Group of neurodegenerative diseases
This group of diseases is characterized by damage to the central nervous system. A certain number of neurons die, and this leads to neurological pathologies. Neurodegenerative diseases can have different causes and different clinical manifestations. It is characteristic that all diseases in this category are incurable. All therapy used is symptomatic. That is, it alleviates the manifestation of the disease, but does not in any way contribute to the regeneration of damaged areas. The most effective would be a transplantation of nerve tissue, but the method has both technical and moral obstacles. Similar diseases include Alzheimer's, Parkinson's, and Farah's diseases. As a rule, diagnosing such diseases in the early stages is difficult. Most often, when making a diagnosis, specialists rely on patient complaints and the results of observations of their behavior. But the main tool is tomography (computer, magnetic resonance).
General information
The main characteristics of the group of degenerative diseases of the central nervous system are the following criteria:
- diseases begin unnoticed; before their appearance, the nervous system could function absolutely normally;
- diseases have a gradually progressive course and can last for years or decades;
- some degenerative diseases are associated with hereditary factors and develop in several members of the same family;
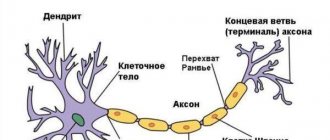
- a neurodegenerative disease of the central nervous system is characterized by the gradual death of neurons and their replacement by glial elements;
- atrophic processes at the initial stage of pathology development occur in a specific area of one of the cerebral hemispheres; further, during the advanced stage of degeneration, atrophy in the brain becomes almost symmetrical.
Various diseases of the central nervous system, the list of which is quite long, remain under study. The reasons for the occurrence of atrophic processes during the normal functioning of the nervous system for most of a person’s life are not reliably known. However, there are a number of factors that can trigger brain degeneration:
- alcohol abuse, drug addiction;
- toxic effects of pesticides and herbicides;
- meningococcal infection;
- viral encephalitis;
- deficiency of vitamin B12 and folic acid.
The danger of degenerative diseases of the central nervous system is that they are difficult to predict. If there are provoking factors in a person’s life, it is recommended to lead a healthy lifestyle and regularly visit a neurologist for preventive examinations. If you suspect signs of a central nervous system disease, you should immediately consult a doctor. The earlier the disease is detected, the greater the chance of slowing down the progression of degenerative processes in the brain.
Diagnosis and treatment of degenerative diseases will depend on the type of pathology. Having determined the clinical picture of the disease, the doctor will prescribe tests to clarify the patient’s condition. These may include laboratory tests, ultrasound, MRI, CT, and psychological tests to determine the status of cognitive skills.
At the Yusupov Hospital in Moscow there is a neurology clinic, where highly qualified neurologists and doctors of sciences provide assistance. Doctors at the Yusupov Hospital have extensive experience in treating degenerative diseases of the central nervous system and use the latest methods of therapy and rehabilitation in their work, which allows them to take on the most complex cases.
You can ask for help, make an appointment and get advice from specialists by phone.
Neurologist, director of the chronic pain clinic
The list of such diseases is quite long, and they occur so often that doctors are already talking about neurodegeneration as a big problem of the 21st century. The leaders of the “neuron killers” are Alzheimer’s and Parkinson’s, or rather, diseases named after the scientists who described them.
It is generally accepted that these pathologies, as well as neurodegenerative diseases in general, are the lot of older people. However, there are many cases where both diseases begin at a young age, literally as soon as the brain stops growing.
And it is in youth that hyperprolactinemia mainly develops, a pathology in which too much of the hormone prolactin is produced. The death of neurons in this disease causes inhibition of reproductive function, infertility, and at an advanced stage the disease provokes a pituitary tumor.
There are two groups of neurodegenerative diseases: sporadic and irritative. Sporadic diseases include Alzheimer's disease, multiple system atrophy, parkinsonian dementia, progressive supranuclear palsy, and dementia with Lewy bodies.
Irritative diseases include Wilson-Konovalov's disease, Hallervorden-Spatz's disease, Fahr's disease, Bessen-Kornzweig's disease and Gettington's chorea.
