In modern ophthalmology, the susceptibility of the visual fields is considered a serious criterion for the diagnosis of many eye diseases. Problems with it can indicate both visual impairments and disorders of the central nervous system. The loss of certain segments of the visual field is called hemianopsia. This pathology belongs to the category of polyetiological diseases, which means that its development can be provoked by a large number of different factors. Depending on the degree of damage to parts of the brain, hemianopia can be temporary or permanent.
Which doctors should you contact if you have Hemianopsia:
Ophthalmologist
Is something bothering you? Do you want to know more detailed information about Hemianopsia, its causes, symptoms, methods of treatment and prevention, the course of the disease and diet after it? Or do you need an inspection? You can make an appointment with a doctor - the Eurolab clinic is always at your service! The best doctors will examine you, study external signs and help you identify the disease by symptoms, advise you and provide the necessary assistance and make a diagnosis. You can also call a doctor at home. The Eurolab clinic is open for you around the clock.
How to contact the clinic: Phone number of our clinic in Kyiv: (+38 (multi-channel). The clinic secretary will select a convenient day and time for you to visit the doctor. Our coordinates and directions are listed here. Look in more detail about all the clinic’s services on its personal page.
Useful video
Irina Sergeevna Mironova’s story about the causes and features of the development of the pathological condition:
Author's rating
Author of the article
D. Aleaxndrescu
Articles written
2031
about the author
Was the article helpful?
Rate the material on a five-point scale!
( 1 ratings, average: 2.00 out of 5)
If you have any questions or want to share your opinion or experience, write a comment below.
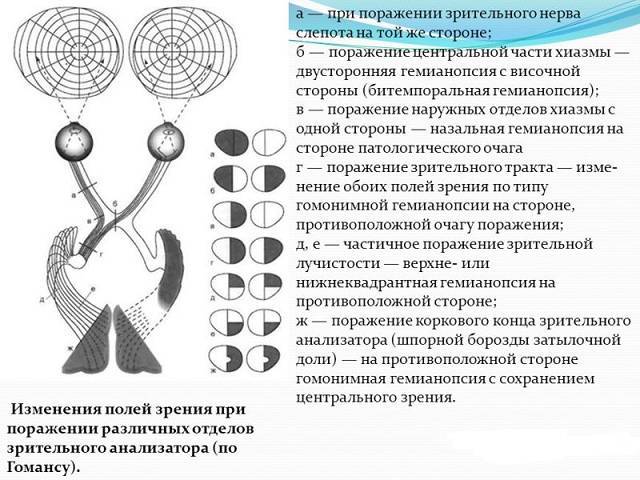
Classification and types of violations
Modern medicine distinguishes several types and subtypes of hemianopsia.
The homonymous form is one of the most common forms
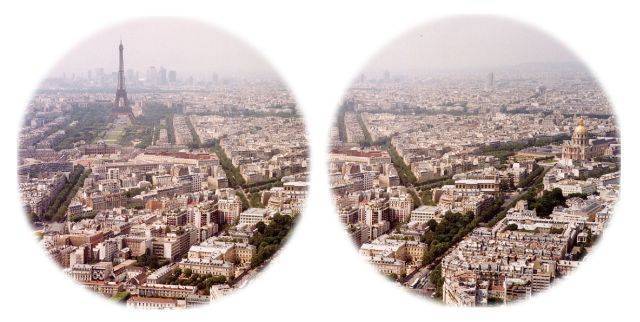
Homonymous anopsia is a pathological condition during the development of which the patient ceases to perceive the right or left area of the visual field.
Homonymous hemianopsia can be either right-sided or left-sided. It occurs due to damage to the cortex of the occipital lobes, with right-sided on the left, and with left-sided on the right.
This pathology is also divided into complete, square and partial. The type of disease depends on which area is affected.
Additionally, this form of the disease is divided into congenital and acquired. Acquired homonymous hemianopia is observed with damage to the central nervous system and brain due to stroke, traumatic brain injury, unsuccessful surgery or tumor.
All this leads to inflammation of the optic nerves. They are compressed, which impairs blood circulation, and they are additionally negatively affected by toxins. In this situation, dysfunction of the visual tracts develops.
Transient homonymous hemiopia is a pathology that is caused by diseases of the cerebral vessels. It is also called transient, because in this case there is a disruption of blood circulation in the vessels of the brain.
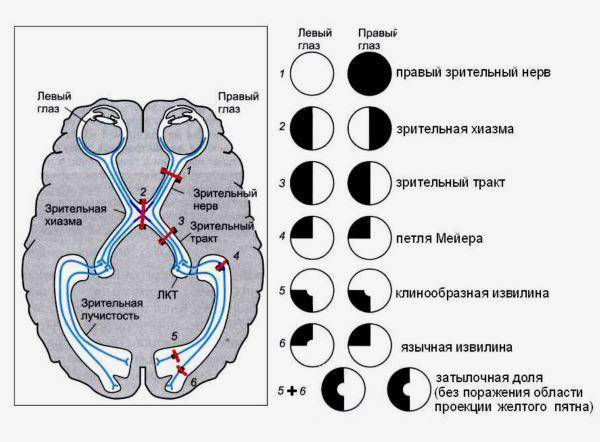
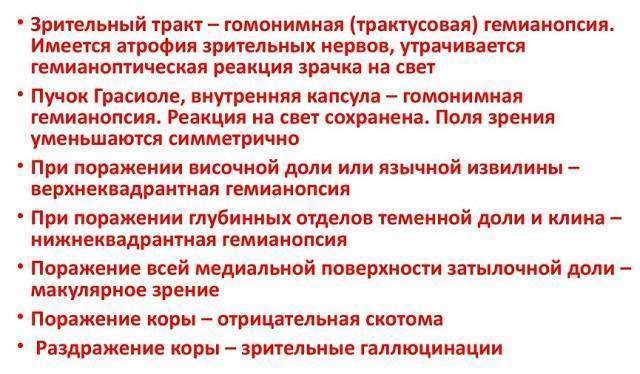
In all the situations described, the focus of inflammation has a specific localization. Thus, if the parietal lobe is affected, the person develops inferior quadrate homonymous hemianopsia. Due to damage to the temporal region, superior quadratic or complete form of hemiopia develops.
