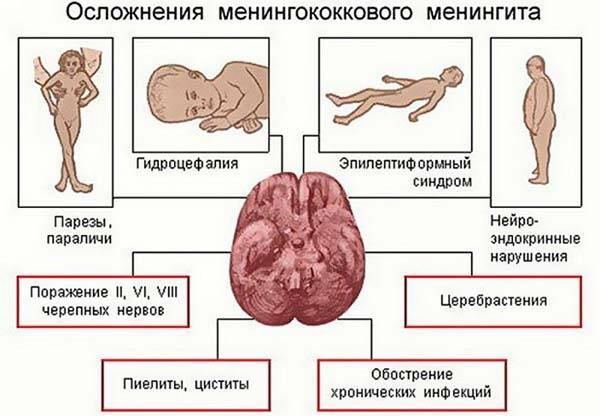
Regardless of the type and degree of neglect, meningitis in adults almost always entails serious complications and consequences, since the infection affects the brain. Complications can appear both immediately during the course of the disease and in a delayed period. In the first case, the patient may develop:
- Cerebral edema - there is a disorder of consciousness, sharp fluctuations in blood pressure, tachycardia and shortness of breath with symptoms typical of pulmonary edema.
- Infectious-toxic shock - occurs against the background of poisoning of the body with decay products of bacteria that provoke the development of meningitis.
In both cases, if emergency care is not provided by resuscitators, the patient may fall into a coma and die 2-3 hours after the onset of the active phase of complications.
The delayed consequences of meningitis in adults, suffered in a mild form, may appear in the form of symptoms in the next six months:
- monotonous and frequent headaches;
- decreased memory and mental functions;
- convulsions that occur spontaneously without specific causes.
The consequences of severe meningitis are more serious. Throughout the rest of his life, a person may experience the following pathological conditions caused by a disorder of cerebral activity:
- epileptic seizures;
- restrictions on mental, speech and motor functions depending on which part of the brain is affected by the infection;
- paralysis of limbs or individual parts of the body;
- hormonal imbalance, which leads to disruption of metabolic processes and brain function as a whole;
- deafness (partial or complete);
- hydrocephalus.
Causes of the pathological condition
People of all ages are susceptible to infections of viral origin, but most often children 5 years of age and older are infected with meningitis. The risk of developing an inflammatory process in infants is minimal; mother's milk protects against a dangerous illness.
Factors that can provoke the appearance of the disease:
- Enterovirus 71 subspecies.
- Visiting overcrowded kindergartens and schools.
- Poor quality of life.
- Chronic pathologies that occur in severe form.
- Lack of personal hygiene.
- Diseases of the nervous system.
- Back and skull injuries.
- Weakened immune system.
A viral type of meningitis occurs in a mild form and goes away on its own if it does not develop into encephalitis - inflammation of the brain.

Possible complications after inflammation
Delayed treatment can lead to serious consequences. So, among the complications of a dangerous disease there are:
- Loss of vision (partial or complete).
- Strabismus.
- Paralysis of limbs.
- Bedsores.
- Delays in child development.
The best prevention of inflammation of the spinal cord and brain is strengthening the body's defenses: proper nutrition, hardening, personal hygiene. It is necessary to promptly treat viral and infectious pathologies, this will prevent the development of the disease.
The duration of therapy for the disease depends on its degree and form. With a late consultation with a neurologist, sometimes it is not possible to save a person’s life. Timely, adequate treatment is the key to a quick recovery, but recovery can take many years.
Whether meningitis occurs without fever can be determined by your doctor after a full examination. To prevent the inflammatory process, doctors prescribe special vaccines that are valid for 4 years. But the vaccine is not effective against some types of infection. You should carefully monitor the condition of your body and at the first dangerous symptom, contact your doctor.
source
Symptoms of the pathological syndrome
Meningitis can develop regardless of the time of year, but with the arrival of cold weather, along with flu and colds, cases of infection are observed more often. Signs of the syndrome can be different; timely diagnosis significantly increases the chance of a quick recovery without health consequences.
With inflammation of the membranes of the brain and spinal cord, there is most often an elevated temperature, indicating the occurrence of a pathological process, which can rise to significant limits. It is recommended to knock it down with the help of drugs recommended by your doctor.
The temperature during the inflammatory process can be as follows:
- febrile – 38-39 degrees;
- pyretic – 39-40 degrees;
- hyperpyretic temperature - up to 41 degrees.
Signs of pathological syndrome in children
The clinical symptoms of meningitis are the same as in adult patients, but other manifestations of the inflammatory process are also characteristic of early age.
Signs of the disease may be as follows:
- Regurgitation of food.
- Stool disorder.
- Drowsiness, apathetic state.
- At high temperatures, the extremities remain cold.
- While sitting, the child throws back his head and leans forward.
- Tense chest and back muscles.
- Constant crying.
- Poor appetite.
- Swelling of the fontanelle.
The incubation period is short, meningitis develops quite quickly (sometimes up to 10 days). The symptoms of inflammation of the membranes of the brain and spinal cord can easily be confused with the flu. The weaker the immune system, the more severe the patient’s condition.
Symptoms of different stages of the disease
The following signs predict the disease in a patient:
- Severe cramps;
- Pale complexion, blue lips;
- Lethargy, general weakness;
- Muscle pain;
- Hands and feet get cold.
Further development of meningitis is characterized by fever, headache and vomiting (regardless of food intake).
Characteristic symptoms of meningitis, which indicate a high level of inflammation, are:
- The patient feels a persistent headache, feels nauseous and chills. There is a very high body temperature;
- A painful reaction to light appears;
- The patient feels weak and drowsy almost all the time;
- Loss of flexibility in the neck muscles. The patient cannot turn or tilt his head without severe pain. When the head is tilted, the muscles of the limbs involuntarily contract;
- Pain appears in the neck, back of the head, and back;
- Skin rashes are a characteristic sign of meningitis;
- Along with the appearance of severe convulsions, clouding of consciousness occurs;
- The pressure drops sharply, the pulse and breathing quicken, and the patient may suffocate.
The insidiousness of the disease is manifested in the fact that it can arise and develop rapidly. Specific symptoms of meningitis may be observed within 3-4 hours.
Methods for diagnosing the inflammatory process
The diagnosis can be made based on the results of a study of cerebrospinal fluid. If it is confirmed, then the composition of the fluid determines the type of meningitis - purulent or serous, and complex therapy is prescribed.
Diagnostics also includes other methods:
- study of the fundus;
- electroencephalography;
- X-ray of the skull;
- CT and MRI of the brain.
The diagnosis of a dangerous disease is made in the presence of several factors: signs of the virus, symptoms of meningitis, characteristic changes in the cerebrospinal fluid.

