Clinical picture
The following symptoms of the disease are observed:
- weakness or complete numbness of the left or right half of the body;
- severe migraine;
- difficulty in orientation in space and time;
- increased drowsiness;
- nausea, gag reflexes, dizziness;
- deterioration in the functioning of receptors in the arms and legs;
- difficulty speaking;
- mild stupor;
- unsteadiness.
During an attack, a person begins to turn pale and blood pressure decreases. If a cerebral infarction occurs in the brainstem itself, a rapid increase in blood pressure is rarely observed. The pulse quickens, but becomes weaker.
With repeated heart attacks, the patient's mental state may be disrupted. Symptoms of asthenia can often be observed even after normalization of the mental state.
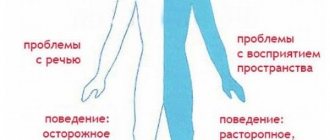
How to recognize an attack? The clinical symptoms of the disease directly depend on which hemisphere is affected. The right hemisphere is responsible for the left side of the body, and the left hemisphere is responsible for the right. The right hemisphere is responsible for creative skills and allows a person to navigate in space. Thanks to the work of the left hemisphere, a person learns to write, read and speak.
Left-sided stroke is diagnosed more often in medical practice. With lesions in the basin of the left middle cerebral artery, focal signs prevail over cerebral ones. With thrombosis in the basin of the left middle cerebral artery, hemiparesis, opticopyramidal syndrome develops, and the sensitivity of the right side is also impaired.
Severe dizziness due to cerebral infarction
The following sensations are warning signs of an attack:
- severe dizziness;
- darkening of the eyes;
- numbness in the limbs;
- short-term speech impairment.
The atherothrombotic type of lesion causes epileptic attacks, problems with urination, asthenia and memory impairment. In severe cases, coma is possible. Rapid development is characteristic of the hemorrhagic type. Hemorrhagic cerebral infarction manifests itself in the form of hoarse breathing, migraines, facial flushing, decreased body temperature, dilated pupils, partial paralysis of the limbs, and numbness of the facial muscles. In severe cases, the patient experiences deafness, blindness and memory loss.
Venous thrombosis of the cerebral arteries can be recognized by general cerebral symptoms:
- loss of consciousness;
- convulsions;
- headache,
- disorientation in space;
- nausea and vomiting.
Thrombosis of the cerebral arteries may cause nausea and vomiting
Cerebellar stroke
Deputy chief physician for medical work, kmn, neurologist Neurologist, highest category Maltseva Marina Arnoldovna Neurologist of the highest category, specialist in the field of extrapyramidal pathologies, doctor of the highest category Shabunina Ekaterina Mikhailovna Neurologist, category 2
Cerebellar stroke is one of the rarest types of ischemic stroke. It has been studied very little, so doctors experience great difficulty in making a correct diagnosis. It is also considered one of the most dangerous, since the lesion can be located very close to the trunk and other vital nerve centers of the human brain.
A cerebellar stroke may appear as a ruptured blood vessel or tissue death (necrosis). The mechanism of development is very similar to other types of intracerebral strokes. Thus, the causes of occurrence and subsequent symptoms may be identical.
People over the age of 40 most often suffer from cerebellar stroke, and the highest percentage of damage is observed in men. Medical statistics indicate a high mortality rate among victims.
However, a favorable outcome is still possible if first aid to the victim was provided on time.
Causes of cerebellar stroke
- Blockage of a blood vessel by a thrombus or embolus;
- Rupture of the vessel wall, resulting in hemorrhage and hematoma formation.
- Dissection of a section of the vertebral artery. A very rare phenomenon, due to which a cerebellar stroke is possible in young people.
Impaired blood flow in the cerebellum due to thrombosis is most often observed in patients suffering from other blood pathologies, atherosclerosis. Patients who have recently suffered a myocardial infarction are often at high risk.
Thus, blood clots can travel through the bloodstream from the heart into the cerebral arteries.
Hemorrhage in the tissues of the cerebellum is no less dangerous, and it is this that often causes the death of the victim. Blood permeating the brain tissue increases the volume of the hematoma. There is strong pressure on the cerebellar parenchyma, which in turn compresses and displaces the tissue of the brain stem. This is what can lead to sudden death of the patient.