Signs that indicate the appearance of this disease, in particular after a stroke or other brain damage, are primarily the occurrence of visual hallucinations.
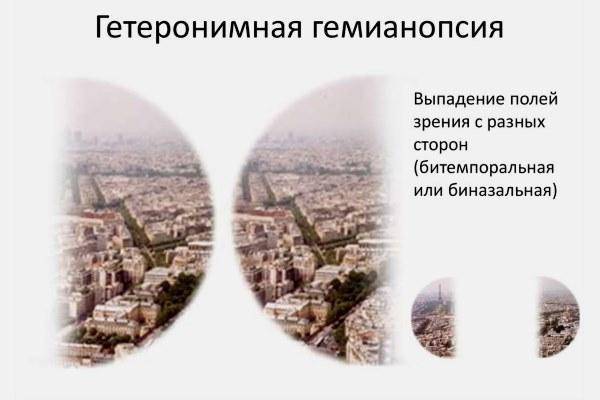
Heteronymous form
Heteronymous hemianopsia is a pathology accompanied by loss of perception of the nasal or temporal areas of the visual field. Here, too, the full, partial and square forms of the disease are distinguished.
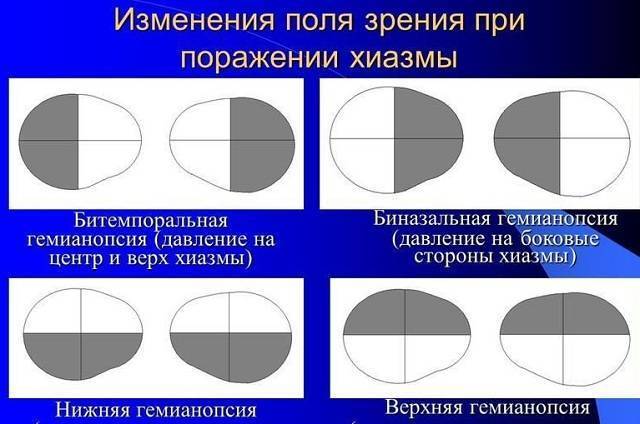
Bitemporal form is the most common
Bitemporal hemianopia is characterized by a lack of visibility in the upper parts of the visual field in both eyes. This pathology occurs in patients more often than the previous two. It can lead to:
- damage to the pituitary part where the optical fibers intersect;
- lesion of the medial part of the chiasm.
The location of the blind spot will depend on how much pressure is applied to the chiasm.
Binasal hemiopia
Binasal hemianopsia is a disease that occurs with loss of visibility of the lower, in other words, nasal region of the visual field.
Heteronymous binasal blindness is a pathology accompanied by the simultaneous appearance of several lesions that put pressure on the literal region of the chiasm.
The development of this form of disorder is influenced by chiasmatic arachnoiditis, as well as empty sella syndrome.
The development of pathology in one eye with complete blindness of the second is a disease accompanied by loss of visibility of a portion of the visual field, which spreads only to one eye, with the second becoming completely blind.
This pathology is divided into nasal and temporal. The difference between the latter is that one eye becomes completely blind, and the second one loses the upper half of its field of vision. This condition develops when the optic fibers of the chiasm are completely damaged.
The diagnosis of “nasal hemianopsia” is very rare. Its difference is that in this case the lower half of the visual field falls out.
This condition usually develops over a long period of time. First, partial blindness occurs in both eyes at once. Later, it begins to progress and in case of improper therapy or complete absence of treatment, after some time, the left or right eye becomes completely blind.
Bilateral hemianopsia is a condition in which vision is lost in both eyes at once. In this case, several lesions appear above the chiasma.
