Metasympathetic nervous system (MNS)
- part of the autonomic nervous system, a complex of microganglionic formations (intramural ganglia are ganglia located on the surface or in the thickness of organs) and the nerves connecting them, as well as individual neurons and their processes located in the walls of internal organs, which have their own motor activity. The main effector apparatuses of the walls of hollow visceral organs, which are regulated by the MHC, are: smooth muscle, secretory, absorptive and excretory epithelium, capillary network, local endocrine and immune formations. Characterized by a high degree of relative independence from the central nervous system. Has no nuclear structure.
From the point of view of organ affiliation, it is proposed to distinguish, respectively, the enterometasympathetic, cardiometasympathetic, urethrometasympathetic, vesiculometasympathetic nervous system [1]. The most studied is the metasympathetic system of the intestines and heart.
Criticism of the conditional identification of the metasympathetic nervous system
This is how Doctor of Medical Sciences, Prof. explains the reasons for the critical attitude in the scientific world to the hypothesis of the “metasympathetic nervous system”. Motavkin P. A.[2]:
The metasympathetic division of the autonomic nervous system includes intramural neurons of the digestive, respiratory systems, heart, bladder, and prostate gland. This department, according to some physiologists, has complete autonomy, that is, it is not dependent on the influence of central mechanisms. It functions on the basis of local reflexes, the basis of which is formed by the ANS’s own cells, not connected to central neurons. Complete autonomy of this department is possible if the presence of motor neurons not controlled by preganglionic fibers
. Currently, six types of cells, different in morphology and mediator specialty, have been identified in the enteric system. The possibility that among them there are local effector cells that are independent of central influences should not be denied.<…> In the meantime, the prevailing point of view relates intramural neurons to the parasympathetic division...
Cardiometasympathetic system
The metasympathetic autonomic nervous system, as mentioned, consists of several divisions. The ganglion system of the heart is already quite well studied, so we can look at how it works.
Protection of the heart occurs due to reflex cycles that have a “base” in the intramural ganglia.
Thanks to the work of G.I. Kositsky, we know about one very interesting reflex. Stretching of the right atrium always affects the functioning of the right ventricle. He works harder. The same thing happens in the left side of the heart.
When the aorta is stretched, the contractility of both ventricles reflexively decreases. These effects occur through the metasympathetic nervous system. The Goltz reflex occurs when, when struck in the abdomen, the heart may stop contracting for a while. The reaction is associated with the activation of the abdominal nerve, with its afferent part.
The heart rate also decreases under other influences. The Aschner-Dagini reflex is the reaction of the heart when pressure is applied to the eyes. Cardiac arrest also occurs when the vagus nerve is irritated. But with subsequent irritation of the nerve, this effect goes away.
Cardiac reflexes are designed to maintain blood filling of the arteries at a single constant level. The autonomy of the nervous intracardiac system proves the ability of the heart to survive after transplantation. Although all of the cardiac major nerves have been cut, the organ continues to contract.
Functions
Functions of the metasympathetic nervous system:
- transmission of central influences - due to the fact that sympathetic and parasympathetic fibers can contact the MNS and thereby correct its influence on control objects;
- integration, since the system has reflex arcs (afferent-intercalary-efferent neurons).
Internal organs communicate with each other via the MNS, bypassing the brain, and its role as a signal switch is performed by the ganglia. To overcome the natural barrier between the chest and abdominal cavities - the diaphragm - local reflex connections are helped by the celiac and vagus nerves, the processes of which reach the bronchi and vessels of the pulmonary circulation. The lungs and stomach can influence each other and the heart. Peripheral reflexes are not isolated from the central nervous system; under normal conditions, they interact with all parts of the regulatory apparatus, and if the connection with the periphery is disrupted, they can provide regulation of the vital activity of “their” organs[3].
Mediators of the autonomic nervous system
⇐ PreviousPage 19 of 37Next ⇒All neurons of the autonomic nervous system, according to the quality of the mediator released by their endings, are divided into cholinergic (acetylcholine) and adrenergic (norepinephrine, dopamine). The mediator of all preganglionic fibers, sympathetic and parasympathetic, is acetylcholine, which interacts with M- and N-cholinergic receptors of ganglion cells, causing their excitation. M-cholinergic receptors (muscarine-sensitive) lose sensitivity to acetylcholine under the influence of muscarine (a poison isolated from the fly agaric mushroom) and atropine. H-cholinergic receptors (nicotine-sensitive) - under the influence of nicotine and similar ganglion blockers (hexonium). In addition, in the autonomic ganglia the function of mediators or neuromodulators is performed by a number of other biologically active substances, for example, substance P, dopamine, etc.