Risk factors leading to cerebellar stroke
- High blood pressure;
- Diabetes;
- Sedentary lifestyle;
- Abuse of smoking, alcohol, drugs;
- Congenital pathology of blood vessels;
- Age;
- Diseases of the cardiovascular system, tendency to thrombosis;
- Metabolic disorders, etc.
Types and symptoms of cerebellar stroke
There are two types of cerebellar stroke: isolated in a certain area and extensive.
Symptoms of isolated cerebellar stroke:
- Disorders of the vestibular apparatus, gait, fine motor skills of the hands;
- Impaired speech and hearing, the victim is unable to pronounce words or make sounds;
- Severe dizziness and nausea;
- Acute pain in the occipital region;
- Coordination of movements and sense of balance are impaired.
Symptoms of extensive cerebellar stroke:
- Acute headache, vomiting and nausea (general cerebral symptoms);
- Coordination of movements and hand motor skills are impaired;
- The patient's speech suffers;
- The patient is unable to maintain balance;
- Respiratory and cardiac functions are impaired;
- The patient is unable to control the functioning of the tongue and make swallowing movements.
If the affected areas occupy more than a third of the volume of both hemispheres of the cerebellum, then such a stroke leads to acute hydrocephalus, which is caused by severe swelling of the damaged tissues. Strong pressure on the brain stem inevitably leads to the death of the victim. This form of stroke requires urgent surgical intervention.
Treatment of cerebellar stroke involves taking the necessary measures as in the treatment of other types of disease. If it is necessary to maintain breathing, then artificial ventilation is performed. Antihypertensive therapy is prescribed for hypertensive patients.
For low blood pressure, infusion therapy is used. High fever and aches are eliminated with analgesics and antipyretics. Diuretics relieve cerebral edema.
In addition to drug therapy, appropriate care for the patient is organized, including nutrition and prevention of bedsores.
Clinical Brain Institute articles on social networks
Other related articles:
- Residual effects of stroke
- Left-sided ischemic stroke
- Acute ischemic stroke
- Lacunar stroke
- Frontal stroke
- Middle cerebral artery stroke
- Stroke due to hypertension
- Stroke and alcohol use
- Incontinence as a consequence of stroke
- Speech impairment after stroke
Source: //www.neuro-ural.ru/patient/dictonary/ru/i/insult-mozzhechka.html
Classification of violation
The following subtypes of cerebral infarction are distinguished by etiopathogenetic subtypes:
- atherothrombotic;
- cardioembolic;
- lacunar;
- hemodynamic;
- hemorheological.
The disease can be localized in the following areas:
- internal carotid artery;
- frontal cerebral artery;
- middle cerebral artery;
- vertebral artery;
- basilar artery;
- cerebellum;
- Thalamus region;
- posterior cerebral artery.
Clinical syndromes of lacunar disease
Clinical manifestations observed during the development of lacunae are referred to as lacunar syndromes. Lacunar cerebral infarction is often accompanied by lacunar transient ischemic attacks (TIA, micro-strokes). Transient ischemic attacks (TIA, micro-strokes) can occur in the patient several times a day and last only a few minutes.
The development of cerebral infarction (ischemic stroke) may be accompanied by a sudden onset or increasing neurological deficit over several days. A few hours or days after the development of a cerebral infarction (ischemic stroke), the patient's condition improves, although some patients become disabled. The patient's recovery may be complete over a period of several weeks to months, or there may be minimal residual neurological deficit.
Neurological manifestations of many lacunar syndromes are known. Some of these neurological syndromes require confirmation. The most common neurological syndromes with lacunar disease are:
- Pure motor hemiparesis with an infarction in the area of the posterior thigh of the internal capsule or the base of the bridge. The face, arm, leg, foot and fingers are almost always involved. Muscle weakness can be intermittent during a transient ischemic attack (TIA, microstroke), gradually increasing or sudden. Muscle weakness can progress to paralysis (plegia) and then often regress. In many cases of such syndromes, recovery is complete;
- Syndromes with purely sensory disorders of the hemitype in thalamic infarctions;
- True ataxic hemiparesis due to infarction at the base of the pons and dysarthria with awkwardness in the hand or arm due to infarction at the base of the pons or knee of the internal capsule;
- Pure motor hemiparesis with “motor aphasia”, caused by thrombotic blockage of the lenticulostriate branch of the artery of the lentiform nucleus and striatum, supplying blood to the knee and anterior thigh of the internal capsule with the adjacent white matter of the corona radiata.