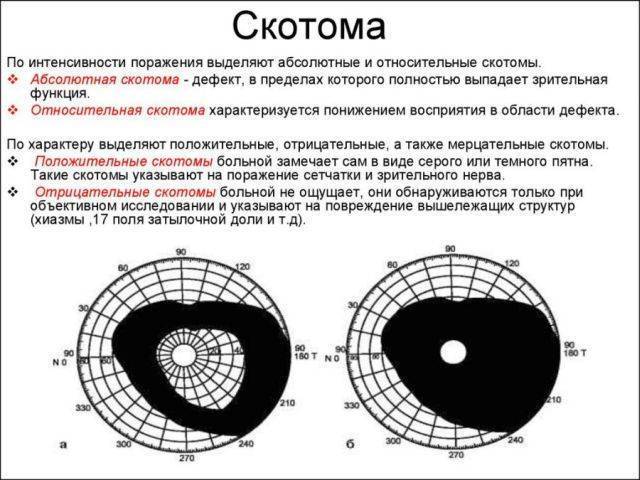
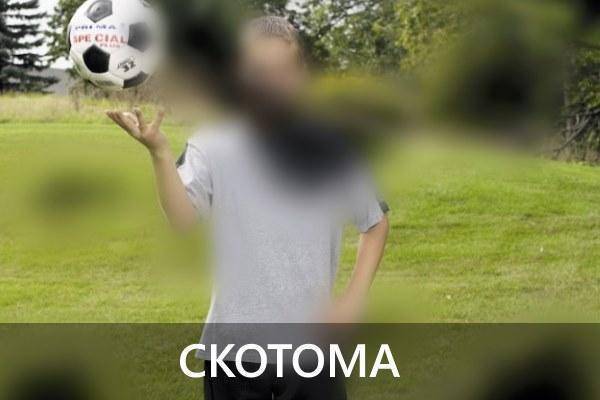
A scotoma is a dark area formed in the field of vision. It comes in various shapes. Scotoma has no connection with the peripheral borders, and therefore can manifest itself in absolutely any part of the visual field.
Types of disease

Modern science identifies several types of this disease. In addition to bitemporal, there are other types of hemianopsia.
One of them is symmetrical or homonymous hemianopsia. While in this state, the patient is unable to distinguish between both right or both left halves of the visual field. In this case, the temporal half of the right eye and the nasal half of the left eye fall out (or vice versa).
This condition in most cases is a consequence of damage to the optic tract. When the left optic tract is involved in the pathological process, we speak of right-sided hemianopia. A typical and reverse situation: with damage to the right tract, the patient does not see the left areas of the visual field. In this case, a diagnosis of left-sided hemianopsia is made.
Bilateral development of this disease is also possible. In this case, doctors diagnose contralateral hemianopsia. This is a specific neurological disorder that is characterized by bilateral blindness.
Massage for hemiparesis
Massage for hemiparesis is performed for:
- reducing reflex excitability of spastic muscles;
- weakening muscle contractures;
- activation of relaxed muscles;
- normalization of movements;
- elimination of trophic disturbances.
For paresis, massage is performed on the paretic limbs, back, lower back, and chest on the affected side. The procedure is carried out according to the following scheme:
- To begin, massage the front surface of the leg.
- After this, a massage of the pectoral muscle on the affected side is performed.
- Next, the specialist proceeds to massaging the affected arm.
- The patient lies on his stomach or side. Then a massage is performed on the back of the leg and back.
Massage for paresis is carried out using the following techniques:
- stroking;
- spiral rubbing;
- kneading;
- soft, longitudinal pressure;
- felting
It is strictly forbidden to use percussive massage techniques with a diagnosis such as hemiparesis!
It is useful to conduct hydromassage sessions at home. Physiotherapeutic and mud massages also help well.
Features of treatment
Before starting treatment, you should undergo a diagnostic examination. Patients are advised to consult an ophthalmologist and a neurologist. To make an accurate diagnosis, MRI, CT, and ultrasound may be required.
Important! If left untreated, hemianopia will progress and lead to complete loss of vision. Depending on the severity, nature of the disease, as well as the degree of damage, the pathology is a temporary phenomenon or remains a permanent symptom
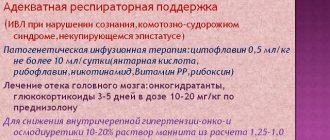
Therapeutic tactics are selected taking into account the pathological factor:
Depending on the severity, nature of the disease, as well as the extent of damage, the pathology is a temporary phenomenon or remains a permanent symptom. Therapeutic tactics are selected taking into account the pathological factor:
- if the underlying disease is migraine, the patient is prescribed nasal sprays with sumatriptans;
- for hydrocephalus, diuretics are prescribed;
- To combat stroke, rehabilitation therapy is prescribed. Drugs are used to normalize blood circulation and regenerate damaged tissues;
- For oncology, surgery, chemotherapy or radiation therapy can be used.
After the treatment, it is possible to fully recover or become disabled due to vision loss. The outcome is influenced by a large number of factors:
- degree of severity of the process;
- duration of visual impairment;
- treatment methods;
- general condition of the patient;
- time to start treatment;
- the presence of concomitant pathologies and complications;
- age indicators.

If alarming symptoms are detected, you should immediately contact a specialist. The patient can make reading easier by increasing the size of small eye movements along the line. To do this, the text should be held at a right angle and read vertically. In the right-hand process, the text must be rotated so that it can be read from top to bottom, with the next line being in the left half of the visual field. In order to better navigate in space, the eye should be turned to the blind half.
To improve visual functions for patients with hemianopsia, special programs have been developed. The treatment course helps to compensate for the loss of the visual field and to navigate in space.
Classification
Homonymous
With this type, the patient is not able to immediately identify two left or two right halves of the visual field.