The endings of all parasympathetic and sympathetic nerves that innervate the sweat glands and provide vasodilation of working muscles (vasodilators) are also cholinergic. All other postganglionic sympathetic neurons are adrenergic, which form synapses with α- and β-adrenergic receptors of the membranes of the organs they innervate.
Most organs contain both types of adrenergic receptors, which can cause different reactions, for example in blood vessels. The connection of the mediator with α-adrenergic receptors causes constriction of arterioles, and the connection with β-adrenergic receptors causes expansion. It is also possible for the organ to have identical reactions in the presence of both types of adrenergic receptors, as in the intestine, where, by acting on α- and β-adrenergic receptors, one can only cause inhibition of smooth muscles.
In other organs - the heart, the bronchi - there are only β-adrenergic receptors, upon interaction with which there is an increase in heart contractions and dilation of the bronchi.
In addition to acetylcholine and norepinephrine, other mediators (dopamine, serotonin) were found in the endings of the autonomic nerves, the effect of which is similar to the action of acetylcholine, but persists after blockade of cholinergic receptors (intestines, uterus).
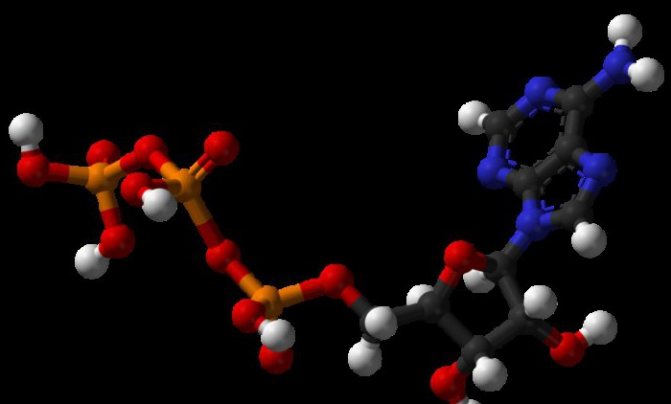
Mediators of the autonomic nervous system also include purine compounds - adenosine, inosine, adenosine triphosphoric acid. Neurons in whose endings these substances are released are called purinergic. Their excitation inhibits the activity of the smooth muscles of the stomach and intestines, and promotes relaxation of the sphincters of the gastrointestinal tract.
The role of a mediator of the autonomic nervous system in some cases can be played by histamine, which has a wide spectrum of action, as well as the inhibitory mediator GABA (gamma-aminobutyric acid), which is widespread in the synapses of the central nervous system, found in the stellate, inferior mesenteric, and celiac ganglia.
COMPARATIVE CHARACTERISTICS OF SOMATIC AND
AUTONOMIC NERVOUS SYSTEMS
| No. | Signs | Somatic | Vegetative |
| 1. | Source of development | · The ectoderm differentiates into spongioblasts (neuroglia) and neuroblasts (nerve cells). · Rapid evolution, due to the rapidly progressing apparatus of movement and sensory organs. | · From the neuroectoderm (common with the animal part of the source), as a result of migration and further differentiation, nuclei, nodes and fibers of the autonomic nervous system are formed. · Slow evolution, due to the less progressive development of plant life organs. |
| 2. | Functions | Characteristic only of animal organisms: · motor – voluntary contractions of skeletal muscles; · sensitive – the functions of the senses (vision, hearing, smell, taste, touch, gravity) and nonspecific sensitivity (temperature, pain, tactile), provide the body with the external environment. | Characteristic equally of animal and plant organisms: · neurosecretory; · adaptation-trophic. They ensure homeostasis, regulate metabolism, respiration, excretion, reproduction, and circulation of fluids in the body. |
| 3. | Innervation area | Limited area of distribution - striated muscles and sensory organs. | Widespread distribution in the body (internal organs, blood vessels, glands). |
| 4. | Principle of innervation | Segmental (principle of symmetry). | The focality of the output of vegetative fibers: mesencephalic, pontobulbar, thoracolumbar and sacral sections. |
| 5. | Regulation principle | Reflex, voluntary (controlled). | Reflexive, involuntary. |
| 6. | Characteristics of nerve fibers | Afferent and efferent, covered with a myelin sheath. | Afferent: myelinated and non-myelinated. Efferent: · preganglionic, myelinated; · postganglionic, unmyelinated. |
| 7. | Fiber diameter | 4-22 microns. | Afferent – 2-22 µm. Efferent: · preganglionic – 1.5-4.5 µm · postganglionic – 0.5-2.5 µm |
| 8. | Impulse conduction speed. | 12-120 m/s. | Afferent – 1-120 m/s. Efferent: · preganglionic – 1.5-20 m/s · postganglionic – 0.5-3 m/s |
| 9. | Centers | Spinal cord and brain. | Suprasegmental (integrative) Segmental (sympathetic and parasympathetic). |
| 10. | Nodes | Sensitive (cranial and spinal). | I order – paravertebrates, gangll. paravertebralia , sympathetic. II order – prevertebrates, gangll. prevertebralia , sympathetic. III yard - final, gangll. terminalia , parasympathetic. |
| 11. | Plexus | Cervical, shoulder, lumbosacral. | Primary (perivascular) Secondary (intraorgan) |
| 12. | Nerves | 12 pairs of cranial nerves; 31 pairs of spinal nerves. | Parasympathetic consisting of III, V, VII, IX, X pairs of cranial nerves. Organ, nn. splanchnici. Sympathetic as part of all spinal nerves |
| 13. | Reflex arc of the spinal cord | The simplest one is two-neuron. | The simplest one is three-neuron. |
| 14. | Localization of neurons in a 3-neuron reflex arc | 1st neuron – spinal ganglion; 2nd neuron – posterior horns of the spinal cord; 3rd neuron – anterior horns of the spinal cord. | 1st neuron – spinal ganglion; 2nd neuron – lateral horns of the spinal cord; The 3rd neuron is the autonomic ganglion. |
Sympathetic part of the autonomic nervous system
Carrying out the adaptive-trophic function of the body, the sympathetic nervous system is widespread, innervating almost all organs and tissues of the body.