Diagnostics
A meningitis rash makes diagnosing the disease much easier. However, there are cases when this characteristic symptom is not present. Then additional methods of examining the patient are used:
- Nasal discharge is analyzed. Testing the fluid may reveal the presence of bacteria such as pneumococcus in the body.
- Accurate diagnosis of meningitis is possible by taking a puncture. This is a rather unpleasant procedure. However, analysis of cerebrospinal fluid from the lumbar spine makes it possible to quickly determine the type of meningitis and prescribe adequate treatment.
- Testing the patient for the presence of Kernig, Hermann, Brudzinski, etc. symptoms. For example, according to the Kerning system, a patient with meningitis has difficulty straightening the knee while the person is sitting, and the Brudzinski test tests the ability to pull the knees towards the abdomen while trying to pull the chin towards the chest.
- Disturbances in the functioning of joints are common consequences of the development of meningitis. But it can be difficult to determine them on your own, without the help of a doctor.
After receiving all the results of the study, the doctor prescribes treatment, which must be started immediately.
Reactive brain inflammation
An acute form of bacterial syndrome that develops at lightning speed. Purulent infections affecting the membranes of the “gray matter” cause a coma and death of the patient. The causes of the disease are meningococci, streptococci, pneumococci. The disease can manifest itself as a consequence of pneumonia or sinusitis.
The primary signs of meningitis are:
- High temperature, which is not knocked down by anything.
- Hardening in the neck and back of the head.
- Migraine attacks, sore throat.
- Constant vomiting.
Reactive meningitis can be fatal within 24 hours. In some cases, even correct diagnosis of the disease will not help to avoid negative consequences - aseptic shock.

Serous type inflammation
The cause of this type of disease is a serous inflammatory process that occurs in the membranes of the “gray matter”. Based on its origin, meningitis is divided into types such as:
- viral illness;
- bacterial meningitis: tuberculous, syphilitic;
- fungal.
The development of acute serous disease is influenced by viruses of various etiologies. The pathology is accompanied by high fever, which in many patients was brought down only by strong medications; simple antipyretics had no effect. The virus affects the central and peripheral nervous system.
Causes
Any infectious agents that penetrate the soft meninges can cause meningitis. The main causative agents of meningitis, as a rule, are bacteria and viruses; less often they encounter infection with protozoa and yeast fungi. More often, a person becomes infected with meningococcus, tuberculosis bacillus and Afanasyev-Pfeiffer bacillus. Less common: pneumococci, staphylococci and Haemophilus influenzae streptococcus.
The causes of childhood meningitis are usually enteroviruses that enter the body with food, water and contaminated objects; they can also spread against the background of chickenpox and rubella.
Adult patients are characterized by a bacterial form of the disease caused by Neisseria meningitidis and Streptococcus pneumoniae. Microorganisms can inhabit the mucous membranes of the respiratory tract and not manifest themselves in any way, but when the body’s defenses are reduced, they penetrate the membranes of the brain, where they cause severe symptoms of the disease.
Group B streptococci often cause the disease in newborns; infection can occur during childbirth or in the postpartum period. Listeria can cause disease in infants, debilitated people and the elderly. In rare cases, the causative agent of meningitis is Klebsiella, or Escherichia coli. This pathogen provokes the disease due to brain injuries and blood poisoning.
The main routes of transmission of meningitis are:
- airborne;
- fecal-oral;
- insect and rodent bites;
- transplacental.
Meningitis can occur as a complication of other infectious processes occurring in the body. Infectious agents penetrate the lining of the brain in different ways. The most common is hematogenous. It is also possible to spread the infection by lymphogenous route.
If the source of inflammation comes into contact with the meninges, a contact route of transmission is likely. It is promoted by purulent otitis media, frontal sinusitis, brain abscess, mastoiditis and sinus thrombosis of the brain. Open injuries to the spine and head with leakage of cerebrospinal fluid create a gateway for infection.
Treatment of dangerous syndrome in adults and children
Meningitis is a serious pathological condition that requires emergency, adequate therapy. Patients with inflammation of the brain and spinal cord require urgent medical attention in a clinical setting. It is unacceptable to treat meningitis at home without the help of doctors, as this can cause the death of the patient.
The sooner you start therapy, the greater the likelihood of recovery. Treatment of the pathological syndrome includes taking antibiotics, which are the main method of complex treatment.
It is impossible to determine the type of pathogen using a blood test in 20% of situations. Usually, during the inflammatory process, medications are prescribed with an unknown cause for the manifestation of the pathological syndrome.
The drug is selected so as to cover the entire spectrum of the most common pathogens. The duration of treatment with antibiotics is 10 days or more; drugs must be taken for 7 days from the moment the temperature normalizes for infectious meningitis.