Before treatment for arterial hypertension, multiple lacunae often cause patients to develop pseudobulbar palsy with emotional lability, a state of lethargy, abulia and bilateral pyramidal symptoms. Currently, this syndrome is rare.
There are other lacunar syndromes that have been associated with observed arterial pathology:
- Pseudobulbar syndrome with loss of the ability to form speech sounds (anarthria), caused by bilateral infarctions in the area of the internal capsule, can develop with damage to the lenticular nucleus and striatum.
- Syndromes caused by narrowing of the lumen (occlusion) of the penetrating branches of the underlying portion of the posterior cerebral artery (listed above).
- Syndromes observed with possible narrowing of the lumen (occlusion) of penetrating arteries emanating from the main artery. These lacunar syndromes include ipsilateral ataxia and paresis of the lower extremity, pure motor hemiparesis with horizontal gaze palsy, and hemiparesis with crossed abducens (VI cranial) nerve palsy.
- Downstream basilar artery syndromes include sudden nuclear ophthalmoplegia, horizontal gaze palsy, and appendicular cerebellar ataxia.
- Syndromes that develop with possible narrowing of the lumen (occlusion) of the branches of the vertebral artery include pure motor hemiparesis (while the facial muscles remain intact) due to the involvement of the pyramid of the medulla oblongata, as well as the syndrome of damage to the lateral parts of the pons and medulla oblongata, accompanied by dizziness, vomiting, weakness facial muscles, Horner's syndrome, ipsilateral numbness in the area of innervation of the trigeminal nerve and contralateral loss of sensitivity due to damage to the spinothalamic tract (partial lateral medulla oblongata syndrome).
Negative consequences
What are the dangers of an attack and the consequences of the disease? Cerebral stroke does not go away without leaving a trace. Untimely medical care or self-medication can cause severe complications or death of the patient. After a heart attack, the patient may experience complications such as:
- paralysis of limbs;
- loss of pain sensitivity;
- lack of coordination;
- blindness;
- epilepsy attacks;
- cognitive disorders.
Most often, people who have suffered a cerebral attack experience problems with speech function. This manifests itself in incoherent and difficult pronunciation. The most dangerous complication is cerebral edema. After an attack, the patient is prescribed bed rest. The consequence of a horizontal position is congestive pneumonia.
It develops as a result of poor ventilation of the lungs. This complication appears within a month. Prolonged horizontal position leads to the formation of bedsores. If you don't take action, bedsores turn into a huge wound. An equally dangerous complication is pulmonary embolism and acute heart failure.
Scheme of pulmonary embolism
Nutrition and diet after a heart attack
The successful course of the rehabilitation period and minimizing the risk of a second heart attack, which often leads to death, largely depend on proper nutrition. The menu after a heart attack is very strict, high demands are placed on it.
The diet should be aimed at:
- accelerating regeneration processes in the area of necrosis, restoring the functioning of the heart muscle;
- maintaining weight within physiological limits;
- weight loss in obesity;
- normalization of the digestive process, since it can be disrupted during bed rest;
- stabilization of cholesterol and glucose levels in the blood.
Treatment of cerebral infarction
Features of the course of the disease and the outcome of the attack directly depend on the provision of first aid and further intensive care. In case of cerebral stroke, mandatory hospitalization in the intensive care unit is indicated. Timely treatment and rehabilitation of the patient increases the chances of a favorable outcome. Diagnosis of the disease is carried out using tomography, which allows you to determine the extent of the lesion.
The disease must be treated in stages. There are 4 stages:
- Prehospital.
- Hospital.
- Restorative.
- Rehabilitation.
Artificial respiration and chest compressions
Ischemic stroke is treated in the clinic. The patient is prescribed basic and specific treatment. The basic type of therapy is aimed at restoring the breathing process, water-electrolyte balance, accelerating blood flow and reducing swelling. It includes monitoring body temperature, measures to prevent complications and bedsores.
