Structure
The pyramidal system consists of a pyramidal tract formed by corticonuclear and corticospinal fibers. They are axons of neurons in the inner cortical layer of the telencephalon. They are localized in the precentral ridge (gyrus) and in the cortex of the parietal and frontal lobes. The primary motor field is located in the precentral crest along with pyramidal motor neurons, which are capable of controlling skeletal muscles as a whole (groups) or individually (1 muscle). Nerve cells that excite the lingual, pharyngeal and head muscles are localized in the lower parts of the ridge. Higher up, in the middle section, is the muscular system of the upper limbs and torso. The uppermost section provides nerve fibers to the muscle groups of the lower extremities.
Beginning of the pyramidal path (Kora)
The pyramidal system is the basis for the implementation of voluntary movements, starting in the 5th layer of the cerebral cortex, in the Betz motor cells.
The pyramidal tract is formed by myelin fibers passing through the white matter of the cerebral hemisphere and heading to the internal capsule. The knee of the capsule is formed by corticonuclear fibers, and the posterior limb of the internal capsule is partially formed by corticospinal fibers.
Pyramid Path
The fibers of the pyramidal tract first go to the basal part of the brain and then to the pontine region. They go through the front first. Then, passing through the brain stem, the corticonuclear fibers cross (transition to the opposite side) to the efferent nuclei of the oculomotor (III pair), trochlear (IV), trigeminal (V), abducens (VI), glossopharyngeal (IX), vagus ( X), accessory (XI) and hypoglossal (XII) nerves. The exception is the facial nerve (VII pair). Nerve fibers make the transition to the opposite side at the level of the nucleus, in the upper third. Partial fibers of the pyramidal tract from the brain stem are directed to the cerebellum.
Transition to the spinal cord
In the region of the medulla oblongata, the pyramidal tract passes through the pyramidal cells. At the junction of the pyramids and the spinal cord, the nerve bundles intersect. This cross divides the fibers into 2 unequal parts.
Division of the tract into the corticonuclear and corticospinal pyramidal tracts
80% of the nerve fibers go to the opposite side, forming the pyramidal lateral corticospinal tract in the lateral cord of the spinal cord. Fibers that do not cross into the anterior cord of the spinal cord, forming in it the anterior corticospinal tract. In the area of the white commissure, the fibers intersect. Many nerve fibers of the pyramidal tract terminate on interneurons of the anterior horns. They give rise to the development of the efferent components of the spinal nerves.
Localization (area of segments) Number of ending nerve fibers (cervical 50, thoracic 25%, lumbar 25%)
At the level of thoracic segments 3-5, the anterior corticospinal tract ends. Due to the crossing of nerve bundles in the pyramidal system, the left hemisphere of the brain is responsible for the innervation of the right half of the human body, and the right hemisphere is responsible for the innervation of the left half of the human body.
The corticonuclear pathway is associated with almost all nuclei of the cranial nerve. The exceptions are the purely sensory nerves olfactory, optic and vestibulocochlear nerves. Divided bundles of fibers also pass through the internal capsule in the white matter. Having reached the cranial nerve, the impulse is sent through separate bundles to the skeletal muscles. The corticonuclear tract controls facial expressions and swallowing muscles, while the corticospinal tract controls body and leg movements.
The pyramidal system is inextricably linked with the extrapyramidal system. They differ from each other in composition and functions.
The main differences of the extrapyramidal system are:
- it includes the basal ganglia, substantia nigra, red nucleus and other structures.
- performing complex unconscious motor acts: chewing food, playing sports (running);
- ensuring facial expressions;
- articulation of speech;
- ensuring muscle tone and its redirection during movements (posing and changing positions).
Pyramid Path
Motor
or
the pyramidal tract
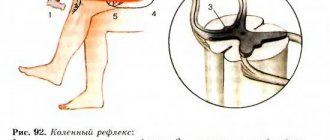
is two-neuron. The diagram of the pyramid paths is perfectly presented in the figure above and does not require explanation.