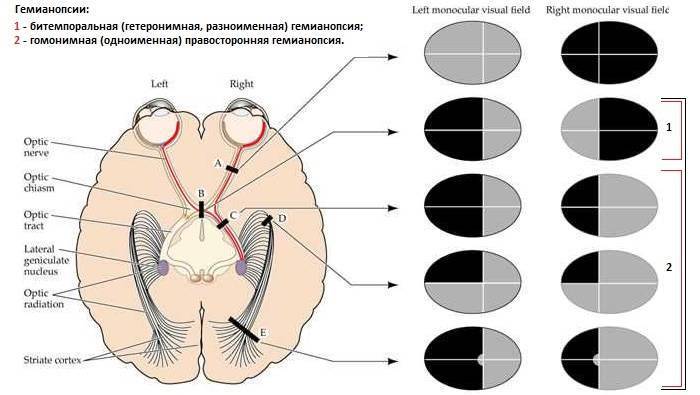
The pathological process is characterized by loss of the temporal half of the visual field. The disease is caused by damage to the optical tract on the side opposite to loss of peripheral vision.
Heteronymous
Bitemporal
The lesion is located in the optic chiasm, compressing the dissecting fibers. Most often caused by abnormal growth of the pituitary gland, which gives way to the optic chiasm.
Partial blindness. The perception of the outer half of the visual fields of both eyes is lost. Most often, the bitemporal form is the result of tumors that are located in the central region of the optic nerve intersection.

The nerve fibers from the nasal halves of the retina are the only ones that cross to the other side of the brain, resulting in loss of vision only on the temporal side.
Binasal
This form is also associated with damage to the uveal tract and central nervous system. Binasal hemianopsia develops when the lateral parts of the chiasm fibers are affected on both sides.
This form of the disease is found in patients with sclerotic lesions of the internal carotid artery on both sides.
Quadrant
Left superior quadrant hemianopsia is a visual defect that occurs when the inferior optic emitting fibers (Meyer's loop) in the temporal lobe of the brain are damaged. Strokes involving the middle cerebral artery can lead to the development of this form of blindness.
Temporal lobe lesions cause other neurological manifestations, including aphasia, memory deficits (if hemisphere dominant), seizures, and auditory and visual hallucinations.
The left lower homonymous form of pathology is damage to the upper fibers in the parietal lobe. Because the parietal lobe is considered the primary sensory area of the cerebral cortex, these lesions often cause sensory deficits.
Gerstmann's syndrome (finger agnosia, agraphia, acalculia and right-sided disorientation) accompanies this defect if the dominant angular lobe of the gyrus is involved. Contralateral heminglect (inability to recognize the visual field opposite the area of traumatic brain injury) is observed with lesions of the parietal lobe of the non-dominant hemisphere, which is difficult to distinguish from this defect.
One-sided
Right-sided blindness occurs when the lesion is located in front of the optic chiasm. Has a wide differential, including corneal diseases or cataracts to optic neuritis. If the site of the stroke is the optic nerve, patients will usually have a relative afferent pupillary defect.
The left-sided form of the disease results from damage to the optic tract en route to the lateral genital body of the thalamus, and damage just after the radiating fibers leave the lateral genital body.
Double-sided
A type of pathology in which defects are found in both corner spaces visible to the eye with a fixed gaze. The pathological condition develops in the presence of several foci in the optical pathways, tracts, and occipital lobe.
Scotoma
This is a blind spot in the visual field. Scotoma takes different shapes - oval, round, arched. It can form in different parts of the visual field and is not associated with peripheral boundaries.

Classification and symptoms
The manifestation of visual pathology depends on the reason and in what area the damage occurred. A classification has been developed that takes into account the types of disease and their symptoms.
Hemianopsia disorder is characterized by loss of one or more visual fields. The patient cannot see part of the picture with one or both eyes. Taking into account which field falls out, types of hemianopsia are distinguished. Damage occurs in different areas of the brain:
- neurons of the occipital lobe - 39%;
- areas of the parietal cortex - 33%;
- temporal sulci - 24%;
- optic tract - 4%.
Homonymous
This is a symmetrical form of pathology, during which a person cannot see the right or left side of the image. There are several homonymous forms of the disorder:
- right-sided homonymous hemianopsia - the right fields disappear, the lesion occurs in the left half of the brain;
- with left-sided homonymous hemianopia, the left fields disappear, and the lesion appears on the right.
Since either the entire visual field or part of it can fall out, there are also types of homonymous hemianopia:
- complete left-sided or right-sided hemianopsia - when the whole half of the image is not visible;
- homonymous quadrant hemianopsia - the image is not visible only in the upper or lower quadrant;
- with upper quadrant homonymous hemianopsia, the person does not see the upper corner of the image on the right or left;
- with the lower quadrant homonymous form, the lower right or left corner is not visible, respectively.
Complete homonymous hemianopsia disorder develops with a pathological process in the parietal lobe, quadrant homonymous - with damage to the temporal lobe. If the occipital lobe is affected, contralateral homonymous hemianopsia develops.

Heteronymous
With this form, the top or bottom margins disappear. The classification of the heteronymous form is as follows:
- bitemporal hemianopsia - the patient is unable to see the upper halves of the image;
- binasal hemianopsia - the patient is unable to see both lower halves of the image.
The bitemporal form develops due to damage to the pituitary gland. Binasal hemianopia occurs when the optic fibers are damaged.
Double-sided
With this type, the patient does not see the image with both eyes. Damage occurs in the right and left visual areas of the brain. There are two types of bilateral pathology:
- with the same defects in both eyes;
- with various defects.
The right or left parts of the image may fall out.
Scotoma
Scotoma is a visual impairment in which a person loses part of the image in the form of separate spots of various shapes. Blind spots occur in different parts of the eyes and can be single or multiple.
