General information
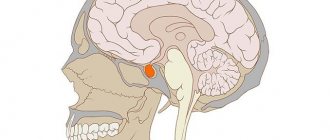
Externally, the pituitary gland resembles a small ball hidden under the cerebral cortex, in the depression of the sella turcica. Its size is only 7-11 millimeters. Its weight is only half a gram. However, such modest dimensions do not prevent the gland from producing a fairly extensive list of important hormones.
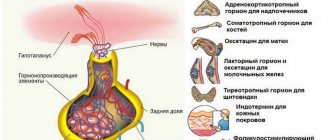
All pituitary lobes are under the control of the hypothalamus. There are three of them:
- front;
- back;
- average.
Moreover, the first two have their own unique functions.
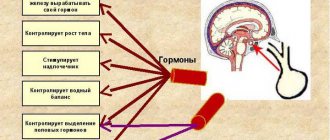
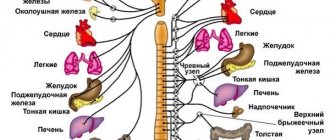
The hypothalamus, in turn, is the subcortical center that controls the entire ANS (autonomic nervous system). This part of the brain monitors the state of the body and, at the slightest change, releases special substances:
- statins;
- libertines.
They actually regulate the flow of hormones into the blood.
The largest part of the gland is located in front. It is called the adenohypophysis. Thanks to her, people receive a number of vital
essential protein hormones, mainly involved in the metabolic process.
The list of biologically active substances looks like this:
- somatotropin (affects human growth, its excess activates bone development, deficiency, on the contrary, stops);
- prolactin is probably the most famous hormone that helps women produce breast milk (it’s not hard to imagine why its deficiency is dangerous);
- thyroid-stimulating hormone ensures normal functioning of the thyroid gland;
- adrenocorticotropic stimulates the adrenal cortex;
- a number of gonadotropins are responsible for sexual function - both in the female and male bodies.
The posterior lobe is called the neurohypophysis. Only two substances are produced here:
- oxytocin;
- vasopressin.
Without the first, in principle, the normal activity of our intestines is impossible - it stimulates the contraction of its smooth muscles, that is, it affects peristalsis. Similarly, oxytocin is involved in the functioning of the bladder and gall bladder.
Among other things, in women it is produced in large quantities directly during childbirth, which leads to increased contractions of the uterus. Eventually contractions begin and the baby is pushed out.
Oxytocin also ensures the functioning of the mammary glands - without it, in fact, the nutrient fluid would not be able to leave the breast of a nursing mother.
Vasopressin is responsible for:
- water retention in the body;
- salt removal.
Its deficiency leads to very rapid and extremely dangerous dehydration of the body.
The pituitary gland connects directly to the hypothalamus through a stalk through which as many as 7 arteries pass.
Unfortunately, at the moment all the functions of the gland are not fully understood. Most likely, we will not soon learn all its secrets.
Hypogonadism with hypothalamic syndrome (with organic lesions of the hypothalamus or pituitary gland)
It can develop after infectious and inflammatory diseases, tumors and injuries of the hypothalamic-pituitary region and occurs as a result of a decrease or loss of gonadotropic and other functions of the adenohypophysis.
The clinical course is similar to adiposogenital dystrophy, however, unlike the latter, there is organic damage to the pituitary gland or hypothalamus; it occurs and manifests itself at any age, including in adults.
The etiology of this form of acquired secondary hypogonadism includes possible intrauterine infections (encephalitis, toxoplasmosis, tuberculous meningoencephalitis), viral infection (influenza, scarlet fever, etc.
), traumatic injuries of the skull (including birth injuries), tumors of the pituitary gland (chromophobe adenomas, cysts, gliomas, gliosarcoma) or tumors of the gray tubercle, medulla oblongata, compressing the pituitary gland. The lesion can also be localized in the mediobasal hypothalamus, which regulates the secretion of gonadotropins.
The pathogenetic mechanisms include hypofunction of gonadotropic, as well as thyroid-tropic and corticotropic structures. This causes a reduced function of the corresponding peripheral glands, especially the reproductive glands. The clinical picture is similar to adiposogenital dystrophy, and the degree of its severity depends on the nature and degree of loss of gonadotropic and other tropic functions of the pituitary gland.
After tumor removal, panhypopituitarism develops. If the pathology occurs in an adult, regression of secondary sexual characteristics is observed. Symptoms of loss of tropic functions may appear gradually and non-simultaneously. Sometimes the first sign of a pituitary tumor is decreased sexual activity.