Specific treatment depends on the type of stroke and the precipitating factor. The patient is prescribed thrombolytic drugs:
- anticoagulant;
- platelet aggregation inhibitors;
- defibrinizing enzymes;
- neuroprotectors.
Thrombolytic therapy dissolves blood clots, restores the vascular bed and normalizes blood flow to the brain. Anticoagulants (Heparin, Daltoparin) are aimed at preventing the formation of a blood clot. Taking anticoagulants is contraindicated in persons with gastric ulcers, renal or liver failure.
Drug Glycine
Diagnosis and treatment of the disease
First of all, tests are carried out to identify the disease. In this case, arterial hypertension is immediately detected. After an attack, all symptoms may worsen over the next few days, often this time is limited to hours. That is why the patient is under the supervision of specialists all this time.
If the disease was detected as early as possible, then proper treatment will have an effect and within a period of up to 6 months, the patient will return all motor and other functions. CT and MRI are used to diagnose pathology. First of all, treatment is aimed at reducing blood pressure to normal and improving blood circulation.
When treating lacunar stroke, specialists use basic therapy. Differentiated treatment is not used, since there is no need for it. The principles of treatment are as follows:
- metabolic and neuroprotective drugs are used;
- during treatment the goal is to improve blood circulation;
- in addition, adequate therapy is used for the underlying disease affecting the blood vessels, that is, the symptoms of vasculitis, diabetes mellitus, hypertension and atherosclerosis are eliminated.
Recovery period
If the lesion is localized in the cerebellum, then rehabilitation is carried out through an individual complex of kinesitherapy, balance training and therapeutic massage. The recovery period for patients with astheno-depressive disorders includes therapeutic exercises and individual sessions with a psychotherapist.
Rehabilitation of elderly patients includes therapeutic exercises, a course of neurotrophic drugs and vitamins is prescribed. To restore the functions of the facial muscles and tongue, you can seek help from a speech therapist. Patients with impaired swallowing are initially fed through a tube. To make chewing and swallowing food easier, doctors prescribe a special diet.
During rehabilitation, you should give up smoking and alcoholic beverages
During the recovery period after an ischemic stroke, it is necessary to exclude irritating factors that negatively affect the vascular system and can provoke a relapse. Therefore, during the rehabilitation period you need to:
- stop smoking and drinking alcohol;
- control blood cholesterol levels;
- control blood pressure.
High cholesterol in the blood causes blockage of the coronary or carotid artery. To maintain normal cholesterol levels, the patient is prescribed a specially designed diet and medications. Persons suffering from arterial hypertension during the rehabilitation period are prescribed medications that maintain heart pressure at a level not higher than 140/90 mmHg.
Originally posted 2014-09-27 08:37:08.
The ability to maintain the same lifestyle after a cerebral infarction largely depends on timely and high-quality rehabilitation procedures.
In order to be able to return to your previous life as soon as possible, it is recommended to undergo rehabilitation in special centers where comprehensive measures are used to facilitate the treatment of strokes.
Basically, such processes are very long-lasting, but all cases of the disease are individual in nature, so the condition of some patients returns to normal later, and others faster.
Today there are a sufficient number of developed methods for restoring the functionality of the nervous system after illnesses. Specially designed therapeutic and physical training complexes have the greatest effect on the condition of patients.
The procedures help restore strength and motor functions of the affected side of the body within three months. Social and mental adaptation processes take much longer.
Cerebellar stroke - what is it - Nerves
A. Olesya Valerievna, Candidate of Medical Sciences, practicing physician, teacher at a medical university
Cerebellar stroke is less common than other forms of cerebrovascular pathology, but represents a significant problem due to insufficient knowledge and diagnostic difficulties. The proximity of the brain stem and vital nerve centers makes this localization of strokes very dangerous and requires quick, qualified help.
Acute circulatory disorders in the cerebellum are infarctions (necrosis) or hemorrhages, which have similar development mechanisms to other forms of intracerebral strokes, so the risk factors and main causes will be the same. The pathology occurs in middle-aged and elderly people, and is more often found among men.
Cerebellar infarction accounts for about 1.5% of all intracerebral necrosis, while hemorrhages account for a tenth of all hematomas. Among strokes of cerebellar localization, approximately three-quarters of them are infarctions. The mortality rate is high and in other cases exceeds 30%.