In addition to image loss, hemianopsia disorder also manifests itself with other symptoms:
- hallucinations;
- agnosia - a person cannot recognize previously familiar objects;
- the ability to fix your gaze on only one object.
These symptoms most often occur after a stroke. Patients often deny their illness.
Acquired hemianopsia causes impairment of a person's ability to work. It is difficult for the patient to carry out everyday activities, which affects his character and emotional state. Due to insufficient perception of the surrounding world, the gait is disturbed - it becomes uncertain, shuffling, and the person staggers when walking.
In the congenital form, symptoms of other abnormalities of brain development appear:
- paresthesia;
- disorders of pain and temperature sensitivity;
- hearing or speech impairment.
Hemianopsia – homonymous, bitemporal, quadrant
Bilateral hemianopsia is a neurological disorder characterized by bilateral blindness in half of the visual fields.
Tractus hemianopsia (from the word “path”) is caused by damage to the optical pathways, and central hemianopsia develops when the cortical areas responsible for visual perception are damaged.
In other words, hemianopsia is the loss of half of visible vision on the left or right, but always in both eyes.
Damage to the optic tract usually results in death of the optic nerves. With the central origin of the disease, the optic nerves do not atrophy and continue to function.
Loss of visual fields by origin is divided into acquired and congenital. The congenital variant occurs when the development of the central nervous system is impaired during the period of intrauterine maturation of the fetus.
It is almost always combined with other defects of the nervous system and rarely occurs as an isolated pathology. The acquired variant develops mainly in people whose average age is from 30 to 50 years.
More common in women.
Varieties
There are several types of neurological disease:
Homonymous hemianopsia (eponymous hemianopsia)
Unilateral hemianopsia is incomplete loss of vision. Characterized by loss of margins on the right or left. Homonymous hemianopsia occurs when the structures of the central nervous system are damaged by infection, stroke, or mechanical trauma.
Features of the pathology. The homonymous variant is reversible. Thus, right- or left-sided blindness can be a sign of aura during migraine. Aura is the preceding stage of a unilateral headache. Hemianopsia may be one of the signs of a stroke.
Contralateral hemianopsia occurs when there is unilateral damage to the optic nerve. For example, if the optic nerve on the left is damaged, the right lateral visual fields will fall out and right-sided homonymous hemianopsia (right hemianopsia) will occur. If the right optic nerve is damaged, there will be left-sided homonymous hemianopsia.
With complete damage to the lateral geniculate body, complete unilateral hemianopia occurs.
Bitemporal heteronymous hemianopsia
By breaking down each word, you can understand the term. “Bi” means two, “temporal” means the side of the temples of the head. The pathology is manifested by the disappearance of both fields of vision from the temples. Bitemporal hemianopsia occurs when the optic pathway is damaged in the area where the optic nerves intersect.
Heteronymous hemianopsia occurs when the optic nerves are damaged, most often caused by a tumor. Often these are neoplasms in or above the pituitary gland. Temporal hemianopsia is often a symptom of pituitary adenoma.
Binasal hemianopsia
Bi - this is two, that is, on both sides, nasal - meaning the nasal part. The pathology is characterized by bilateral loss of visual fields in the nasal part of the face. Binasal hemianopsia occurs when the optic tract and brain structures are damaged. Also, binasal hemianopsia occurs when the central nervous system is damaged against the background of hydrocele of the brain.
Upper quadrant hemianopsia
Unlike previous types of visual field loss, this quadrant hemianopsia is characterized by loss of the upper half of vision. Superior hemianopsia develops due to damage to the ventral part of the optic tract.
Inferior quadrant hemianopsia
Characterized by loss of lower vision on both sides. Inferoquadrant homonymous hemianopsia occurs when the posterior region of the optic tract or parietal cortex is damaged. Thus, when the parietal cortex is damaged, complete hemianopia occurs.
Clinical picture
Patients suffering from pathology often face everyday discomfort. A visual defect prevents a person from seeing objects in the lost field of vision.
For patients, ordinary events, such as crossing the road, turn into danger: a person cannot see an approaching car.
People are not recommended to drive any vehicle, as there is a risk of accidents.
Lost fields of vision do not even allow you to see the food on the other half of the plate, and difficulties arise when reading, since the other half of the page of the book is not visible. Reading turns into torture for people: people need to make more eye movements.
The neurological illness is accompanied by elementary visual hallucinations. Photopsia is the perception of non-existent ugly phenomena and objects, for example, a suddenly appearing point, flashes, lightning or lights. Often, elementary visual hallucinations with hemianopsia occur after a recent stroke.
Everyday life and basic household things cause psychological discomfort in patients: their actions from the outside seem ridiculous and sloppy.
Some patients develop depression and other neurotic disorders.
As a result of loss of visual fields and a feeling of incapacity, some patients withdraw from social life, preferring to spend time alone.
For patients with hemianopia, the range of possible specialties is limited. Thus, such patients cannot transport passengers or work in places where external assessment of objects is required, for example, in engineering or construction.
The clinical picture of visual impairment, in addition to photopsia, is supplemented by agnosia. This is a neurological disorder characterized by impaired recognition of objects in the visual channel. Patients often exhibit prosopagnosia—impaired recognition of familiar faces. Some patients experience Anton-Babinsky syndrome: people deny the presence of their pathology.