Fahr's disease includes cases of primary idiopathic calcium deposition in brain structures; secondary forms of cerebral calcification are not considered within this pathology. The first detailed descriptions of the disease were made in 1930 by the German neurologist K.T. Farom. Fahr's disease is a rare nosology, the prevalence is less than 1 case per 1 million population.
READ MORE: Cerebellar syndrome as a symptom and consequence of neurological disorders
Gender differences in incidence are expressed by a ratio of men to women of 2:1. Pathology manifests itself at any age, most often at 30-60 years. It is detected intravitally in only 1-2% of cases, which is explained by the presence of asymptomatic variants of the course, diagnosis of the disease under the guise of other neurodegenerative processes (Parkinson's disease, senile chorea).
Fahr's disease
Symptoms of the disease
Since this disease is a rather rare phenomenon, it is difficult for specialists to provide the correct clinical picture of the syndrome. Symptoms may appear if the patient is over 40 years of age. In younger people, Farah's disease symptoms may be vague and vague. Patients have impaired coordination of movement and parkinsonism. Also, the development of the disease may be indicated by such signs as tremor, dystonia, rapid and erratic movements of the limbs (chorea), involuntary contractions of the hands and feet. Since the disease affects areas of the brain, performance and mental capabilities decrease. A person’s memory also suffers. Speech is often impaired. Other neurological signs include pain and mental disorders. There is a juvenile form of the disease, which manifests itself in children and adolescents. The main symptoms are: dystonia, chorea, epileptic seizures. The senile form is typical for middle-aged and older people. In this case, parkinsonism, speech disorders, and other problems in the functioning of the nervous system are observed. Urinary incontinence may also occur.
Classification
In practical neurology, Farah's disease is divided into two clinical forms, differing in the age of manifestation and the type of predominant symptoms:
- Juvenile form - the onset of the disease occurs in childhood or adolescence. Extrapyramidal disorders in the form of athetosis, chorea, and muscular dystonia are characteristic. The pathology may be accompanied by oligophrenia. As people grow older, hyperkinesis changes to parkinsonian symptoms.
- Senile form - manifests in old and middle age. The clinical picture is characterized by the dominance of parkinsonian symptoms in combination with cognitive disorders. Progressive dementia is typical.
In practical neurology, Farah's disease is divided into two clinical forms, differing in the age of manifestation and the type of predominant symptoms:
- Juvenile form - the onset of the disease occurs in childhood or adolescence. Extrapyramidal disorders in the form of athetosis, chorea, and muscular dystonia are characteristic. The pathology may be accompanied by oligophrenia. As people grow older, hyperkinesis changes to parkinsonian symptoms.
- Senile form - manifests in old and middle age. The clinical picture is characterized by the dominance of parkinsonian symptoms in combination with cognitive disorders. Progressive dementia is typical.
Possible causes of Fahr syndrome
The reasons why the disease may develop have not been precisely established. However, it is known that disorders of the thyroid and parathyroid glands have a huge impact on its occurrence. In this case, disruptions occur in the metabolic processes of calcium and phosphorus. Similar neurodegenerative diseases can also occur when the acid-base balance in the body is disturbed. Alkalosis leads to significant loss of acids. But alkaline compounds are present in excess. There is also an opinion that Fahr syndrome occurs due to genetic disorders. That is, the gene that is responsible for the exchange of an element such as calcium mutates. However, this version has many contradictions. There are isolated cases where symptoms of the disease appeared after irradiation of the head area, poisoning with poisons, lead, in children with Down syndrome. Calcinosis has also been diagnosed in people who have had rubella (rarely). Another possible cause of basal ganglia calcification is birth trauma.