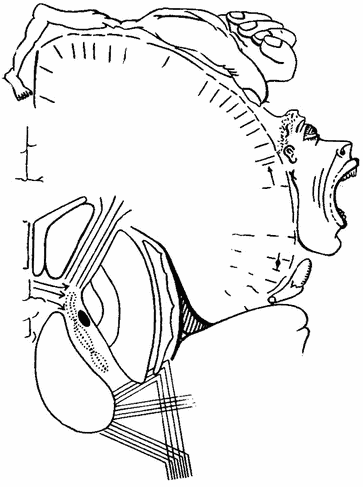
It is worth noting that within the brain stem, fibers extend from the motor tracts to the reticular formation, then to the motor nuclei of the cranial nerves - corticonuclear fibers
(fibrae corticonucleares), the course of which is shown in the diagram below.
Diagram of the course of the corticonuclear fibers of the pyramidal tract
Separately, it is worth saying that the ventral root connects with the dorsal root, forming a mixed spinal nerve. Subsequently, the spinal nerves form plexuses, and peripheral nerves emerge from the plexuses. Each peripheral nerve contains fibers from several adjacent segments of the spinal cord and innervates specific areas. The peripheral motor neuron is connected to the muscles of only its own side, while the central one, in most cases, is connected to the muscles of the opposite side.
Pathologies caused by damage to the pyramidal tract
Depending on the location of the pathological process, various clinical conditions caused by disruption of the pyramidal tract are identified.
Pyramidal insufficiency is a violation of the conduction and transmission of nerve signals at the level of the medulla oblongata in the area where the pyramids are located.
Children under 12 months of age and adults who have heart pathologies and malignant neoplasms most often suffer.
The causes of development in adults can be: immuno-inflammatory processes, hemodynamic disorders in the vessels of the brain, closed and open skull injuries, excess cerebrospinal fluid, which provokes the development of hydrocephalus, etc.
The causes of damage to the pyramidal tract in childhood are:
- Developmental abnormalities of the brain and spinal cord;
- Birth injuries in newborns;
- Hereditary (congenital) pathologies of the central nervous system;
- Hypoxia (with a decrease in atmospheric pressure)
- Traumatic brain injuries;
- Infectious and inflammatory processes (meningitis, encephalitis);
- Deficiency of micro- and macroelements;
- Cervical spine injuries.
Hereditary pathologies caused by gene mutations include some syndromes:
- With. Cobb (manifested by weakening movements of the arms and legs).
- With. Bonnet-Dechant-Blanc (manifested by visual impairment, in the form of protrusion of the eyes, double vision of objects and asymmetry of the palpebral fissures).
- v. Shtrumpel (weakening of the tone of the lower extremities, convulsive syndrome occurs).
The clinical picture in children under 2 months is not worrying. The reason for this is the congenital high tone of muscle tissue.
Children over 2 months: restless, constantly crying, cannot hold objects, reduced mental abilities, do not speak (starting from 3 months, children must make sounds (aha, etc.), in case of pyramidal insufficiency they only moo). By 6-8 months, children should crawl and rise to their feet, but with this pathology this is not possible. They are unable to use their fingers correctly (the grasping reflex is impaired). During sleep, you may notice how children's arms, legs and chin twitch.
In children older than one year, their gait changes, they walk on their toes, bend their legs, and as a result, clubfoot develops.
In adults, pyramidal insufficiency manifests itself in the form of increased skeletal muscle tone and a persistent increase in blood pressure. Sometimes convulsive and spastic syndromes occur. Due to the limitation of physical activity, because with hypertonicity, performing any physical exercise causes pain, excess body weight appears. When the process is neglected, a decrease in libido may occur.
Motor neurons of the pyramidal tract
Morphologically and functionally, three types of cells of the anterior horns - motor neurons (motoneurons) are distinguished:
- α-large,
- α-small,
- γ cells.
α-Motoneurons
α-Large
motor neurons carry out rapid physical movements, ending in white muscles;
α-small
motor neurons have tonic actions, terminating in red, slow-twitch muscles (see figure).