As noted above, the central segmental section of the sympathetic part is localized in the lateral horns of the spinal cord at the level of C8, Th1-L2 and is represented by nuclei - nucl. intermediolaterales
. The axons of the neurons that form these nuclei are part of the anterior roots, then the trunk of the spinal nerves, and upon exiting the spinal canal they are separated, forming white connecting branches. These branches go to the sympathetic ganglia - paravertebral or prevertebral.
Sympathetic trunk
Paravertebral ganglia form the sympathetic trunk, truncus sympathicus
.
This is a paired formation consisting of a chain of 17-22 nerve nodes, ganglia trunci sympathici
, interconnected by internodal branches,
rami interganglionares
. The sympathetic trunk is located on the posterior wall of the body on both sides of the spinal column, extending from the base of the skull to the coccyx. Below the diaphragm, the sympathetic trunks gradually come closer together and at the level of the coccyx they unite in the unpaired coccygeal ganglion.
The sizes of the nodes vary: from microscopic to 10-12 mm in the lumbar region. The shape of the nodes is often polygonal. The sympathetic trunk is connected to the spinal nerves by connecting branches (white and gray), and to the internal organs, vessels and prevertebral nerve plexuses by visceral branches.
White connecting branches, rr. communicantes albi
, are present only in the thoracic and lumbar sections of the sympathetic trunk (C8-L2), and the gray connecting branches,
rr.
communicantes grisei , - along the entire length of the sympathetic trunk. The white and gray connecting branches, which are efferent, also include afferent fibers. These are the dendrites of neurons in the spinal ganglia, as well as the axons of type II Dogel neurons located in the vegetative ganglia. The visceral, or organ, branches of the sympathetic trunk extend to the internal organs and vessels and have names corresponding to them (cardiac, pulmonary branches, internal carotid nerve, etc.). these branches innervate organs not only on their own, but also on the opposite side due to transverse connections, which is especially pronounced in the abdominal cavity.
There are four sections in the sympathetic trunk : cervical, thoracic, lumbar, sacral . Each section usually contains fewer nodes than the corresponding segments of the spinal cord.
Rice. 20. Sympathetic part of the autonomic nervous system.
1 – truncus sympathicus; 2 – ganglion cervicothoracicum; 3 – ganglion cervicale medium; 4 – ganglion cervicale superius; 5 – a. carotis interna; 6 – plexus celiacus; 7 – plexus mesentericus superior; 8 – plexus mesentericus inferior.
Cervical region
Extends from the base of the skull to the neck of the first rib. It is represented by three nodes and internodal fibers connecting them. Preganglionic fibers pass to these nodes from the sympathetic nuclei of the C8-Th6-7 segments as part of the internodal branches of the thoracic sympathetic trunk.
Superior cervical ganglion, ganglion cervicale superius
,
- one of the largest nodes of the sympathetic trunk, 1.5-2 cm long, 0.5 cm wide, located in front of the transverse processes of the II-III cervical vertebrae, behind the internal carotid artery and medial to n.
vagus . Its shape is often spindle-shaped.
Middle cervical ganglion
,
- an unstable, small node, located anterior to the transverse process of the VI cervical vertebra at the intersection of a.
thyroidea inferior and the cervical sympathetic trunk (its old name is
ganglion thyroideum
). It has an oval or triangular shape.
Lower cervical ganglion, ganglion cervicale inferius
,
– variable in its topography, shape and size. It is located between the transverse process of the VII cervical vertebra and the head of the first rib. Length up to 2 cm, width 0.8-1 cm, spindle-shaped or polygonal in shape. This node often merges with the upper thoracic node, forming a large cervicothoracic, or stellate, node, ganglion cervicothoracicum s.
stellatum . The nodes of the cervical sympathetic trunk give off
connective and visceral branches .