Research methods for diagnosis
Before the advent of computed tomography, patients underwent X-ray examinations of the brain. Thanks to the advent of modern research methods, specialists received more informative pictures from the affected area. However, it is worth noting that computed tomography rather than magnetic resonance imaging has greater sensitivity for this clinical picture. When analyzing most images, the affected areas are limited to the globus pallidus. They are small in size. Most often, the basal ganglia, thalamus, and cerebellum undergo changes. The level of calcification is approximately the same in young and elderly people. Also, no differences were found between groups in which Farah's disease is asymptomatic and those in which the syndrome is accompanied by pronounced symptoms.
Histological studies
When conducting a postmortem examination, the following picture is observed in the brain: the vessels have a whitish appearance (some branched areas). When touched by a knife, they make a sound similar to a crunch. For histological analysis, material is collected: sections of the cerebral cortex, basal ganglia, and cerebellum. It is in the area of the latter that calcification occurs most often. The samples contain calcium salts. They are also most often detected on arteries (small, medium-sized) and capillaries. Less commonly (in isolated cases), Farah's disease affects the veins. Small calcium conglomerates are found along the entire length of the vessels, as well as in adjacent tissues. The presence of traces of arsenic, aluminum, cobalt, and mucopolysaccharides is also detected in the tissues.
Pathogenesis
The pathogenetic mechanisms that form the disease have not been fully determined. Genetically determined changes in cerebral metabolism are assumed, causing the deposition of excess calcium in the brain tissue. Severe calcification of subcortical formations causes disorganization of the frontal-subcortical system, which regulates voluntary movements and provides cognitive functions (memory, thinking, attention).
Morphologically, calcifications are found symmetrically in various structures: the cerebral cortex, white matter, subcortical ganglia, internal capsule, cerebellum, walls of small arteries, and less commonly veins. The presence of perivascular small calcium conglomerates is characteristic. The most massive calcification is detected in the subcortical regions.
Establishing diagnosis
Depending on whether Farah disease has symptoms, making a diagnosis can be somewhat more difficult. It is often diagnosed accidentally, when a tomography is performed to confirm a completely different disease. First of all, the specialist excludes calcium metabolism disorders and other developmental defects. Then a computed tomography scan (or x-ray examination) is prescribed. Doctors note that one of the problems in making a correct diagnosis is hypoparathyroidism. This is a disease that occurs due to parathyroid hormone deficiency. As a result, the level of calcium in the blood decreases, and the level of phosphorus increases. If calcification of the striopallidodentate structures is observed on a CT scan, then additional tests are necessary to distinguish hypoparathyroidism from a condition such as Fahr's disease. First of all, it is important to determine the level of parathyroid hormone and calcium. Also, when making a diagnosis, parasitic damage to the nervous system is used. Specific reactions occur in the blood and cerebrospinal fluid. Fahr's disease is rarely differentiated from a condition such as Bourneville's sclerosis.
Neurodegenerative diseases: not just for the elderly
All of these diseases, which have neurodegenerative disorders, cannot be treated. These processes occurring in the cerebral cortex and central nervous system are irreversible and dead nerve cells cannot recover and resume lost functions.
The patient is not given up; he is seen by a doctor with regularity, which is established by the leading specialist. The attending physician develops a set of medications that serve as support and respite for the patient. They are aimed at slowing the progress of the disease, eliminating some symptoms and relieving pain.
Such patients require constant care and attention, because they are no longer able to do many things on their own. They should not be left unattended, but their presence in society is also unsafe, so it is worth isolating them. Comprehensive treatment includes the support of family and friends, which is indispensable in the process of treatment measures.
The list of medications is prescribed purely individually, because each individual case is unique in its own way. The direction of treatment depends on the causes of the disease, complications and characteristics of the patient’s body. To improve brain nutrition, nootropics are prescribed, to calm the nervous system, antipsychotics, sedatives, and in some cases antidepressants.
These complex diseases often cause deep depression in patients who may have suicidal tendencies and therefore require strong medications, but they all have many side effects. They can be adjusted and changed during the treatment period, and a different dose can be selected.
For each patient, a set of training exercises is developed that improve memory and intelligence, but they will be beneficial only in the initial stages, when the progress of the disease is not so strong and the patient has not completely lost his mind.