γ-Motoneurons
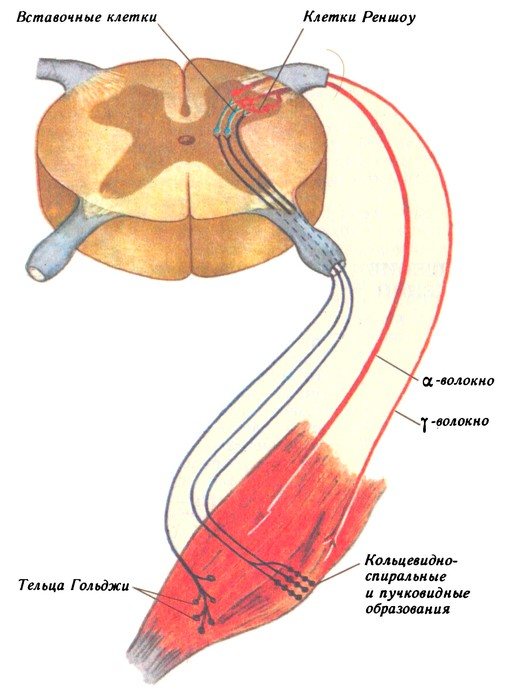
Of particular interest are γ-motoneurons
.
These cells do not carry out direct motor acts and therefore their designation as motor neurons is relative. Their efferent fibers approach a special type of proprioceptors embedded in the thickness of the muscle - “ muscle spindles
”, or
ring-spiral formations
.
From these receptors, impulses travel along afferent fibers through the dorsal roots, approach small α-motoneurons ( intercalary cells
,
Renshaw cells
), through them influencing the tonic state of the muscle. So, in addition to the central control carried out through the pyramidal and retinospinal tracts, peripheral control is also carried out, which was proven by the discovery of γ-motoneurons.
The descending pathways of the brain and spinal cord conduct impulses from the cerebral cortex, cerebellum, subcortical and brain stem centers to the underlying motor nuclei of the brain stem and spinal cord.
The highest motor center in humans is the cerebral cortex. It controls the motor neurons of the brain stem and spinal cord in two ways: directly through the corticonuclear, anterior and lateral corticospinal (pyramidal) tracts, or indirectly through underlying motor centers. In the latter case, the role of the cortex is reduced to starting, maintaining or stopping the execution of motor programs stored in these centers. Descending paths are divided into two groups:
- Pyramid system
ensures the execution of precise, purposeful conscious movements, adjusts breathing, ensuring the pronunciation of words. It includes the corticonuclear, anterior and lateral corticospinal (pyramidal) tracts.
Corticonuclear pathway
begins in the lower third of the precentral gyrus of the cerebrum. Here pyramidal cells (1 neuron) are located, the axons of which pass through the knee of the internal capsule into the brain stem and are directed in its basal part down to the motor nuclei of the cranial nerves of the opposite side (III–VII, IX–XII). The bodies of the second neurons of this system, which are analogues of the motor neurons of the anterior horns of the spinal cord, are located here. Their axons go as part of the cranial nerves to the innervated muscles of the head and neck.
Anterior and lateral corticospinal
(pyramidal) tracts conduct motor impulses from pyramidal cells located in the upper two-thirds of the precentral gyrus to the muscles of the trunk and limbs of the opposite side.
The axons of the first neurons of these pathways go together as part of the corona radiata, pass through the posterior leg of the internal capsule into the brain stem, where they are located ventrally. In the medulla oblongata they form pyramidal elevations (pyramids); and from this level these paths diverge. The fibers of the anterior pyramidal tract descend along the ipsilateral side in the anterior cord, forming the corresponding tract of the spinal cord (see Fig. 23), and then at the level of their segment they pass to the opposite side and end on the motor neurons of the anterior horns of the spinal cord (the second neuron of the system). The fibers of the lateral pyramidal tract, in contrast to the anterior one, pass to the opposite side at the level of the medulla oblongata, forming the decussation of the pyramids. Then they go in the back of the lateral cord (see Fig. 23) to “their” segment and end on the motor neurons of the anterior horns of the spinal cord (the second neuron of the system).