The communicating branches are represented only by the internodal and gray communicating branches, since in the cervical segments of the spinal cord (except C8) there are no sympathetic nuclei and, as a consequence, white communicating branches. The gray communicating rami consists of postganglionic fibers of the neurons of the cervical sympathetic ganglia and is part of all cervical spinal nerves.
The visceral branches are formed mainly by postganglionic fibers, which are processes of neurons of the cervical sympathetic ganglia, as well as preganglionic fibers that transit through the cervical ganglia and end at the prevertebral (intermediate) ganglia. Visceral branches can be divided into two groups:
visceral branches to vessels;
visceral branches to organs.
The first group includes branches heading to the vessels of the head and neck, around which they form plexuses and bear the same names:
internal carotid plexus, plexus caroticus internus
, from which the deep petrosal nerve,
n.
petrosus profundus , and orbital plexus,
plexus ophtalmicus
.
The continuation of the internal carotid plexus is the cavernous plexus, plexus cavernosus
;
external carotid plexus, plexus caroticus externus
, spreads along the branches of the artery of the same name;
jugular plexus, plexus jugularis
, rises to the sensitive nodes of the IX and X pairs of cranial nerves and the trunk of the XII pair, due to which the branches of the listed pairs of cranial nerves also include sympathetic fibers;
subclavian plexus, plexus subclavius
, continues to the vessels of the upper limb;
vertebral plexus, plexus vertebralis.
The second group of visceral branches of the cervical spine includes branches that follow the organs, receiving their name:
cervical cardiac nerves, nn. cardiaci cervicales superior, medius et inferior
, enter the deep cardiac plexus;
Hypopharyngeal nerves, nn. laryngopharyngei
, form the pharyngeal plexus together with the branches of the glossopharyngeal and vagus nerves.
Thoracic region
The thoracic section of the sympathetic trunk is represented by a chain of 9-12 nodes, ganglia thoracica
, located in front of the heads of the ribs, behind the intrathoracic fascia and parietal pleura and the internodal branches connecting them.
The nodes are mostly triangular in shape, 0.3-0.5 cm in size. White connecting branches (preganglionic fibers) are connected to all nodes of the thoracic part.
Gray connecting and visceral depart from the nodes of the thoracic region . The gray connecting branches are directed and included in the intercostal nerves. Visceral branches go to the organs:
üthoracic cardiac branches, rr. cardiaci thoracici
, extend from the five upper nodes and participate in the formation of the superficial cardiac plexus;
Pulmonary branches, rr. pulmonales
, form the pulmonary plexus;
ümediastinal branches, rr. mediastinales
, participate in the formation of plexuses along the vessels of the mediastinum (gyzygos and semi-gyzygos veins, thoracic lymphatic duct), and also form the thoracic aortic plexus,
plexus aorticus thoracicus
, and esophageal plexus,
plexus esophageus
.
The visceral branches of the sympathetic trunk, following to the organs and vessels of the abdominal cavity, form the greater and lesser splanchnic nerves.
Greater splanchnic nerve, n. splanchnicus major, is formed by branches extending from the V-IX thoracic nodes, and consisting mainly of preganglionic fibers that passed in transit (without interruption) through these nodes. Having merged into one common trunk at the level of the IX thoracic vertebra, the nerve penetrates the abdominal cavity between the muscle bundles of the diaphragm and becomes part of the celiac plexus, ending in its nodes ( gangl. coeliaca, gangl. aororenalia, gangl. mesentericum superior
).
Lesser splanchnic nerve, n. splanchnicus minor , is formed by the visceral branches of the X-XI thoracic nodes and also contains predominantly preganglionic fibers. This nerve, penetrating into the abdominal cavity, sends some of its fibers to the nodes of the celiac plexus, and some to the aorto-renal nodes.
Lower splanchnic nerve, n. splanchnicus imus, non-permanent, starts from the XII thoracic node and ends in the gangl. aortorenalia
renal plexus.
Lumbar
The lumbar sympathetic trunk is represented by 3-5 nodes, ganglia lumbalia
, and internodal branches connecting them. The nodes are spindle-shaped, measuring 0.6 cm or more. They are located on the anterolateral surface of the lumbar vertebral bodies. The nodes of the right and left sympathetic trunks are connected by transverse connecting branches. White connecting branches approach the first two lumbar nodes.
From each lumbar node depart:
ü gray connecting branches , rr. communicantes grisei
, heading to the lumbar spinal nerves;
ü lumbar splanchnic nerves , nn. splanchnici lumbales
, which are directed to the prevertebral plexuses of the abdominal cavity and choroid plexuses - splenic, hepatic, gastric, renal, etc.