It is important to monitor nutrition, diet and regularity, because due to poor memory and forgetfulness, the patient may skip main meals. It is better to feed the patient strictly on time, using a special diet.
Folk remedies in this case are absolutely powerless; there is no substitute for strong medications. You can use infusions and decoctions only as an additional remedy; alcohol tinctures are also allowed.
Since the pathogenesis of the disease remains unclear, therapy is predominantly symptomatic. In order to improve metabolic processes, tissue metabolism stimulants (acetylcarnitine, glutamic acid, L-citrulline malate complex, nicotinamide), cytoprotectors (riboflavin, succinic acid, meldonium) are used.
For symptoms of parkinsonism, it is preferable to prescribe levodopa pharmaceuticals, for hyperkinesis - anticholinergics, benzodiazepines. The presence of epileptic seizures is an indication for treatment with modern anticonvulsants (levetiracetam). Complex therapy uses physical therapy, hydrotherapy, and cognitive training.
Currently, there is no effective treatment that eliminates the cause of the disease. Depending on the symptoms, various medications are used to relieve or suppress the symptoms of Farah disease. If signs of depression, anxiety or other mental disorders appear, drug treatment is used as standard against these diseases.
READ MORE: Treatment of Irritable Bowel Syndrome
Epilepsy is treated with antiepileptic drugs, and oxybutynin is used for urinary incontinence. The regulation of calcium phosphate dehydrogenase is sometimes beneficial in reducing movement disorders. Due to differences in the severity of symptoms, it is difficult, however, to predict the prognosis of a particular person who develops Fahra disease. The mortality rate when this disease occurs is high. The disease can also lead to progressive disability.
We do not yet know how to treat neurodegenerative diseases, although we have known about them for a very long time. You can only carry out symptomatic therapy, slow down some diseases, and alleviate the condition.
But today there are already breakthroughs in diagnostics: scientists say that the first signs of Alzheimer’s and Parkinson’s diseases can be detected at the very beginning, when the death of neurons has not yet affected the person externally, and he feels completely healthy.
Such diagnostics are not widespread yet. But what can definitely be done today is to start preventing such diseases. It's not complicated. All that is required is a healthy lifestyle with physical activity, a change in diet (the Mediterranean diet works great) and active exercise on the brain: chess, gardening, learning a foreign language or playing a musical instrument.
All this is the key to the formation of new connections between such small but important neurons for us.
Senile dementia: can it be avoided?
Health
Treatment
Removing calcium deposits that have formed in the brain and its vessels is impossible. As a rule, treatment of such a disease is symptomatic. First of all, it is aimed at improving the metabolism of calcium and phosphorus in the body. If symptoms of Parkinson's disease are observed, the specialist prescribes special medications (levodopa). Also, Farah's disease, treatment of its manifestations, involves taking antioxidants and means to improve metabolism. Therapy with calcium channel blockers is ineffective. It is worth considering the fact that the disease is quite rare and little studied. In most cases, therapy reduces the symptoms of the disease, but does not affect the degree of calcification.
Chapter 2: "Far's Disease"
Book: “Rare neurological syndromes and diseases” (V.V. Ponomarev)
Fahr's disease (idiopathic non-atherosclerotic symmetrical intracerebral calcification of the basal ganglia) is a rare neurodegenerative disease first described by T. Fahr in 1930 [3]. A characteristic radiological sign of Fahr's disease (FD) is massive calcification of the subcortical ganglia (usually the globus pallidus) and the genu of the internal capsule. Less commonly, similar disorders are widespread and are found in the cerebral hemispheres and cerebellum [5, 6, 12]. Clinical manifestations of FD are varied and do not correlate with morphological data. Neurological symptoms of the disease include various extrapyramidal disorders (rigidity, tremor, hyperkinesis), transient or persistent pyramidal signs, epileptic seizures, and dementia [1, 2, 7]. The clinical picture of FD often includes manifestations of hyper- or hypoparathyroidism in the form of focal convulsions, tetanic spasms, pain in the distal extremities, and positive Khvostek and Trousseau symptoms [8, 11].