Essential in diagnosis, in addition to assessing clinical and hormonal parameters, is skull radiography. In the case of a previous tuberculosis process, inclusions of petrificates above the sella turcica are detected in the hypothalamic region. Tumors give a specific x-ray picture. The nature of therapy is determined by the cause.
For tumors, surgery, radiation therapy, and symptomatic hormone therapy are indicated. For infectious processes - anti-inflammatory therapy. Hormone therapy for hypogonadism (gonadotropins and, if necessary, androgens) should be accompanied by therapy for obesity.
Hyperprolactinemic hypogonadism has been identified as a separate form of central hypogonadism only in recent years with the development of laboratory radio-immunological diagnostics in endocrinology. The syndrome of lactorrhea, gynecomastia and testicular hypoplasia in men with a pituitary adenoma is known as O'Connelly syndrome. Lactorrhea in men is most often a symptom of pituitary prolactinoma; rarely, the latter is not accompanied by lactorrhea and gynecomastia.
In recent years, special attention has been paid to the significant role of prolactin in the male body, the hypo- and hyperproduction of which negatively affects the function of the generative system. Hyperprolactinemia accompanies infertility and sexual disorders, and occurring in the pre- and pubertal periods leads to delayed sexual development and hypogonadism.
The cause of hyperprolactinemia can be a tumor of the pituitary gland - prolactinoma, tumor processes in the hypothalamus (hypothalamic hyperprolactinemia), often - hypothyroidism (dishormonal hyperprolactinemia), extremely rarely - Itsenko-Cushing's disease, the use of certain drugs (drug-induced hyperprolactinemia), the consequences of anatomical destruction of the connection between hypothalamic centers and pituitary gland with switching off the mechanism that inhibits prolactin inhibition factors. The absence of tumor processes in the pituitary gland with hyperprolactinemia in some patients suggests the presence of a microadenoma that secretes prolactin. The pathogenesis of hyperprolactinemic hypogonadism is a violation under the influence of a long-term excess of secretion and metabolism of T, its transformation into DHT in the pre-crucible gland and other target tissues, gradual suppression of the secretory activity of testicular interstitial endocrinocytes, and subsequently, disruption of spermatogenesis. An essential element of hypoandrogenism in prolactinemia is the suppression of the secretion of gonadotropins, primarily LH. It is believed that in infertile men with hypogonadism and hyperprolactinemia, the neural mechanism that regulates the pulsatile secretion of gonadotropin-releasing hormone is impaired.
Hyperprolactinemia , which occurs in childhood and adolescence, leads to delayed sexual development, underdevelopment of the genital organs, secondary sexual characteristics and is accompanied by general symptoms that occur with T deficiency. Lactorrhea is typical. Gynecomastia is not necessary. Hyperprolactinemia that occurs in an adult leads to regression of primary, secondary and tertiary sexual characteristics, typical symptoms of hypoandrogenization, varying degrees of severity of lactorrhea, loss of sexual activity, and infertility develop.
In patients with hypogonadism and lactorrhea, it is necessary to determine the level of prolactin in the blood, which can be increased several times (and with prolactinoma - hundreds of times). prolactin may be increased in acromegaly, Itsenko-Cushing's disease, some visceropathies, and in some cases of primary hypogonadism.
However, this increase is not as high as with hyperprolactinemic syndrome. X-rays of the skull and visual field examination are mandatory. Detection of an enlarged sella turcica with a sharp increase in PRL levels indicates a tumor of the pituitary gland (prolactinoma).
A tumor of the pituitary gland leads to a narrowing of the visual field.
In the diagnosis of hyperprolactinemia, a detailed history plays a significant role: previous diseases and the nature of treatment.
Drugs that contribute to the development of hyperprolactinemia are the following: antidepressants (imipramine, amitriptyline), antihypertensives (reserpine, methyldopa), phenothiazine group (aminazine, haloperidol).
In case of drug-induced hyperprolactinemia, the doses are reduced or the drugs that caused the pathology are discontinued, parlodel (bromocriptine), metergoline, pergolide, L-DOPA are prescribed under the control of the level of PRL in the blood plasma, 2 - 4 tablets per day with a preliminary test for drug tolerance (1/2 tablet at night) and provided that the PRL level decreases under its influence. For severe hypogonadism, simultaneous use of hCG or androgens is useful. Typically, patients regain sexual activity and fertility. In case of hyperprolactinemia associated with hypothyroidism, Itsenko-Cushing's disease, the underlying disease should be treated first. For pituitary tumors, external beam radiation therapy and parlodel are first used. If there is no effect, especially when vision is narrowed, surgical removal of the tumor is indicated. The signs of hypopituitarism that arise after this are corrected by hormone replacement therapy in accordance with the deficiency of a particular hormone.