Sacral (pelvic) section
Represented, as a rule, by four nodes, ganglia sacralia
, fusiform, 0.5 cm in size. The nodes are located on the pelvic surface of the sacrum medially from the pelvic openings and are connected by longitudinal and transverse internodal branches.
Heading downwards, both trunks come closer and at the level of the first coccygeal vertebra they merge in the unpaired node, ganglion impar
. From the sacral nodes they depart:
ü gray connecting branches to the sacral and coccygeal spinal nerves;
ü sacral organ nerves , nn. splanchnici sacrales
involved in the formation of the hypogastric plexuses.
Prevertebral plexuses
The prevertebral section of the sympathetic nervous system is represented by plexuses located on the aorta and its branches. Anatomically, this section of the nervous system resembles a network with cells of various sizes and shapes, formed by pre- and postganglionic fibers, as well as autonomic ganglia (II order). The bodies of the second neurons of the efferent part of the autonomic reflex arc are located in the vegetative nodes, the axons of which form the visceral nerves. The prevertebral plexuses also include afferent and parasympathetic fibers. the prevertebral plexuses of the neck, thoracic, abdominal and pelvic cavities are distinguished .
The nerve plexuses of the neck are formed by branches of the cervical and first and second thoracic sympathetic nodes. The plexus also includes afferent and parasympathetic fibers. An example of such a plexus is the pharyngeal plexus, plexus pharyngeus.
, located in the wall of the ascending pharyngeal artery,
a.
pharyngea ascendens , and its branches. The plexus includes postganglionic sympathetic fibers emanating from the cervical and superior thoracic ganglia of the sympathetic trunk, preganglionic parasympathetic and sensory fibers of the vagus and glossopharyngeal nerves.
In the thoracic cavity, the prevertebral plexuses are localized in the region of the heart, the hilum of the lung, along the descending aorta and around the esophagus.
The cardiac plexuses, plexus cardiacus, are formed by sympathetic (from the cervical and superior thoracic ganglia), parasympathetic (vagus nerve fibers) and afferent nerve fibers. There are superficial (between the aortic arch and the bifurcation of the pulmonary trunk) and deep (between the aortic arch and the tracheal bifurcation) cardiac plexuses. A large number of nerve cells and nodules are detected in the cardiac plexuses. The branches of the cardiac plexuses accompany the vessels of the heart to their final branches and are named accordingly.
The pulmonary plexus, plexus pulmonalis, is located in the region of the roots of the lungs and is formed by the mediastinal branches from the five upper thoracic sympathetic nodes and the branches of n. vagus
. From the pulmonary plexus, the nerves spread along the vessels and bronchi into lobes, segments and lobules. Along the plexus, numerous intraorgan nerve nodules are found. The aortic and esophageal branches depart from the thoracic nodes of the sympathetic trunk, forming plexuses of the same name.
Prevertebral plexuses of the abdominal and pelvic cavities. located in front of the abdominal aorta ( plexus aorticus abdominalis
) and around its branches, extending from the diaphragm to the floor of the pelvic cavity.
The largest part of the abdominal aortic plexus is the celiac, or solar, plexus , plexus coeliacus s.
plexus solaris .
This plexus is called the abdominal medulla. it is located in the form of a horseshoe around the celiac trunk. It consists of two celiac ganglia, ganglia coeliaca, s.
ganglia solaria, s. ganglia semilunaria , semilunar in shape, located on the sides of the celiac trunk, two aortorenal nodes,
ganglia aortorenalia
, at the origin of the renal arteries and an unpaired superior mesenteric node,
ganglion mesentericum superior
, lying at the beginning of the artery of the same name. Connecting branches (commissures) are found between the symmetrical nodes.
The large and small splanchnic nerves, visceral branches of the upper lumbar sympathetic ganglia, fibers of the posterior vagus nerve, as well as sensory (afferent) fibers of the right phrenic nerve approach the celiac plexus.
Branches extend from the celiac nodes, forming the choroid plexuses of the same name: hepatic, plexus hepaticus,
splenic,
plexus lienalis,
gastric,
plexus gastrici
, pancreas,
plexus pancreaticus
, adrenal,
plexus suprarenales
, diaphragmatic,
plexus phrenicus.
The choroid plexuses include sympathetic postganglionic, parasympathetic preganglionic and afferent fibers. The exception is the fibers innervating the adrenal medulla. They consist of sympathetic preganglionic fibers, and the role of ganglia is performed by cerebral endocrinocytes, which have a common origin with the sympathetic nervous system.
Branches also depart from the celiac and aortorenal nodes, forming the paired renal plexus, plexus renalis,
passing into the ureteric,
plexus uretericus
, testicular,
plexus testicularis
, in men and ovarian,
plexus ovaricus
, in women plexus.