FD occurs at any age. Conventionally, three groups of patients are distinguished:
1) young people with signs of cerebral calcification; 2) patients with hypoparathyroidism; 3) elderly patients with relatively small calcification [5].
The etiology of FD has not been definitively established. The main pathogenetic mechanism for the development of the disease is a violation of phosphorus-calcium metabolism. Its main cause is considered to be primary (autoimmune) or postoperative endocrine adenomatosis of the thyroid or parathyroid gland [7, 9, 12]. Another possible mechanism for the development of the disease is called chronic respiratory alkalosis, leading to various electrolyte disturbances (hypercalcemia, hyponatremia) and, as a consequence, to the development of brain hypoxia [1, 8, 11]. There is an opinion about the genetic mechanisms of calcium metabolism disorders in FD, identified with a certain locus of chromosome 14q [4]. Therapy for the disease is symptomatic or aimed at improving calcium-phosphorus metabolism.
Over 15 years, out of 45 thousand CT studies of the brain, we observed massive brain calcification in 22 cases (0.04%), and only 2 patients had clinical symptoms. We present these observations.
Patient 3., 39 years old, welder, upon admission to the neurological department of the 5th clinical hospital in Minsk, complained of general stiffness and slowness of movements. I was ill for 4 months when, for no apparent reason, I noticed a slowdown in movements in my left hand, then general stiffness, and my gait changed. He received undifferentiated treatment as an outpatient. Hospitalized due to progressive deterioration of his condition.
Previous illnesses include rare colds and mild traumatic brain injury (15 years ago). Denies similar illnesses in the family. Upon admission, the condition was satisfactory, low nutrition, blood pressure 120/80 mm Hg. Art. The thyroid gland is not enlarged, no somatic pathology was detected. Consciousness is clear, memory and criticism of one’s condition are reduced. Speech is monotonous and lacks modulation. The posture (the posture of the petitioner) is disturbed, the face is hypomimic, the arms are brought to the body (Fig. 17). Reflexes of oral automatism are expressed. The strength in the limbs is sufficient, muscle tone is increased according to the plastic type. Moderate oligo- and bradykinesia are noted. Tendon-periosteal reflexes are high, evoked from the expanded zones D=S, plantar and abdominal reflexes are of medium vivacity, there are no pathological foot signs. Coordination and sensitivity are not impaired. The gait is changed according to the microbasic type, there are no friendly movements of the arms.
During the examination: general clinical blood and urine tests without pathology. Blood electrolytes: potassium 4.4 mmol/l (normal 3.6-5.4 mmol/l), sodium 136 mmol/l (normal 130-150 mmol/l), calcium 2.0 mmol/l (normal 2, 0-2.75 mmol/l), phosphorus 1.0 mmol/l (normal 0.8-1.48 mmol/l). Ophthalmologist: visual acuity OD/OS = 0.9/0.7, not correctable, fundus without pathology. CT scan of the brain: massive symmetrical areas of calcification are identified subcortically in the frontal, temporal, occipital lobes of the cerebral hemispheres, basal ganglia, and cerebellar hemispheres. The basal cisterns, cerebral ventricles, and cortical grooves are expanded (Fig. 18). Radioisotope study of the thyroid gland: the gland is spherical, the isotope distribution is uniform.
Rice. 17. Patient 3., 39 years old, diagnosed with Farah disease: “petitioner” pose, arms brought to the body, face hypomimic
Rice. 18. CT scan of the brain of the same patient: massive symmetrical areas of calcification are identified subcortically in the frontal, temporal, occipital lobes of the cerebral hemispheres, basal ganglia, and cerebellar hemispheres
Treatment was carried out: madopar (625 mg/day), piracetam, vitamin E, a course of hyperbaric oxygenation. Against this background, the patient’s condition improved, and the severity of akinetic-rigid syndrome decreased. During follow-up for three years, no signs of disease progression were noted. The patient's children were examined: a daughter (15 years old), who had several epileptic seizures in early childhood and took anticonvulsants for a year. Currently, there are no complaints; examination revealed no neurological symptoms; CT scan of the brain shows no pathology. The son (12 years old) has no complaints; objective and CT examinations revealed no abnormalities.