Causes of cerebellar stroke and its types
The cerebellum, as one of the parts of the brain, needs good blood flow, which is provided by the vertebral arteries and their branches. The functions of this part of the nervous system are reduced to coordination of movements, ensuring fine motor skills, balance, the ability to write and correct orientation in space.
In the cerebellum it is possible:
- Heart attack (necrosis);
- Hemorrhage (hematoma formation).
Disruption of blood flow through the vessels of the cerebellum leads to either their blockage, which happens much more often, or rupture, in which case the result will be a hematoma. The peculiarities of the latter are not considered to be the saturation of nervous tissue with blood, but an increase in the volume of convolutions that push apart the cerebellar parenchyma.
However, one should not think that such a development of events is less dangerous than brain hematomas that destroy an entire area. It must be remembered that even if some neurons are preserved, an increase in the volume of tissue in the posterior cranial fossa can lead to death due to compression of the brain stem.
Often it is this mechanism that becomes decisive in the prognosis and outcome of the disease.
Ischemic cerebellar stroke, or infarction , occurs due to thrombosis or embolism of the vessels supplying the organ. Embolism is most common in patients suffering from cardiac pathology.
Thus, there is a high risk of blockage of the cerebellar arteries by thromboembolism during atrial fibrillation, recent or acute myocardial infarction.
Intracardiac thrombi with arterial blood flow enter the brain vessels and cause their blockage.
Thrombosis of the cerebellar arteries is most often associated with atherosclerosis, when there is a proliferation of fatty deposits with a high probability of plaque rupture. With arterial hypertension during a crisis, so-called fibrinoid necrosis of the arterial walls is possible, which is also fraught with thrombosis.
Hemorrhage into the cerebellum, although less common than a heart attack, causes more problems due to tissue displacement and compression of surrounding structures by excess blood. Typically, hematomas occur due to arterial hypertension, when, against the background of high pressure numbers, the vessel “bursts” and blood rushes into the cerebellar parenchyma.
Other causes include arteriovenous malformations and aneurysms that form during fetal development and remain undetected for a long time because they are asymptomatic. There have been cases of cerebellar stroke in younger patients associated with dissection of a portion of the vertebral artery.
The main risk factors for cerebellar strokes have been identified:
- Diabetes;
- Arterial hypertension;
- Lipid disorders;
- Old age and male gender;
- Physical inactivity, obesity, metabolic disorders;
- Congenital pathology of vascular walls;
- Vasculitis;
- Pathology of hemostasis;
- Heart diseases with a high risk of thrombosis (heart attack, endocarditis, prosthetic valve).
How does a cerebellar stroke manifest?
Manifestations of a cerebellar stroke depend on its scale, so the clinic distinguishes:
- Major stroke;
- Isolated in the area of a specific artery.
Isolated cerebellar stroke
An isolated stroke of the cerebellar hemisphere, when the blood supply from the posterior inferior cerebellar artery is affected, is manifested by a complex of vestibular disorders, the most common of which is dizziness. In addition, patients experience pain in the occipital region, complain of nausea and gait disturbances, and speech suffers.
Heart attacks in the area of the anterior inferior cerebellar artery are also accompanied by disorders of coordination and gait, fine motor skills, and speech, but hearing impairment appears among the symptoms. With damage to the right hemisphere of the cerebellum, hearing is impaired on the right, with left-sided localization - on the left.
If the superior cerebellar artery is affected, then the symptoms will be dominated by coordination disorders, the patient has difficulty maintaining balance and performing precise targeted movements, the gait changes, dizziness and nausea bother him, and difficulties arise in pronouncing sounds and words.
When the focus of damage to the nervous tissue is large, the vivid symptoms of coordination and motor disorders immediately prompt the doctor to think about a cerebellar stroke, but it happens that the patient is only bothered by dizziness, and then the diagnosis includes labyrinthitis or other diseases of the vestibular apparatus of the inner ear, which means the correct treatment will not be started on time. With very small lesions, there may be no clinical necrosis at all, since the functions of the organ are quickly restored, but about a quarter of cases of extensive heart attacks are preceded by transient changes or “small” strokes.
Extensive cerebellar stroke
A major stroke affecting the right or left hemisphere is considered an extremely serious pathology with a high risk of death.