Branches depart from the superior mesenteric node, forming the superior mesenteric plexus, plexus mesentericus superior
, which continues along the course of the artery of the same name and its branches, reaching the thin, blind, ascending and right half of the transverse colon.
At the origin of the inferior mesenteric artery there is the inferior mesenteric node, ganglion mesentericum inferior
, the branches of which form the inferior mesenteric plexus,
plexus mesentericus inferior
. The branches of the celiac and superior mesenteric plexus also take part in the formation of the inferior mesenteric plexus, which enter it from the intermesenteric plexus (part of the abdominal aortic plexus between the superior and inferior mesenteric arteries). It spreads along the artery of the same name and its branches and reaches the left half of the transverse, descending, sigmoid colon and upper part of the rectum. The final sections of these plexuses form in the walls of hollow organs, according to their layers, submucosal, intermuscular and subserosal plexuses.
The abdominal aortic plexus continues along the course of the iliac arteries into the paired iliac plexus, plexus iliacus
, as well as into the unpaired superior hypogastric plexus,
plexus hypogastricus superior
, which is located below the aortic bifurcation on the bodies of the lower lumbar vertebrae.
This plexus has the appearance of a nerve fiber plate, to which nerve fibers from the ganglia of the lumbar and sacral sections of the sympathetic trunk approach. At the level of the promontory, the superior hypogastric plexus divides into two hypogastric nerves, nn.
hypogastrici dexter et sinister , which descend behind the peritoneum into the small pelvis.
The hypogastric nerves give rise to the paired pelvic, plexus pelvinus,
or lower hypogastric,
plexus hypogastricus inferior
, plexus.
This is one of the largest autonomic plexuses, in the formation of which, in addition to sympathetic elements, parasympathetic splanchnic nerves and afferent fibers take part. The plexus looks like plates located on both sides of the rectum. The nodes of the inferior hypogastric plexus have different shapes and sizes. From them begin secondary plexuses, the names of which correspond to the pelvic organs innervated by them: middle and lower rectal, plexus rectalis medius et inferior
, vesical,
plexus vesicalis,
vas deferens,
plexus deferentialis,
and prostate,
plexus prostaticus
, in men, utero-vaginal,
plexus uterovaginalis,
in women.
To summarize the above, we once again emphasize that the prevertebral plexuses are mixed: both efferent (sympathetic and parasympathetic) and afferent nerve fibers participate in their formation. Sympathetic fibers are pre- and postganglionic, parasympathetic fibers are preganglionic. All preganglionic fibers are covered with a myelin sheath, while postganglionic fibers are unmyelinated. In addition to nerve fibers, the plexus includes sympathetic ganglia of the second order. They are approached by preganglionic fibers that have transited through the truncus sympathicus
, and end on the bodies of the neurons of these ganglia. Postganglionic fibers depart from the ganglia and go to the innervated substrate.
⇐ Previous19Next ⇒
Microstructure and functional organization
The activity of the MNS is based on a functional module: a cluster of neurons connected in a special way, where oscillatory cells are distinguished, such as sensory neurons, tonic neurons, motor neurons, interneurons. The oscillator cell is the key cell of the module. It is excited spontaneously in a certain rhythm, transmitting action potentials through interneurons to the motor neuron, the axon of which is in contact with the muscle cell. The more active the oscillator cell, the more pronounced the inhibition of the motor neuron becomes. The oscillator-motoneuron system is modulated by:
- afferent neurons acting on the motor neuron through activation through the cholinergic synapse or at its termination (axo-axonal inhibition), removing the inhibitory effect on the muscle cell;
- parasympathetic and sympathetic postganglionic fibers, by influencing interneurons.
Oscillatory cells are extremely stable, and their function does not change under the action of neurotransmitters or ganglion blockers. Through an interneuron, an impulse from an oscillator cell triggers slave cells, which, according to the structure of their connections, represent sequentially organized chains. The sensory elements included in the neural ensemble activate special tonic neurons, causing the appearance of a prolonged discharge in them. In turn, tonic neurons form excitatory or inhibitory synaptic input to slave cells. Activation of a tonic neuron depends on the nature of the connection and can create either supportive excitation or, conversely, inhibition, which determines the direction of the responses of smooth muscles, epithelial cells, endocrine and other elements.
Enterometasympathetic system
The enteric nervous system is a unique mechanism where thousands of neurons are completely coordinated with each other. This mechanism, created by nature, is rightfully considered the second human brain. Because even if the vagus nerve, which is connected to the brain, is damaged, the system continues to perform all its functions, namely: digesting food and absorbing nutrients.
But it turns out that the digestive tract is not only responsible for the digestion of food, but, according to the latest data, also for the emotional background of a person. It has been established that the intestines produce 50% of dopamine, the hormone of joy, and about 80% of serotonin. And this is even more than is produced in the brain. Therefore, the intestines can safely be called the emotional brain.