Congenital hemianopsia is often combined with developmental defects in the subcortical and cortical parts of the brain: the thalamus, brain stem and parietal cortex. Therefore, the clinical picture is supplemented by the following pathologies:
- Paresthesia is a perverted sensation. Thus, patients often suffer from tingling skin and complain of flying spots in front of their eyes.
- Violation of deep sensitivity. Patients have impaired pain and tactile perception.
Classification
According to the topic of the lesion, it happens:
- Tractus hemianopsia. Develops due to damage to the visual pathways. It is characterized by atrophy of the optic nerves, lack of pupillary response to light and asymmetry of visual field loss.
- Central hemianopsia. Develops when the central parts of the brain are damaged. The pathology is not accompanied by atrophy of the optic nerves; they continue to respond to light stimuli. The central variant is accompanied by a symmetrical loss of visual fields.
How is the disease detected?
Diagnosis of visual impairment is carried out using visual field testing. The purpose of the express method is to identify field pathologies. In neurological practice, a special hand hammer is used.
A neurologist sits down opposite a person and asks him to close one eye with his palm. The gaze of the open eye is fixed on the doctor's nose. The physician slowly moves the instrument from behind the patient's head from the periphery to the center from all sides.
The patient must be told immediately when he sees the hammer.
Among instrumental methods, perimetry has the greatest diagnostic value. The procedure is carried out using a perimeter.
As a result of the procedure, the doctor receives information about the boundaries of the visual fields for both eyes. Other visual defects are also detected. Computer campimetry is also used.
It identifies disturbances in color perception in various areas of the retina and helps determine the level of disturbance.
To identify the cause of the disorder, computer and ultrasound diagnostics are used: computer and magnetic resonance imaging, Doppler ultrasound of cerebral vessels. Computer diagnostics helps in choosing treatment tactics, as it allows you to visualize the source of hemorrhage, tumor or abscess.
Diagnostics
In order to make a correct diagnosis, the doctor pays attention to three important factors: visual field, ophthalmoscopy, visual acuity. The last two factors may not always accurately indicate the presence of hemianopia
When examining the general ophthalmological picture, the doctor does not always notice the presence of ongoing pathological changes.
As a rule, at the very beginning of its development, the pathology does not affect the fundus of the eye. Destructive changes can appear after a long time (years).
However, in the absence of treatment, when the pathology has developed into a late stage, visual acuity is significantly lost. This occurs due to secondary atrophy in which most of the optic nerve is affected.
Examination of the state of the visual fields is the most important symptom on the basis of which a correct diagnosis is made. Left- or right-sided hemianopia is determined using a simple test using a perimeter. Diagnostics occurs in this way:
The patient's head is placed on a special area (chin rest) of the device
It is important that your head is positioned at the correct angle in relation to the device. One eye is closed by the device's shutter. The second eye should focus on the bright point, which is located in the very center of the arc. The bright element moves slowly from the center of the arc to the periphery area
The patient must signal when this element disappears from the field of view.
This way, the ophthalmologist is able to identify the boundaries of the patient’s vision and correctly make a diagnosis based on simple calculations and calculations.
To make a more accurate diagnosis, modern clinics use computer perimetry, during which automated devices are used.
When the doctor has identified the presence of pathology, it is very important to determine the cause that contributed to the formation of homonymous hemianopia. For these purposes, common methods can be used, such as MRI, ultrasound of the brain, carotid angiography, radiography
Regarding the definition of benign or malignant neoplasms, various endocrine pathologies play a significant role in this. To identify them, various hormonal level tests are performed.
Functional diagnosis of lesions of the anterior segment of the visual pathway

In addition to the study of visual fields, functional electrophysiological research methods are used in clinical practice to assess lesions of the anterior segment of the visual pathway:
- electroretinography (ERG) with photostimulation
- checkerboard pattern electroretinography (P-ERG)
- visual evoked potentials (VEPs) to stimulation with a checkerboard pattern
Electroretinography (ERG) measures electrical potentials from each layer of the retina, which allows detection of retinal lesions before fundus changes occur, such as in retinitis pigmentosa. However, electroretinography (ERG) does not reveal changes caused by lesions of retinal ganglion cells and afferent parts of the visual pathway.
Visual evoked potentials (VEPs) characterize the predominant reaction of the macula, determined in the region of the occipital pole of the cerebral cortex. In the absence of retinal damage, visual evoked potentials (VEPs) make it possible to evaluate, first of all, the functioning of the segment of the visual pathway to the lateral geniculate body and especially the optic nerve.
Visual evoked potentials (VEPs) provide significant assistance in making the diagnosis of multiple sclerosis, allowing the presence of optic nerve damage to be established even in the absence of other symptoms of visual impairment.
What do you need to know about treatment?
Treatment of any form of this disease is mandatory. The fact is that if the pathology is not eliminated, it will progress quickly. This will ultimately lead to complete blindness. In any case, the treatment regimen is aimed at eliminating the source of the pathology. Sometimes this may require x-ray therapy, chemicals, or surgery.
Why does congenital horizontal nystagmus appear: symptoms and treatment
All described types of visual disorders almost never respond to conservative treatment measures. There is no need to listen to the advice of traditional healers who managed to cure someone with the help of herbs, tinctures, and other methods of influencing the eyes and nervous system. The use of so-called folk recipes for hemianopsia is absolutely meaningless, useless and harmful.
However, there are some recommendations that help the patient improve their quality of life, because using the organ of vision in such conditions is not very comfortable. You can consciously increase the size of small movements to one during the reading process. Objects should be placed at right angles and looked at diagonally. This recommendation will make reading with a loss of field of vision much easier.