It is observed in the area of blood supply to the superior cerebellar artery or posterior inferior when the lumen of the vertebral artery is closed.
Since the cerebellum is equipped with a good network of collaterals, and all three of its main arteries are interconnected, cerebellar symptoms almost never occur in isolation, and brain stem and cerebral symptoms are added to them.
An extensive cerebellar stroke is accompanied by an acute onset with general cerebral symptoms (headache, nausea, vomiting), disorders of coordination and motor skills, speech, balance, and in some cases, breathing and cardiac activity and swallowing disorders occur due to damage to the brain stem.
If a third or more of the volume of the cerebellar hemispheres is damaged, the course of the stroke can become malignant, which is caused by severe swelling of the necrosis zone.
The increased volume of tissue in the posterior cranial fossa leads to compression of the cerebrospinal fluid circulation pathways, acute hydrocephalus occurs, and then compression of the brain stem and death of the patient.
The probability of death reaches 80% with conservative therapy, so this form of stroke requires emergency neurosurgery, but even in this case, a third of patients die.
It often happens that after a short-term improvement, the patient’s condition becomes severe again, focal and cerebral symptoms increase, body temperature rises, and coma is possible, which is associated with an increase in the focus of necrosis of cerebellar tissue and involvement of brain stem structures. The prognosis is unfavorable even with surgical assistance.
Treatment and consequences of cerebellar stroke
Treatment of cerebellar stroke involves general measures and targeted therapy for ischemic or hemorrhagic types of damage.
Common activities include:
- Maintaining breathing and, if necessary, artificial ventilation;
- Antihypertensive therapy with beta-blockers (labetalol, propranolol), ACE inhibitors (captopril, enalapril) is indicated for hypertensive patients; the recommended blood pressure is 180/100 mm Hg. Art., since a decrease in pressure can cause a deficiency of blood flow in the brain;
- Hypotonic patients need infusion therapy (sodium chloride solution, albumin, etc.), it is possible to administer vasopressor drugs - dopamine, mesaton, norepinephrine;
- For fever, paracetamol, diclofenac, magnesium are indicated;
- To combat cerebral edema, diuretics are needed - mannitol, furosemide, glycerol;
- Anticonvulsant therapy includes Relanium, sodium hydroxybutyrate, in case of ineffectiveness of which the anesthesiologist is forced to put the patient under anesthesia with nitrous oxide; sometimes the administration of muscle relaxants is required for severe and prolonged convulsive syndrome;
- Psychomotor agitation requires the prescription of Relanium, fentanyl, droperidol (especially if the patient needs to be transported).
Simultaneously with drug therapy, nutrition is being established, which in the case of severe strokes is more advisable to be administered through a tube, which allows not only to provide the patient with the necessary nutrients, but also to avoid food getting into the respiratory tract. If there is a risk of infectious complications, antibiotics are indicated. The clinic staff monitors the condition of the skin and prevents the occurrence of bedsores.
Specific therapy for ischemic strokes is aimed at restoring blood flow with the help of anticoagulants, thrombolytics and surgical removal of blood clots from the artery.
For thrombolysis, urokinase, alteplase are used, among the antiplatelet agents the most popular are acetylsalicylic acid (thromboASS, cardiomagnyl), the anticoagulants used are fraxiparin, heparin, sulodexide.
In case of hemorrhages, the drugs listed above cannot be administered, since they will only increase the bleeding, and specific therapy involves maintaining acceptable blood pressure numbers and prescribing neuroprotective therapy.
It is difficult to imagine stroke treatment without neuroprotective and vascular components. Patients are prescribed nootropil, Cavinton, cinnarizine, aminophylline, cerebrolysin, glycine, emoxypine and many other drugs, and B vitamins are indicated.
Issues of surgical treatment and its effectiveness continue to be discussed. There is no doubt that decompression is necessary when there is a threat of dislocation syndrome with compression of the brain stem.
In case of extensive necrosis, trephination and removal of necrotic masses from the posterior cranial fossa are performed; in case of hematomas, blood clots are removed both during open operations and through endoscopic techniques; it is also possible to drain the ventricles if blood accumulates in them.