Source: //farm7.ru/blog/farmakologiya/gipogonadizm-pri-gipotalamicheskom
Pathologies developing against the background of pituitary dysfunction
Having figured out where the pituitary gland is located specifically in a person, it is worth talking in more detail about the dangers that arise due to its malfunction.
It can be considered a completely proven fact that the proper functioning of the gland is a guarantee of excellent health and longevity. In fact, it acts as a specific regulator of the basic processes that ensure the vital functions of the body.
In particular, a tumor of the pituitary gland or another part of the brain causes a dangerous hormonal imbalance. In all cases, a deficiency of some biologically active substances develops. This, in turn, leads to the onset of the following severe diseases of the endocrine system:
- hypothyroidism;
- dwarfism;
- delayed puberty;
- impotence.
An excess of hormones provokes:
- hypertension;
- mental disorders;
- diabetes;
- infertility;
- gigantism;
- sexual dysfunction.
All of these diseases appear precisely as a result of disruption of the pituitary gland caused by the impact of the resulting tumor.
Most often we are talking about an adenoma - a benign neoplasm that grows on glandular tissue. Its development can be provoked and accelerated by:
- traumatic brain injuries;
- neuroinfection;
- mechanical damage to the brain.
Epiphysis
The pineal gland (pineal body, superior cerebral appendage) is a neuroendocrine organ that receives information from the nervous and endocrine systems, which then integrates into it and regulates the activity of its cells; height 5-8mm, diameter 3-5mm, weight 100-200mg.
Functional characteristics. Participates in the regulation of processes that occur rhythmically and cyclically in the body, for example, the ovarian-menstrual cycle in women. Rhythmic oscillations of other periodic functions, the intensity of which naturally changes throughout the day, are called circadian; they are clearly related to the change of day and night. That. The hormone-forming activity of the pineal gland is determined by its ability to distinguish between changes in light stimuli received by the body.
Development. 1).Protrusion of the roof of the 3rd gland at 5-6 weeks (neuroglial origin). 2).The subcommissural organ develops from the ependyma of the 3rd gland. brain (reduced in humans and mammals). 3). The pineal gland develops to its maximum up to 7 years of age.
How does an adenoma act on the pituitary gland?
The tumor itself is not dangerous, since it almost never becomes malignant. However, as it grows, the pressure on the surrounding tissue and directly on the gland itself increases.
Basically, all symptoms appear against the background of the emerging endocrine-metabolic syndrome. Its development is accompanied by ophthalmic neurological changes. Patients mostly complain about:
- severe headaches;
- inability to move your eyes normally;
- changed viewing angle (the adenoma puts pressure on the apples from the inside and as a result they protrude outward).
The doctor chooses treatment options based on:
- the patient's condition;
- the contraindications it has;
- the complexity of the disease.
Large tumors are removed surgically. Small ones are treated with conservative methods.
Neoplasms are divided into:
- macroadenomas (size 10 millimeters or more);
- microadenomas (up to 3 mm).
The thyroid gland and its main functions
The thyroid gland is a small organ located on the front of the neck.
The size of the organ does not exceed 4 cm; its shape resembles a butterfly. Despite the fact that the organ is small, it provides many important functions:
- hormone production;
- weight control;
- normal mental and physical development;
- regulation of the production of calcitonin, which regulates the concentration of calcium in the body;
- ensuring water-salt balance in the body;
- The thyroid gland takes part in the production of vitamin A in the liver.
It is worth noting that thyroid diseases are more common in women; many experts associate this with the greater need of the female body for such substances. The female body is designed in such a way that it must bear and give birth to a child; with hormonal imbalance, this is impossible.
How is adenoma diagnosed?
If there is a suspicion of the development of a benign tumor, the patient is sent for an MRI and a number of other examinations. If the diagnosis is confirmed, treatment begins immediately. As a rule, only medications or radiation are initially used. Both methods have proven effective in the early stages. They are not particularly suitable for advanced tumors.
It is most difficult to treat when an adenoma is detected in pregnant women. In this case, no treatment options are used until the baby is born. Doctors only closely monitor the woman’s condition.