Current forecast
The prognosis for a lost visual field is completely different - from its complete restoration to its loss. This depends on various factors:
- severity of pathology;
- features of therapy;
- duration of therapeutic measures;
- duration of visual defects;
- stages of the disease;
- individual characteristics of the body, because it can react differently to the course of pathological processes;
- patient's age;
- other complications that appear against the background of hemianopsia.
Prevention of visual pathology
Visual field impairment can be prevented. A person should be periodically examined by an eye doctor and a neurologist. This is especially true for people with myopia and hypermetropia. Patients at risk of developing apoplexy should be especially careful about their vision. It is necessary to undergo routine examinations to detect tumors. To prevent hemianopsia, you need to stop smoking and drinking alcohol, and you need to do gymnastics.

So, different types of this pathology, including bitemporal, lead to a noticeable deterioration in vision. If you do not pay attention to the loss of the field, it can lead to complete loss of vision. It is necessary to monitor your health and contact an ophthalmologist on time for a routine examination. This especially applies to people with cardiovascular disease or tumors.
Symptoms
The presence of the disease can be determined by the following accompanying symptoms:
- memory disorders;
- decreased mental performance;
- violation of purposefulness of movements;
- problems with recognizing objects and phenomena (agnosia);
- speech disorders;
- decreased sensitivity of the affected area of the body;
- persistent headache;
- epileptic seizures;
- fever;
- general deterioration of health;
- weakness and increased fatigue;
- arthralgia.
If the lesion affects the posterior part of the brain or other parts of it, then hemiparesis will primarily affect the limbs and facial muscles. The severity of all of the above symptoms will depend on the age of the patient. But for treatment, not only the intensity of clinical manifestations is important, but also the causes of the disease.
Symptoms of congenital hemiparesis
Congenital hemiparesis usually appears during the period when the child begins to learn to walk independently. Along with it, speech and intellectual disorders become more noticeable.
Early signs of hemiparesis in children are:
- asymmetric movements in the limbs;
- limitation of active movements on the affected side;
- asymmetric Moro reflex;
- flatness of the thigh muscles with slight but noticeable outward rotation;
- when taking a vertical position, the child does not lean on the affected leg, and when lying on his stomach, he stretches the affected arm worse and does not lean on it.
Children with congenital hemiparesis also experience numerous neurological disorders. In particular, stereognosis is impaired, and the so-called syndrome of ignoring the affected limb develops. This only makes an already difficult situation worse.
The development of epilepsy, unfortunately, is a common concomitant symptom of hemiparesis. It significantly aggravates the course of the disease and worsens the prognosis. It can manifest at any age, and taking into account this factor, the types of attacks also vary:
- in early childhood, generalized tonic-clonic and partial seizures with secondary generalization predominate;
- at a later age, partial epileptic seizures come to the fore;
- In 80% of patients with congenital hemiparesis complicated by epilepsy, simple or complex focal epileptic seizures are identified, which can sometimes have secondary generalization.
The overwhelming majority of patients with congenital hemiparesis experience rare attacks of epilepsy. Typically their frequency is once every 3, 6 or 12 months.
Hemiparesis negatively affects the cognitive abilities of the brain, and not only. Thus, with damage to the right hemisphere of the brain (with left-sided hemiparesis), there is underdevelopment of visuospatial analysis and synthesis, as well as perceptual generalizations.
With damage to the left hemisphere of the brain, which is the cause of right-sided hemiparesis, disorders of verbal functions predominate. Children with such a deviation have a poor vocabulary, a decrease in the level of verbal generalizations and the nature of judgments.
Speech disorders are recorded in 20-40% of patients with congenital hemiparesis. This defect manifests itself especially clearly in children. Most often, such disorders are expressed by delayed speech development, dysphagia or dysarthria. They are observed in both right-sided and left-sided hemiparesis.
With the pathology in question, visual deviations may also occur. Thus, the frequency of disturbances in the functioning of the visual analyzer is 30%. Homonymous hemianopsia is diagnosed in 17-27% of patients. In 8.6% of cases, partial atrophy of the optic nerves is recorded, and in 10.5% of patients strabismus is detected.
Possible complications
The occurrence of complications is associated with the serious consequences of the lack of treatment or its insufficient effectiveness. In this case, the disease is likely to progress and capture increasingly larger areas of the visual field, up to complete blindness. In addition, optic nerve atrophy develops over time, which is almost impossible to stop.
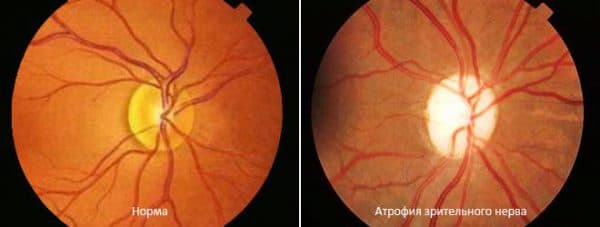
Optic nerve atrophy as a complication of hemianopia
In addition, diseases that are prerequisites for the development of hemianopsia can also cause complications, especially if they are associated with serious disorders of the choroid of the eye and brain.
Even symptomatic treatment can have a positive effect on the quality of vision. However, to completely get rid of the disease, therapy must be comprehensive.