In the enteric autonomic metasympathetic system, several types of neurons are distinguished:
- primary sensory afferents;
- ascending and descending interneurons;
- motor neurons.
Motor neurons, in turn, are divided into moving muscles, excitatory and inhibitory.
System value
The metasympathetic nervous system ensures the transmission of excitation from the extraorgan nervous system to the organ tissue and is an intermediary between the sympathetic and parasympathetic nervous systems and organ tissue. The metasympathetic nervous system regulates organ blood flow and is also directly related to the organization of regulatory influences on such an important function as membrane digestion.
Due to the presence of all components of reflex arcs in the metasympathetic nervous system, internal organs can work without the participation of the central nervous system [4].
Mediators MNS
Neurotransmitters are substances that help transmit impulses from one neuron to another. The mediators of the metasympathetic nervous system are as follows:
- histamine;
- serotonin;
- adenosine triphosphoric acid;
- acetylcholine;
- somatostanin;
- catecholamines.
In total, about 20 mediators and modulators in the neural network were discovered in laboratory conditions. A mediator such as acetylcholine, which belongs to the group of catecholamines, is a mediator of the sympathetic system, that is, it helps transmit the excitation signal. An excess of catecholamines in the body leads to overexcitation of the central nervous system. Heart failure often begins due to constant stress and releases of norepinephrine. Therefore, the body needs a restorative parasympathetic system.
Mediators such as pituitary peptide and ATP are designed to transmit the impulse of relaxation and recovery. Parasympathetic centers are located in the autonomic nuclei of the cranial nerves.
Notes
- Human physiology (textbook for medical universities) / N. A. Agadzhanyan, L. Z. Tel, V. I. Tsirkin, S. A. Chesnokova; edited by acad. RAMS N.A. Agadzhanyan and prof. N. A. Tsirkina. — Moscow: Medical book; N. Novgorod: Publishing house. NGMA, 2003. - P. 63.
- Motavkin P. A.
Course of lectures on histology. - "Medicine of the Far East", 2007. - P. 168. - ISBN 978-5-98301-017-8. - Bypassing the brain // Science and life: magazine. - M.: "Pravda", 1990. - No. 1. - P. 22.
- So, to study the MHC and indirectly prove the presence of internal arches, an isolated heart was taken. When an air balloon was inserted into the right atrium, distension of the atrium led to an increase in heart rate. Then, the inner surface of the heart was treated with an anesthetic and the experiment was repeated - the work of the heart did not change. This indicates the presence of reflex arcs inside the heart.
Central department
This part of the autonomic nervous system represents various structures of the brain. It turns out that it is scattered throughout the entire brain. In the central section, segmental and suprasegmental structures are distinguished. All formations belonging to the suprasegmental department are united under the name hypothalamic-limbic-reticular complex.
Hypothalamus
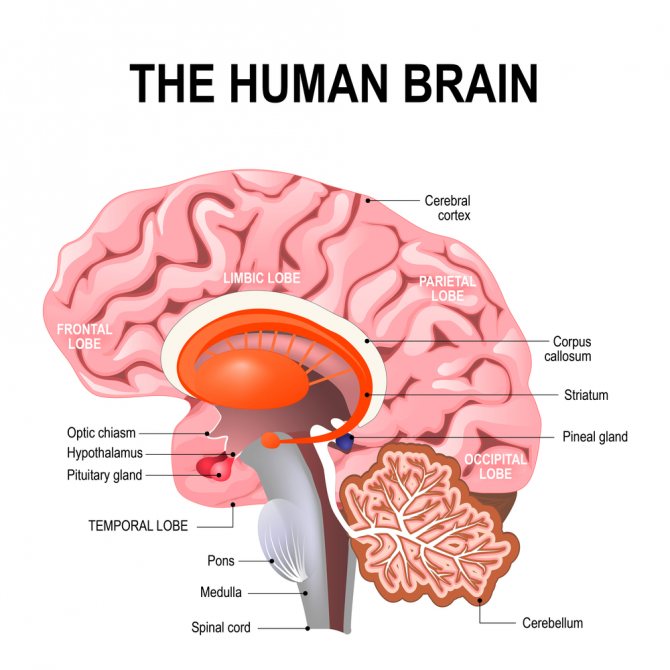
The hypothalamus is a structure of the brain located in the lower part, at the base. This cannot be said to be an area with clear anatomical boundaries. The hypothalamus smoothly passes into the brain tissue of other parts of the brain.
In general, the hypothalamus consists of a cluster of groups of nerve cells, nuclei. A total of 32 pairs of nuclei were studied. Nerve impulses are formed in the hypothalamus, which reach other brain structures through various pathways. These impulses control blood circulation, breathing, and digestion. The hypothalamus contains centers for regulating water-salt metabolism, body temperature, sweating, hunger and satiety, emotions, and sexual desire.