To remove blood clots from the vessels, intra-arterial interventions are performed, and to ensure further blood flow, stenting is performed.
Recovery after a cerebellar stroke should begin as early as possible, that is, when the patient’s condition stabilizes, there is no longer a threat of cerebral edema and repeated necrosis.
It includes medication, physiotherapeutic procedures, massage, and special exercises.
In many cases, patients need the help of a psychologist or psychotherapist; the support of family and loved ones is important.
The recovery period requires diligence, patience and effort, because it can last for months and years, but some patients manage to regain lost abilities even after several years. To train fine motor skills, exercises such as tying a lace, threading a knot, spinning small balls with your fingers, crocheting or knitting can be useful.
The consequences of cerebellar strokes are very serious. In the first week after a stroke, there is a high probability of brain swelling and dislocation of its parts, which most often causes early death and determines a poor prognosis. In the first month, complications include pulmonary embolism, pneumonia, and cardiac pathology.
If it is possible to avoid the most dangerous consequences in the acute phase of a stroke, then most patients then face problems such as persistent loss of coordination, paresis, paralysis, and speech disorders that can persist for years. In rare cases, speech is still restored within several years, but motor function that was not restored in the first year of the disease will most likely not be restored.
It is good if there is an opportunity for the constant participation of competent specialists, and even better if the rehabilitation is carried out in a special center or sanatorium, where experienced personnel work and there is appropriate equipment.
Display all posts with the tag:
Source: //gbuzrk-vpb.ru/diagnostika/insult-mozzhechka-chto-eto.html
Treatment approach
Cerebral infarction is considered an emergency and always requires immediate hospitalization of the patient. Restoring the functioning of the circulatory system in the brain and preventing further possible damage to nerve fibers are the main goals of treatment in a hospital.
As soon as the condition of ischemic stroke begins to develop, patients are prescribed special drugs to help dissolve blood clots:
- Thrombolytics are very successfully used in the treatment of myocardial infarction. In addition to dissolving the resulting blood clot, these agents prevent subsequent damage to nerve tissue, significantly reducing the affected area. It should be borne in mind that such drugs can only be prescribed to a specific group of patients and are used at different stages of the development of a heart attack.
- Another group of drugs used to change the properties of blood are antiplatelet agents, which prevent the process of platelet aggregation. Antiplatelet agents are included in the list of conventional drugs to combat stroke caused by cerebral atherosclerosis or all kinds of blood infections that promote the formation of clots due to platelet aggregation. Such medications are also used to prevent recurrent strokes.
- You need to understand that the formed elements of the brain tissue begin to gradually unlock without the supply of a sufficient amount of oxygen, as well as nutrients. This process is accompanied by a whole list of various biochemical reactions, the development of which is helped by cytoprotectors or neuroprotectors. In addition, neuroprotectors help increase the activity of cells located next to already dead formed elements. Thus, neighboring cells are able to perform the functions of dead ones.
Surgical treatment methods are also used, for example, carotid endarterectomy. An action necessary to remove the inner wall near the carotid artery damaged by atherosclerotic plaque during deformation or narrowing of a blood vessel.
A similar method of intervention is also used for prevention. Existing indications and contraindications should be taken into account before making a decision and performing such operations.
Patients who have suffered a cerebral infarction at one time have a fairly high chance of recovery, as well as a full recovery.
Causes of the disease
This pathology poses a serious danger. The causes of cerebral infarction can be different:
- atherosclerosis;
- hypertension;
- obesity;
- myocardial infarction;
- cardiac ischemia;
- heart disease;
- heart failure;
- heart rhythm disturbance;
- diabetes;
- arterial hypertension;
- pathological changes (thrombosis and stenosis) of arteries;
- increased blood viscosity;
- slow blood flow;
- high cholesterol concentration;
- surgical intervention;
- frequent stress;
- excessive physical activity;
- sedentary lifestyle.
Old age, use of oral contraceptives, consumption of alcoholic beverages and smoking significantly increase the risk of developing ischemic stroke.
Set of preventive measures
Prevention of a disease must have a certain impact on the factors causing its occurrence.
Unfortunately, modern medicine specialists do not have the ability to influence every conditioning factor. First of all, it is necessary to list the circumstances that modern medicine cannot influence.
Once a person reaches age 55, the chances of having a stroke increase and double every 10 years.