- Extrapyramidal system
carries out involuntary regulation and coordination of movements, regulation of muscle tone, maintaining posture, organizing motor manifestations of emotions. Ensures smooth movements and establishes the starting position for their execution.
The extrapyramidal system includes:
Corticothalamic tract,
conducting motor impulses from the cortex to the motor nuclei of the thalamus.
Radiance of the striatum
- a group of fibers connecting these subcortical centers with the cerebral cortex and thalamus.
Cortico-red nuclear tract,
conducts impulses from the cerebral cortex to the red nucleus, which is the motor center of the midbrain.
Red nuclear spinal tract
(Fig. 58) conducts motor impulses from the red nucleus to the motor neurons of the anterior horns on the opposite side (for more details, see Section 5.3.2.).
Tectospinal tract
. Its passage in general terms is similar to the previous path, with the difference that it begins not in the red nuclei, in the nuclei of the roof of the midbrain. The first neurons of this system are located in the tubercles of the quadrigeminal midbrain. Their axons move to the opposite side and, as part of the anterior cord of the spinal cord, descend to the corresponding segments of the spinal cord (see Fig. 23). Then they enter the anterior horns and end on the motor neurons of the spinal cord (the second neuron of the system).
vestibulospinal tract
connects the vestibular nuclei of the hindbrain (pons) and provides regulation of body muscle tone (see Section 5.3.2.).
Reticulospinal tract
connects RF neurons and spinal cord neurons, providing regulation of their sensitivity to control impulses (see Section 5.3.2.).
Corticopontine-cerebellar tract
allow the cortex to control the functions of the cerebellum. The first neurons of this system are located in the cortex of the frontal, temporal, occipital or parietal lobe. Their neurons (corticopontine fibers) pass through the internal capsule and are directed to the basilar part of the pons, to the intrinsic nuclei of the pons. Here there is a switch to the second neurons of this system. Their axons (pontocerebellar fibers) pass to the opposite side and are directed through the middle cerebellar peduncle to the contralateral cerebellar hemisphere.
- Main ascending paths.
A. Ascending to the hindbrain: posterior spinocerebellar tract of Flexig, anterior spinal cerebellar tract of Govers. Both spinocerebellar tracts conduct unconscious impulses (unconscious coordination of movements).
Ascending to the midbrain: lateral spinal midbrain (spinotectal) tract
To the diencephalon: lateral spinothalamic tract. It conducts temperature irritations and pain; the anterior spinothalamic is the pathway for conducting impulses of touch and touch.
Some of them are fibers of primary afferent (sensitive) neurons running without interruption. These fibers, the thin (Gaull's bundle) and wedge-shaped (Burdach's bundle) bundles, are part of the dorsal funiculi of the white matter and end in the medulla oblongata near the neutron relay nuclei, called the nuclei of the dorsal funiculus, or the nuclei of Gaulle and Burdach. The fibers of the dorsal cord are conductors of skin-mechanical sensitivity.
The remaining ascending pathways begin from neurons located in the gray matter of the spinal cord. Because these neurons receive synaptic inputs from primary afferent neurons, they are commonly referred to as second-order neurons, or secondary afferent neurons. The bulk of fibers from secondary afferent neurons pass within the lateral funiculus of the white matter. The spinothalamic tract is located here. The axons of spinothalamic neurons cross and reach without interruption through the medulla oblongata and midbrain to the thalamic nuclei, where they form synapses with thalamic neurons. The spinothalamic tract carries impulses from skin receptors.
The lateral funiculi contain fibers of the spinocerebellar tracts, dorsal and ventral, carrying impulses from skin and muscle receptors to the cerebellar cortex.
The lateral cord also contains fibers of the spinocervical tract, the ends of which form synapses with relay neurons of the cervical spinal cord - neurons of the cervical nucleus. After switching in the cervical nucleus, this pathway goes to the cerebellum and brainstem nuclei.
The pain sensitivity pathway is localized in the ventral columns of white matter. In addition, the spinal cord’s own pathways pass through the posterior, lateral and anterior columns, ensuring the integration of functions and reflex activity of its centers.