The second patient G., 21 years old, a mechanic, was admitted with complaints of repeated tonic convulsions of the right half of the face and limbs lasting 10-15 s, provoked by a change in body position, minimal physical activity or sudden appeal to him. He was ill for 5 months, when after the mentioned provoking factors the above-described paroxysms began to appear occasionally. Subsequently, their frequency increased to 5-6 times a day. Since childhood, he has been observed in the clinic for congenital aortic heart disease and logoneurosis. At the age of 16 he was operated on due to congenital convergent strabismus. There is no heredity for this disease. Upon admission, the condition was satisfactory, elements of dysraphic status (tower skull, fused earlobes). Blood pressure 120/80 mm Hg. Art., pulse 64 beats/min, rhythmic. The thyroid gland is not enlarged. On auscultation, a systolic murmur is heard at the apex and at Botkin's point. No other somatic pathology was identified. Neurologically: conscious, adequate, memory is not impaired, speech with elements of logoneurosis. Cranial nerves without pathology. Strength and tone in the limbs are not changed, tendon-periosteal reflexes are of average vivacity, D=S. Coordination and sensitivity are not impaired. In the department, during the first 5 days, short-term (up to 10 s) fanciful violent movements in the right limbs were repeated without loss of consciousness, provoked by sudden sounds or physical activity.
Positive symptoms of Khvostek (convulsive contraction of the facial muscles during percussion in the area of the facial nerve trunk) and Trousseau (convulsive contraction of the hand muscles in the form of an “obstetrician’s hand” when squeezing the neurovascular bundle at shoulder level) were determined.
Examination: blood and urine tests without pathology. Blood electrolytes: potassium 3.9 mmol/l, sodium 138 mmol/l, calcium 1.9 mmol/l, phosphorus 2.0 mmol/l. Ophthalmologist: visual acuity OD/OS = 0.9/0.2, not correctable, fundus without pathology. EEG: moderate changes in the bioelectrical activity of the brain are recorded at a reduced amplitude level, no signs of epileptic activity were detected. CT scan of the brain: multiple symmetrical foci of calcification are detected in the cerebral hemispheres, basal ganglia, and cerebellum. Ultrasound of the thyroid gland: did not reveal any changes. Attacks of muscle spasms were stopped by the administration of a small dose of carbamazepine (100 mg/day) and did not recur subsequently.
Thus, in both presented cases, characteristic signs of FD were detected radiographically. Clinical manifestations of the disease varied significantly. The first patient had symptoms of parkinsonism and dementia. In the second, clinical manifestations of primary hypoparathyroidism prevailed against the background of perinatal pathology of the central nervous system. In both patients, positive results were obtained when symptomatic treatment was prescribed (levodopa-containing and anticonvulsants).
The classic triad for FD is typical neuropsychiatric symptoms, hypoparathyroidism and symmetrical calcification of the basal ganglia, but literature data indicate that incomplete forms of the disease are more common [10]. With the introduction of modern neuroimaging methods (especially brain CT) into everyday clinical practice, intravital diagnosis of FD has become easier, since these studies can detect signs of the disease even in the preclinical stage of the disease. Despite the use of modern diagnostic technologies, FD is extremely rare. According to various authors, radiological signs of FD are observed in 1-2% of all cases of brain CT [5, 10]. In FD, calcification occurs in all areas of the brain, but predominates in the basal ganglia region [5, 6, 12]. Calcium accumulations are found outside the blood vessels of the brain and have a characteristic ultrastructure. According to A. Guseo et al. [6], calcifications consist of thin filaments (140-400 microns).