Causes and mechanism of visual field loss
The disease can occur against the background of damage to the visual tracts, as well as the central parts of the visual tracts and areas of the cerebral cortex.
This is due to various reasons. Most often, the disease develops due to previously acquired pathologies. For example, with meningitis, compression occurs in areas that provide the conduction of nerve impulses to the cerebral cortex.
Pathology can also develop with various injuries and neoplasms in the brain. Another factor that provokes loss of visual fields is a violation of the blood circulation in the brain due to thromboembolism or aneurysm of the cerebral vessels.
The performance of the visual pathways may be impaired due to increased pressure and increased circulating blood volume. Eventually they may atrophy altogether.
If we talk about congenital blindness, then the cause of the disease lies in developmental defects, namely hydrocephalus, microcephaly, etc.
Consequence of neurological disorders
The disease most often develops as a result of damage to areas of the brain, as well as various neurological diseases.
In order to find out the cause, as well as determine the location of the lesion, a study is carried out - MRI of the brain. Depending on the type and nature of brain damage, various types of hemianopia develop:
- Homonymous hemianopsia develops due to circulatory disorders and damage to the cells of the hemispheres to which the posterior cerebral artery goes; it is often diagnosed with ischemic and hemorrhagic stroke.
- Upper quadrant hemiopia occurs when the area of the cerebral cortex located below the calcarine sulcus in the temporo-occipital region is affected.
- The cause of the appearance of the inferior quadrant form of the disease is damage to the area of the cerebral cortex located above the calcarine sulcus.
- More serious pathologies develop against the background of damage to the occipital lobes on both sides. As a result, visual hallucinations may even develop; the patient will not be able to distinguish colors and will no longer recognize familiar people.
Sometimes a homonymous form of the disorder develops against the background of a heart attack that occurs in the areas to which the posterior cerebral artery goes.
Its boundaries with the middle cerebral artery can fluctuate. Often the Sylvian fissure acts as such a conventional boundary. However, in some cases, the blood supply to the outer parts of the occipital lobe occurs through the middle cerebral artery.
Without giving specific examples, it is difficult to explain what patients experience when this pathology appears. Thus, patients diagnosed with right homonymous hemianopsia will complain that they are unable to see only with their right eye. However, upon examination, it is revealed that the person cannot see the right part of the visual field with the right and left eyes.
Prevention
There is no specific prevention of hemianopsia in adults and children. You can prevent the occurrence of a visual defect if you follow the following recommendations:
- avoid head injuries;
- avoid excessive visual strain;
- monitor the condition of the circulatory system;
- avoid intoxication of the body.
Hemianopsia often occurs against the background of other diseases. Therefore, it is necessary to regularly undergo preventive medical examinations and promptly treat detected diseases.
If the first signs of a visual defect occur, you should consult a doctor as soon as possible.
Author of the article: Kvasha Anastasia Pavlovna, specialist for the website glazalik.ru Share your experience and opinion in the comments.
Classification
The disease is divided into several types depending on the causes and specifics of its course.
Homonymous
Homonymous hemianopsia is a pathology accompanied by loss of ½ of the visual field. A person can only see the left or right side of the image. The boundary between the visible and the dropped out area passes through the central meridian. The illness may be:
- Right-handed. The left side of the optic tract is damaged;
- Left-side homonymous hemianopsia is accompanied by disruption of the activity of the right region of the tract.
The anomaly also has an additional classification, depending on the affected area:
- Full. The “blind spot” occupies ½ of the visual field, reaching the peripheral areas;
- Square. Pathology affects only the upper or lower quarter;
- Partial. The “blackout” affects a more localized part of the visual field.
| The disease can be congenital or acquired. If the disorder is concentrated in the occipital part of the cerebral cortex, the pathological process is called contralateral homonymous hemianopsia. |
The development of the disease can be triggered by a stroke, skull injury, gunshot wound, malignant or benign tumor. All these factors cause inflammation in the nerve endings, the fibers are compressed, and the blood circulation process is disrupted. If this condition persists for a long time, the optic tract atrophies.
Heteronymous
The temporal and nasal areas fall out of sight. The grant between the visible and the “blind” zone runs along the central horizontal parallel. Has the same classification as homonymous hemianopia.
Bitemporal
With the development of this pathology, the temporal areas of the visual field fall out simultaneously in the left and right eyes. It develops when the pituitary gland (the place where the optical fibers meet) or the chiasm (in the medial part) is damaged.
The location of the “blind spot” depends on which side the destructive focus is pressing on the chiasm:
- Upper. Most often, such an anomaly is diagnosed when the walls of the anterior arteries protrude;
- Lower. The reason for the appearance lies in endosellar tumors, which are characterized by an increase in the lumen of the sella turcica;
- Internal pressure. Occurs when a chiasm glioma ruptures;
- Back pressure. Associated with neoplasms on the pituitary stalk;
- Front. A similar pathology develops when a tumor occurs in the main sinus.
Causes
Impaired blood circulation in the brain leads to the development of a pathological condition. This occurs due to a malignant or benign neoplasm, head injury, or cerebral hemorrhage.
Less common causes of the disease include:
- infections;
- seizures or migraines;
- exposure to toxins;
- neurodegenerative disorders;
- non-ketotic hyperglycemia.
Common causes include stroke, tumors or complications from surgery. Also associated with high blood pressure or epileptic seizures.
The disease is caused by aneurysms. In most cases, the cause is a consequence of organic damage to the nerves of the optic pathway.