The pyramidal system (synonymous with the pyramidal tract) is a set of long efferent projection fibers of the motor analyzer, originating mainly in the anterior central gyrus of the cerebral cortex, ending on the motor cells of the anterior horns of the spinal cord and on the cells of the motor nuclei that carry out voluntary movements.
The pyramidal tract comes from the cortex, from the giant pyramidal cells of Betz layer V field 4 in the corona radiata, occupying the anterior two-thirds of the posterior femur and the knee of the internal bursa of the brain. Then it passes through the middle third of the base of the cerebral peduncle into the pons (varolii). In the medulla oblongata, the pyramidal system forms compact bundles (pyramids), some of the fibers of which, at the level of the border between the medulla oblongata and the spinal cord, pass to the opposite side (pyramid decussation). In the brain stem, fibers extend from the pyramidal system to the nuclei of the facial and hypoglossal nerves and to the motor nuclei, crossing slightly above or at the level of these nuclei. In the spinal cord, crossed fibers of the pyramidal system occupy the posterior part of the lateral cords, and uncrossed fibers occupy the anterior cords of the spinal cord. The motor analyzer receives afferent impulses from muscles, joints, etc. These impulses pass to the cerebral cortex through the optic thalamus, from where they approach the posterior central gyrus.
In the anterior and posterior central gyri there are distributions of cortical points for individual muscles that coincide with the distribution of the corresponding muscles of the body. Irritation of the cortical part of the pyramidal system, for example, by a scar on the lining of the brain, causes Jacksonian seizures (see). When the function of the pyramidal system in the brain (see) is lost, paralysis or paresis appears (see), as well as pyramidal symptoms (increased tendon and the appearance of pathological reflexes, increased muscle paralysis). Damage to the corticonuclear tracts of the facial nerve leads to central paresis of this nerve. The lesion of the pyramidal system in the area of the internal bursa leads to hemiplegia (see). Damage to the pyramidal system in the brain stem results in a combination of pyramidal symptoms on the opposite side with symptoms of damage to the nuclei of the cranial nerves on the affected side - alternating syndromes (see). Damage to the pyramidal system in the spinal cord - see.
The pyramidal system (tractus pyramidalis; synonymous with the pyramidal path) is a system of long efferent projection fibers of the motor analyzer, originating in the anterior central gyrus of the cerebral cortex (cytoarchitectonic fields 4 and c) and partly from other fields and areas. The pyramidal system received its name from the so-called pyramids of the medulla oblongata, formed on its ventral surface by pyramidal tracts passing there.
In lower vertebrates there is no pyramidal system. It appears only in mammals, and its importance in evolution gradually increases. In humans, the pyramidal system reaches its maximum development, and its fibers in the spinal cord occupy about 30% of the diameter area (in great apes 21.1%, in dogs 6.7%). The representation of the pyramidal system in the cerebral cortex is the motor analyzer nucleus. In lower mammals, the nucleus of the motor analyzer is not spatially separated from the nucleus of the cutaneous analyzer and has a granular layer IV (a sign of the sensitive cortex). These nuclei mutually overlap, becoming increasingly isolated from each other as phylogenetic development progresses. They are most isolated in humans, although they also have remnants of overlap in the form of fields 3/4 and 5. In ontogenesis, the cortical nucleus of the motor analyzer differentiates early - at the beginning of the second half of uterine life. Until birth, area 4 retains granular layer IV, which represents a repetition in ontogenesis of the characters found in the early stages of mammalian phylogeny. Myelin covers the nerve fibers of the pyramidal system during the 1st year of life.
In an adult, the main cortical representation of the pyramidal system corresponds to cytoarchitectonic fields 4 and 6 of the anterior central gyrus of the brain. Area 4 is characterized by the presence of Betz giant pyramidal cells in layer V, agranularity (absence of granular layers) and a large cortical width (about 3.5 mm). Area 6 has a similar structure, but does not have Betz giant pyramidal cells. From these fields, from giant pyramidal cells of Betz and from other pyramidal cells of layers V and III, and according to modern data, from other fields and areas of the cerebral cortex, the pyramidal tract originates. It is formed by descending fibers of caliber from 1 to 8 microns and more, which in the white matter of the cerebral hemispheres, in the corona radiata, converge towards the internal bursa, where, forming a compact bundle, they occupy the anterior two-thirds of its posterior thigh and knee.