Clinical manifestations of FD are even less common than radiological ones. Thus, N. Goldscheider et al. [5] performed a CT scan of the brain in 8000 patients and found calcification of the basal ganglia in 19 cases, but only 6 people had clinical symptoms of the disease. According to most authors, neurological disorders do not depend on the location and size of lesions [5, 9]. The most common neurological manifestations of FD include parkinsonism and gradually developing dementia, which a number of researchers explain by the extensive type of calcification and metabolic disorders of nervous tissue [2, 12].
Often in the clinical picture of FD there is a primary (usually autoimmune) or postoperative dysfunction of the parathyroid gland. In these cases, changes in the production of parathyroid hormone lead to a decrease in calcium levels and an increase in phosphorus in the blood [7, 10]. In FD, cases of pseudohypoparathyroidism have been described in pulmonary pathology, when the intracellular phosphorus content increases due to hyperventilation and hypocapnia [8, 11]. Similar mechanisms of development of brain hypoxia explain brain calcification in hypertension [1]. D. Geschwind et al. described a family case of diagnosis of FD with the phenomenon of genetic anticipation, in which the authors were for the first time able to identify the chromosomal locus of the disease, mapped to chromosome 14q [4].
Differential diagnosis of FD is carried out with parasitic lesions of the nervous system (toxoplasmosis, echinococcosis, cysticercosis). In these cases, epidemiological history and specific serological reactions in the blood and cerebrospinal fluid are of diagnostic value. Less commonly, FD is differentiated from Bourneville tuberous sclerosis, in which characteristic skin changes occur.
In the treatment of FD, symptomatic drugs are used. In the presence of symptoms of parkinsonism, it is preferable to use levodopa drugs (madopar, sinemet, nacom) rather than dopamine agonists, since in these cases replacement therapy to replenish dopamine becomes of great importance. As a pathogenetic treatment for FD, the administration of antioxidants, brain metabolites, and effects on the electrolyte composition of the blood is indicated.
Prognosis for Farah disease
Since this condition disrupts metabolism in the brain, and calcium salts have an irritating effect on brain tissue, Farah’s disease has very ambiguous prognosis. The disease progresses slowly, and calcium deposits increase with age. Of course, all this does not happen in one year. Typically, neurodegenerative diseases progress over several decades. The main problem is the lack of information on this condition, as well as the lack of specific treatment. Therefore, therapy is aimed at improving the patient’s quality of life. Another negative point is that the disease is poorly diagnosed in the early stages.
Diagnostics
The main diagnostic method that allows a neurologist to reliably determine the presence of foci of calcification in brain tissue is a CT scan of the brain. The intensity of the lesions on tomograms reflects the level of calcium concentration. MRI of the brain visualizes calcifications much worse, but allows one to evaluate concomitant degenerative processes. In order to confirm the idiopathic nature of the pathology, a number of additional examinations are carried out:
- Blood chemistry
. Blood electrolytes are determined: calcium, phosphorus, iron, sodium. The absence of significant deviations allows us to exclude general metabolic disorders in the body, leading to calcium deposition. - Determination of parathyroid hormone levels
. Normal levels of hormone concentration in the blood exclude the presence of hypoparathyroidism and pseudohypoparathyroidism as the most common causes of calcification. - Ultrasound of the thyroid and parathyroid glands
. In patients with Farah's disease, the echoscopic picture remains within normal limits, which excludes hormonal metabolic disorders associated with damage to these glands. - TCD of cerebral vessels
. Necessary for assessing cerebral hemodynamics and identifying chronic cerebral ischemia as the root cause of degenerative changes accompanied by calcification. - PCR studies
. Aimed at identifying toxoplasma, cytomegalovirus and other infectious agents that can cause inflammatory changes in brain tissue with the formation of calcifications.
The diagnosis of Farah's disease is valid after excluding the secondary nature of cerebral calcification, which is observed in endocrine (hypoparathyroidism, pseudohypoparathyroidism, hypothyroidism), vascular (atherosclerosis, vascular amyloidosis), infectious (rubella, cysticercosis, toxoplasmosis, cytomegaly) diseases. Differential diagnosis is also carried out with Hallervorden-Spatz disease and tuberous sclerosis.