What are cranial or cranial nerves?
A nerve or neuron is the basic structural and functional unit of the nervous system and facilitates communication and transmission of signals throughout the body. The brain is one of the main parts of the central nervous system, which is located inside the skull. Therefore, the nerves originating from the brain are cranial.
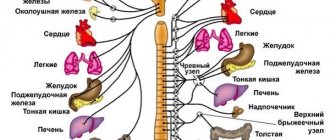
They are mainly associated with the head and neck and are involved in the transmission of sensory and motor information from the brain to the head, neck, and face. This information triggers bodily reactions, helps you “feel” certain sensations, and tells your body what to do.
Cranial nerves, 12 pairs (table, functions, characteristics are presented below) belong to the somatic nervous system.
XI, XII pairs of cranial nerves, their nuclei, topography and areas of innervation.
Accessory nerve, n. accessories (XI),
is a motor nerve that innervates the sternocleidomastoid and trapezius muscles.
It has two cores. One nucleus lies within the medulla oblongata, and the other in the spinal cord. The nerve begins with several cranial and spinal roots. The cranial roots, radices craniales,
emerge from the posterior lateral groove of the medulla oblongata,
the spinal roots, radicess pindles,
emerge from the same groove of the cervical part of the spinal cord and rise upward.
The resulting trunk of the accessory nerve is directed to the jugular foramen, where it is divided into two branches: internal and external. Internal branch, r.
internus, formed by fibers of both cranial and spinal roots, joins the trunk of the vagus nerve.
Outer branch, r.
externus, leaves the jugular foramen, goes first between the internal carotid artery and the internal jugular vein, and then, coming under the posterior belly of the digastric muscle, goes to the sternocleidomastoid muscle. Having given it part of the branches, the external branch appears at the posterior edge of this muscle and then follows to the trapezius muscle, which it also innervates.
Hypoglossal nerve, n. hypoglossus (XII),
- also motor, innervates the muscles of the tongue.
Nerve fibers emerge from the motor nucleus of the hypoglossal nerve, which is located in the medulla oblongata. The nerve emerges from the medulla oblongata through numerous roots in the groove between the pyramid and the olive. The trunk of the hypoglossal nerve is directed forward and laterally into the canal of the same name and passes through it. After leaving the canal, the hypoglossal nerve goes down and anteriorly, bending around the vagus nerve and the internal carotid artery on the lateral side. Having passed between the internal carotid artery and the internal jugular vein, the hypoglossal nerve is directed under the posterior belly of the digastric muscle and under the stylohyoid muscle and goes into the submandibular triangle. Having formed an arch, convexly facing downwards, the hypoglossal nerve follows forward and upward to the tongue, in the thickness of which it breaks up into lingual branches, rr.
linguales, innervating the muscles of the tongue.
A descending branch departs from the hypoglossal nerve, containing motor fibers attached to the first spinal nerve. This branch connects with the branches of the cervical plexus, as a result of which a cervical loop, ansacervicalis
(loop of the hypoglossal nerve), is formed anterior to the common carotid artery.
Classification
Cranial nerves supply sensory, motor and autonomic innervation to the structures of the head and neck. They are classified depending on their exit from the skull and on a functional basis.
At the exit point
All cranial nerves exit the brain, bypassing the spinal nerve. They are part of the peripheral NS, as they are directed to the cranial and cervical structures. Sensory nerves are formed from young neuronal cells, and motor nerves are formed from cells of the motor nuclei.
| Brain department | Associated cranial neuron |
| Brain | I |
| Thalamus | II |
| Midbrain | III IV V VI VII VIII (partially) |
| Medulla | VIII (partially) IX X XI XII |
After exiting, the nerves travel from their source to various parts of the body: the head, face, mouth, and some around the periphery of the body.
By function
Cranial nerves (the table characterizes 12 pairs for reference) are classified as sensory, motor, or a combination of both.