In addition to nerve impulses, substances with a hormone-like structure are formed in the hypothalamus: releasing factors. With the help of these substances, the activity of the mammary glands (lactation), adrenal glands, gonads, uterus, thyroid gland, growth, fat breakdown, and the degree of skin color (pigmentation) is regulated. All this is possible thanks to the close connection of the hypothalamus with the pituitary gland, the main endocrine organ of the human body.
Thus, the hypothalamus is functionally connected with all parts of the nervous and endocrine systems.
Conventionally, two zones are distinguished in the hypothalamus: trophotropic and ergotropic. The activity of the trophotropic zone is aimed at maintaining the constancy of the internal environment. It is associated with a period of rest, supports the processes of synthesis and utilization of metabolic products. It exerts its main influences through the parasympathetic division of the autonomic nervous system. Stimulation of this area of the hypothalamus is accompanied by increased sweating, salivation, slowing of heart rate, decreased blood pressure, vasodilation, and increased intestinal motility. The trophotropic zone is located in the anterior parts of the hypothalamus. The ergotropic zone is responsible for the body’s adaptability to changing conditions, ensures adaptation and is realized through the sympathetic division of the autonomic nervous system. At the same time, blood pressure increases, heartbeat and breathing accelerate, pupils dilate, blood sugar increases, intestinal motility decreases, and urination and bowel movements are inhibited. The ergotropic zone occupies the posterior parts of the hypothalamus.
Limbic system
This structure includes part of the temporal lobe cortex, hippocampus, amygdala, olfactory bulb, olfactory tract, olfactory tubercle, reticular formation, cingulate gyrus, fornix, and papillary bodies. The limbic system is involved in the formation of emotions, memory, thinking, ensures eating and sexual behavior, and regulates the sleep-wake cycle.
To realize all these influences, the participation of many nerve cells is necessary. The functioning system is very complex. In order for a certain model of human behavior to be formed, it is necessary to integrate many sensations from the periphery, transmitting excitation simultaneously to various structures of the brain, as if circulating nerve impulses. For example, in order for a child to remember the names of the seasons, repeated activation of structures such as the hippocampus, fornix, and papillary bodies is necessary.
Reticular formation
This part of the autonomic nervous system is called the reticular system because, like a network, it interweaves all the structures of the brain. This diffuse location allows it to participate in the regulation of all processes in the body. The reticular formation keeps the cerebral cortex in good shape, in constant readiness. This ensures instant activation of the desired areas of the cerebral cortex. This is especially important for the processes of perception, memory, attention and learning.
Individual structures of the reticular formation are responsible for specific functions in the body. For example, there is a respiratory center, which is located in the medulla oblongata. If it is affected for any reason, then independent breathing becomes impossible. By analogy, there are centers of cardiac activity, swallowing, vomiting, coughing, and so on. The functioning of the reticular formation is also based on the presence of numerous connections between nerve cells.
In general, all structures of the central part of the autonomic nervous system are interconnected through multineuron connections. Only their coordinated activity allows the vital functions of the autonomic nervous system to be realized.
Segmental structures
This part of the central part of the visceral nervous system has a clear division into sympathetic and parasympathetic structures. Sympathetic structures are located in the thoracolumbar spinal cord, and parasympathetic structures are located in the brain and sacral spinal cord.
Sympathetic department
Sympathetic centers are localized in the lateral horns in the following segments of the spinal cord: C8, all thoracic (12), L1, L2. Neurons in this area are involved in the innervation of smooth muscles of internal organs, internal muscles of the eye (regulation of pupil size), glands (lacrimal, salivary, sweat, bronchial, digestive), blood and lymphatic vessels.
Parasympathetic Division
Contains the following structures in the brain:
- accessory nucleus of the oculomotor nerve (nucleus of Yakubovich and Perlia): control of pupil size;
- lacrimal nucleus: accordingly, regulates tear secretion;
- superior and inferior salivary nuclei: provide saliva production;
- dorsal nucleus of the vagus nerve: provides parasympathetic influences on internal organs (bronchi, heart, stomach, intestines, liver, pancreas).
The sacral section is represented by neurons of the lateral horns of segments S2-S4: they regulate urination and defecation, blood flow to the vessels of the genital organs.
I Manifestation of activity ans.
The result of changes in ANS activity may be:
1) visceroreflexes (motor, secretory effects and their transport and metabolic support);
2) autonomic components of behavioral reactions (excitation of the sympathoadrenal system and endocrine glands);
3) level of mental activity (together with the reticular formation through neuropeptides);
4) level of physical activity (together with the reticular formation, sympathoadrenal system, endocrine glands);