Then the fibers of the pyramidal system go to the middle third of the base of the cerebral peduncle. Entering the pons, they break up into separate small bundles that pass among the transversely located fibers of the frontal-pontine-cerebellar tract and the pons' own nuclei. In the medulla oblongata, the fibers of the pyramidal system again gather into a compact bundle and form pyramids. Here most of the fibers pass to the opposite side, forming a cross of the pyramids. In the brainstem, fibers to the motor cranial nerves (corticonuclear; tractns corticonuclearis) and to the anterior horns of the spinal cord (corticospinal; tractus corticospinals lat. et ant.) go together to the lower edge of the superior olive. Then the corticonuclear pathway gradually gives off its fibers to the motor nuclei of the facial, hypoglossal, trigeminal and vagus nerves. These fibers cross at the level of the nuclei or directly above them. Corticospinal fibers descend into the spinal cord (see), where the intersecting fibers of the pyramidal system are concentrated in the lateral column, occupying its posterior part, and the non-intersecting fibers pass in the anterior column. Ending on the motor cells of the anterior horns (or on the intercalary cells) of the spinal cord, the fibers of the pyramidal system, gradually depleting, reach the sacral part of the spinal cord. The number of fibers of the pyramidal system exceeds 1 million. In addition to motor fibers, there are also autonomic fibers.
The cortical section of the pyramidal system, or the motor zone of the cerebral cortex, is the core of the motor analyzer. The analyzer, or afferent, nature of this nucleus is confirmed by the afferent fibers coming to it from the optic thalamus. As has been established, the fibers of the pyramidal system originate from a wider area of the cerebral cortex than the anterior central gyrus and the pyramidal system is closely connected with the extrapyramidal system, especially in the cortical region (Fig. 1). Therefore, with a variety of localizations of brain lesions, the pyramidal system usually suffers to one degree or another.
Physiologically, the pyramidal system is a system that carries out voluntary movements, although the latter are ultimately the result of the activity of the entire brain. In the anterior central gyrus there is a somatotopic distribution of cortical points for individual muscles, electrical stimulation of which causes discrete movements of these muscles. The muscles performing the most subtle working voluntary movements are especially widely represented (Fig. 2).
Rice. 1. Diagram of the pyramidal tract and the distribution of places of its origin in the cerebral cortex: 1 - limbic region; 2 - parietal region; 3 - precentral region; 4 - frontal region; 5 - insular region; 6 - temporal region; 7 - visual thalamus; 8 - inner bag.
Rice. 2. Scheme of somatotopic distribution of muscles of the limbs, trunk and face in the cortex of the anterior central gyrus (according to Penfield and Baldry).
Lesions of the pyramidal system in lower mammals do not cause significant impairment of motor functions. The higher the mammal is organized, the more significant these disturbances are. Pathological processes in the cortical part of the pyramidal system, especially in the anterior central gyrus, irritating the cerebral cortex, cause partial (partial), or Jacksonian, epilepsy, manifested mainly by clonic spasms of the muscles of the opposite half of the face, trunk and limbs on the opposite side. Loss of functions of the pyramidal system is manifested by paralysis and paresis.
Lesions of the pyramidal system are detected by neurological examination of voluntary (active) movements, their volume in various joints, muscle strength, muscle tone and reflexes in combination with other neurological symptoms. Electroencephalography and electromyography are gaining increasing diagnostic importance. With unilateral damage to the cerebral cortex in the area of the anterior central gyrus, monoplegia and monoparesis of the arm or leg of the opposite side of the body are most often observed. Damage to the corticonuclear tracts of the facial nerve is usually expressed by central paresis of the lower and middle branches of this nerve. The upper branch is usually less affected due to its bilateral innervation, although its lesion can often be identified (the patient cannot close the eye on the affected side in isolation). A focal lesion of the pyramidal system in the area of the internal bursa usually leads to hemiplegia (or hemiparesis), and with bilateral lesions to tetraplegia.