This means that the axons (neurites that carry nerve impulses) in these nerves originate from sensory ganglia (a ganglion of axons) outside the skull or motor nuclei in the brain stem. Axons with sensory functions form synaptic endings, with which they subsequently enter the stem nuclei.
| Sensory | Olfactory, visual, vestibulocochlear pair | The first 2 pairs, the olfactory and optic nerves, develop as outgrowths in the anterior medullary vesicle. These nerves do not have peripheral sensory nodes. |
| Motor | Oculomotor pair, trochlear nerve, abducens, accessory and hypoglossal nerves | Motor axons innervate the skeletal muscles of the head or neck. |
| Mixed (nerves of gill arches) | Trigeminal, facial, glossopharyngeal, vagus | The sensitive parts of the nerves of the branchial arches have nerve ganglia (ganglia), in which the organs of peripheral sensory neurons are located. |
The cranial nerve nuclei are functionally organized into distinct nuclei in the brainstem. In general, the nuclei located towards the back tend to be sensory, while the nuclei located towards the front tend to have motor functions.
Branches of the optic nerve
1. Branches of the optic nerve (n. ophthalmicus) (Fig. 523A).
Tentorial branch (r. tentorii). The thin branch begins from receptors located in the lateral and superior walls of the cavernous sinus. The branch enters the optic nerve as it exits the orbit.
Lacrimal nerve (n. lacrimalis). Forms fibers that contact the receptors of the lacrimal gland, skin and conjunctiva of the lateral corner of the eye. Parasympathetic fibers that leave the zygomatic nerve are connected to the lacrimal nerve. These postganglionic fibers arose from the pterygopalatine ganglion to innervate the secretory cells of the lacrimal gland.
Frontal nerve (n. frontalis). Formed by connecting the supraorbital, supratrochlear nerves and the frontal branch: 1) the supraorbital nerve (n. supraorbital) starts from the receptors of the skin and tissue of the frontal region, passes into the orbit through a notch or hole in the supraorbital edge of the frontal bone; 2) the supratrochlearis nerve (n. supratrochlearis) contacts the receptors of the upper eyelid, medial corner of the eye and glabella. Penetrates into the orbit near the block of the superior oblique muscle, i.e. in the medial corner of the eye; 3) the frontal branch (r. frontalis) is thin, has receptors in the skin along the midline of the forehead. The nerve passes into the orbit closer to the medial corner of the eye. All three branches join at n. frontalis at the site of attachment of the superior rectus muscle to the eyeball.
523 A. Diagram of the first branch of the trigeminal nerve. 1 - n. supratrochlearis: 2 - n. frontalis: 3 - n. lacrimalis: 4 - fissura orbitalis superior; 5 - r. meningeus; 6 - n. ophthalmicus; 7 - gangl. trigeminal; 8 - n. nasociliaris; 9 - radix oculomotoria; 10 - n. oculomotorius: 11 - gangl. ciliare; 12 - nn. ciliares breves; 13 - n. ethmoidalis posterior; 14 - n. ethmoidalis anterior; 15 - n. zygomaticus; 16 - r. communicans cum n. zygomatico; 17 - n. infratrochlearis.
The nasociliary nerve (n. nasociliaris) is formed from a number of branches: a) a long root (radix longa) - its fibers contact the receptors of the eyeball and are directed to the ciliary node (Fig. 523A); b) long ciliary nerves (nn. ciliares) start from the receptors of the eyeball, numbering 2 - 3, exit through the posterior pole of the eyeball above the exit of the optic nerve; c) the posterior ethmoid nerve (n. ethmoidalis posterior) has receptors in the mucous membrane of the sphenoid sinus, the posterior cells of the ethmoid bone. Penetrates from the nasal cavity into the orbit through the posterior ethmoidal openings; d) the anterior ethmoidal nerve (n. ethmoidalis anterior) has receptors in the mucous membrane of the frontal sinus, in the ciliary ganglion, the skin of the tip of the nose and the nasal mucosa; dendrites pass into the cranial cavity through holes in the horizontal plate of the ethmoid bone, where fibers innervating the dura mater of the anterior cranial fossa are connected to them. The anterior ethmoidal nerve then passes through the anterior ethmoidal foramen into the orbit; e) subtrochlear nerve (n. infratrochlearis) starts from the skin receptors of the upper eyelid, medial corner of the eye and nose. Penetrates into the orbit under the block of the superior oblique muscle.