A greater tendency to the disease is observed in men. All sorts of genetically determined predispositions play an important role. The remaining known causes of the disease can be controlled.
We list the main preventive measures:
- Diet. This method of prevention is primarily aimed at preventing the progression of atherosclerosis. A proper diet implies a minimum amount of foods in the diet that contain animal fats or cholesterol. It is recommended to consume a sufficient amount of fruits, vegetables, proteins and grains, as well as vegetable oil. Sea fish will be very useful, since such food contains fatty acids that prevent damage to blood vessels.
- Smoking. The likelihood of developing a cerebral infarction increases under the influence of nicotine. Blood vessels narrow and the intensity of processes that contribute to the development of atherosclerosis increases. Quitting tobacco use is considered one of the main preventive measures.
- Stress. The impact of stress on the chances of developing a stroke has long been studied and proven. You should learn to look at events happening in life more positively, avoiding the development of conflict situations. If it is not possible to deal with this problem on your own, it is better to seek help from qualified psychologists.
- Lipidemia control. Excessive amounts of fat in the blood contribute to the development of atherosclerosis and increase the likelihood of cerebral infarction by changing the composition of the blood. If an increase in cholesterol levels or any other substances that increase the likelihood of atherosclerosis is detected, it is recommended to switch to a special diet and, if necessary, undergo a course of treatment using medications that help normalize the lipid spectrum in the blood.
- Physical exercise. You need to exercise regularly. This prevents obesity and other disorders that are significant risk factors. Exercise also helps reduce the risk of blood clots. The likelihood of premature death is reduced by approximately 30% with consistent exercise.
Instrumental examination for the diagnosis of lacunar disease
Computed tomography (CT) of the brain can detect most supratentorial lacunar infarcts. Magnetic resonance imaging (MRI) of the brain clearly reveals both supra- and subtentorial infarcts (lacunae measuring 7 mm or more), as well as extension into the gray matter of the cortical surface of a small infarction in the white matter of the brain. This spread is predominantly a consequence of embolism rather than narrowing of the lumen (occlusion) of small penetrating vessels. Therefore, in such situations, a diagnosis of lacunar infarction should not be made.
Many infarctions larger than 2 cm, combined not only with pure motor hemiparesis, are incorrectly called lacunae in the literature. They are too large to represent the result of occlusion of a single penetrating branch. These are likely embolic infarcts in which brain computed tomography (CT) is unable to demonstrate cortical involvement. The diagnosis of lacunar infarction should be made only when the size of the infarction is less than 2 cm and its localization can be explained by occlusion of a small penetrating branch of one of the large arteries of the base of the brain. Larger deep infarcts in the white matter and middle cerebral artery basin are probably caused by emboli.
Electroencephalography (EEG) is usually normal, in contrast to that seen in infarcts involving the cerebral cortex. If normal results are obtained during an EEG study soon after the onset of symptoms, this gives reason to think about a deep infarction in the white matter of the cerebral hemisphere.
The prognosis depends on many factors
The prognosis for further development of the disease depends on the location and size of the affected area, as well as certain concomitant disorders and diseases. The favorable prognosis may worsen depending on the size of the damaged area and the moment the treatment procedures begin.
In severe cases, it is very difficult to restore memory, speech, and normal coordination of movements, especially when the patient suffers from a coma.
Each day of this condition reduces the possibility of recovery by approximately 15%. It should be borne in mind that about 25% of citizens who have had a heart attack die in about a month.
If a patient experiences a lacunar stroke, the chance of death is about 2%.
Factors that cause heart attack
As already mentioned, lacunar stroke or heart attack appears as a consequence of arterial hypertension affecting the brain.
It depends on what blood pressure is observed, how much the artery walls are damaged and what condition they are in. It is important to monitor the surges that occur during the day and their surges, because sudden changes or drops in pressure can cause a lacunar stroke.
Basically, the risk of getting a cerebral infarction is in people with:
- hyaline dystrophy AG;
- atherosclerosis;
- previously suffered infectious inflammation of arterioles localized in the brain;
- high blood sugar or diabetes.
In addition, a fairly common causative agent of lacunar stroke of the brain is vasculitis, which can manifest itself in a nonspecific and specific form.