Lesions of the pyramidal system in the area of the brain stem are determined by the combination of pyramidal symptoms on the opposite side with damage to the nuclei of the cranial nerves or their roots on the affected side, that is, by the presence of alternating syndromes (see).
With pyramidal hemiplegia and hemiparesis, the distal parts of the limbs are usually most affected.
Hemiplegia and hemiparesis with damage to the pyramidal system are usually characterized by increased tendon reflexes, increased muscle tone, loss of skin reflexes, especially plantar reflexes, the emergence of pathological reflexes - extensor (Babinsky, Oppenheim, Gordon, etc.) and flexor (Rossolimo, Mendel-Bekhterev, etc. ), as well as protective reflexes. Tendon and periosteal reflexes are evoked from the expanded zone. Cross reflexes and friendly movements appear - so-called synkinesis (see). In the initial stages of pyramidal hemiplegia, muscle tone (and sometimes reflexes) is reduced due to diaschisis (see). An increase in muscle tone is detected later - 3-4 weeks after the onset of the lesion. Most often, especially with capsular lesions, increased muscle tone predominates in the forearm flexors and leg extensors. This distribution of muscle hypertension leads to the appearance of Wernicke-Mann type contracture (see Wernicke-Mann type of contracture).
Neurology is one of the most exact sciences of medicine. With the help of topical diagnostics, a neurologist, using a hammer, questioning and examination, as well as samples and various tests, can in some cases localize the lesion with high accuracy. This lesion may be located in the spinal cord or head. Previously, this was an applied science, and before that it was a descriptive science (anatomy also always belonged to a descriptive science).
Diagnostics
Diagnosis of pyramidal insufficiency is based on consultation with a neurologist.
In childhood, the doctor identifies developmental delays from their peers, impaired coordination and orientation in space, increased tone of the lower leg muscles, the appearance of pathological reflexes, etc. A spinal puncture may be performed to confirm the diagnosis.
In adults, the diagnosis of such conditions consists of examining all reflexes (superficial and deep), measuring muscle strength with a dynamometer, measuring biopotentials and electrical conductivity in the muscles.
Instrumental research methods include computed tomography, magnetic resonance imaging, and ultrasound examination of cerebral vessels. With their help, you can accurately determine the level of localization of the pathological focus to confirm the diagnosis. After this, patients will be provided with the appropriate level of medical and/or surgical therapy.
In childhood, it is necessary to undergo physiotherapy courses. Children's massage helps reduce muscle tone and prevents the development of scoliosis by strengthening the muscular system of the spine.
Therapeutic gymnastics, water procedures, hardening also help in the fight against hypertension.
Physiotherapeutic measures also include electrophoresis, manual therapy, mud baths and more. Drug treatment is based on the use of drugs that accelerate metabolic processes in neurons, improve the conduction of impulse signals and drugs that stabilize muscle tone.
Drugs that carry out full metabolism include Actovegin, piracetam, and gamma-amino-butyric acid.
For stable passage of the pulse wave, proserin or dibazole is required. To reduce muscle tone and strengthen the muscular system, B vitamins and antioxidants are used - vitamin E, mydocalm, baclofen.
With the progression of pyramidal insufficiency, surgical treatment is performed.
What is a pyramid system?
The pyramidal tracts (or system) are called the corticospinal, efferent, or descending tracts. They originate in the place where the precentral gyrus is located, or more precisely, in the gray matter of this gyrus. The neural bodies are located there. They produce impulses that give commands to the striated (skeletal) muscles. These are conscious impulses; the pyramidal system is easy to subordinate to the will of the mind.
The function of the pyramidal tract is to perceive the program of voluntary movement and conduct the impulses of the program to the brain stem and spinal cord. The pyramidal and extrapyramidal (unconscious) systems are united into a single system, which is responsible for movement, coordination of balance and muscle tone.