The ophthalmic nerve (n. ophthalmicus) is sensitive, 2-3 mm in diameter, formed by the fusion of the lacrimal, frontal and nasociliary nerves lateral to the trochlear and abducens nerves in front of the superior orbital fissure. In the cranial cavity, the optic nerve is located in the lateral wall of the cavernous sinus together with n. trochlearis and n. abducens. Next, it enters the anterior pole gangl. n. trigemini.
What can damage each pair of nerves lead to?
Damage to cranial nerves, their tracts or nuclei leads to dysfunction:
- If the facial nerve is damaged, one side of the face will be unable to express emotions.
- The optic nerve can be damaged by skull fractures. In this case, irreversible blindness in the affected eye may develop.
- Any damage or injury to the vestibulocochlear structure can lead to hearing loss or balance problems.
- Injury to the hypoglossal nerve can cause complete paralysis of the tongue, leaving the person unable to eat or speak normally. There are many reasons that can damage the hypoglossal nerve, such as infection or nerve damage, causing the tongue to become paralyzed.
- Any dysfunction of the accessory nerve can cause the shoulders and neck to not function properly.
- Damage to the abducens nerve can result in blurred vision or double vision.
- If the vagus nerve is damaged, your resting heart rate may be around 100 beats per minute.
The cranial nerves, 12 pairs (the table is presented in the article for reference) of which are located inside the skull, when damaged, require focusing on protecting the brain. Some treatments for their conditions include surgery. Tumors are treated using radio waves.
Cranial nerves transmit information from the brain to parts of the human body, especially the head and neck, and back. Many of the 12 pairs are connected by connecting branches. The structures and connections of the human body are presented in anatomical tables and atlases, which help to better understand the functioning of the body.
Author: Belyaeva Anna
Pathologies and possible lesions
It is not difficult to guess that damage to any nerve ending is fraught with the development of serious complications that develop into chronic pathologies, the treatment of which requires special knowledge and skills, not always ending in success. To familiarize yourself with the possible consequences of such violations, it is worth studying the following auxiliary table:
| Name of the paired nerve | External symptoms and consequences |
| Facial | loss or worsening of olfactory sensitivity and hallucinations |
| Visual | partial or complete loss of function, loss of certain visual areas, scotoma formation, hallucinations |
| Oculomotor | eyelid closure, strabismus, diplopia, dilated pupils, deterioration of near function |
| Block-shaped | squint upward or inward |
| Trigeminal | decreased skin and taste sensitivity, increasing pain during inflammatory processes, atrophy or hypertonicity of the masticatory muscles, sagging jaw, problems with the respiratory system |
| Abductor | strabismus to the inside, double vision |
| Facial | unilateral facial paresis and paralysis of the limbs, increased sensitivity to sounds and tastes, dry eye syndrome due to infrequent blinking |
| Auditory | vertigo, incoordination, nausea and vomiting, tinnitus and auditory hallucinations |
| Glossopharyngeal | pain and numbness in the pharynx extending to the ear area, impaired taste sensitivity |
| Wandering | paralysis of the pharynx and certain parts of the esophagus, hoarseness, heart rhythm disturbances up to death |
| Additional | deviation of the head towards the source of nerve damage, difficulty abducting in the opposite direction when shrugging the shoulders, throwing back and lack of motor function in different directions |
| Sublingual | numbness, paralysis of the affected tongue, various speech disorders |
Neurology is one of the most complex medical fields, which continues to be intensively studied by the world's best luminaries. Knowledge in this area helps modern specialists to completely or partially eliminate various pathologies associated with the motor, sensory and mixed functions of the human body.