Tunnel neuropathy is a fairly common phenomenon. It is associated with impaired microcirculation and compression of peripheral nerves in the so-called tunnels, that is, narrow fibro-osseous canals of the upper and lower extremities.
This pathology can be caused by genetic predisposition, endocrine disorders (such as hypothyroidism and diabetes), as well as joint diseases: from rheumatoid arthritis to deforming osteoarthritis.
View gallery
Currently, there are several theories explaining the mechanism of development of tunnel neuropathy (for example, hormonal), but none of them has received final scientific confirmation, so the disease is considered multifactorial. Depending on which nerve is affected, several types of this pathology are distinguished.
Compression-ischemic: basic information
Sometimes you can come across the term “tunnel compression-ischemic neuropathies.” And this is by no means a tautology.
The term “compression-ischemic” means that a sufficiently long-term compression of the nerve occurs, accompanied by circulatory disorders, which lead to ischemia of the nerve fibers.
There are many varieties of this pathology, for example, tourniquet, tunnel, iatrogenic (postoperative) neuropathies. Tunnel diseases are classified as a separate group because they have a common symptom: local compression of the nerve occurs inside the natural canals and tunnels.
View gallery
If you look at the ICD 10 code for tunnel neuropathy, you will note that there is a clear division into mononeuropathies of the upper and lower extremities. They are assigned codes G56 and G57, respectively. The last group includes, for example, tunnel neuropathy of the peroneal nerve.
Diagnosis of such diseases is carried out using various methods. For example, ultrasound of the nerve and radiography of joint tissues are considered the most informative, although in some cases the doctor may prescribe an additional study - electromyography.
Pathogenesis of neuritis
The clinical course of neuropathies is often a chronic and long-term process, with some exceptions when pain syndromes or muscle weakness come to the fore, which significantly interfere with the patient’s quality of life. Examples of an acute process can be discogenic radiculitis, trigeminal neuritis, facial nerve neuritis, etc.
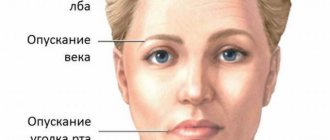
Neuritis of the facial nerve is characterized by an acute process, rapidly developing weakness of the facial muscles, which reaches a maximum within a few hours, less often - days. It is characterized by lacrimation due to weakness of the orbicularis oculi muscle, and sometimes by dry eye as a result of the lacrimal fibers being affected. Approximately 30% of patients experience painful hypersensitivity to sounds (hyperacusis), and half have impaired taste in the anterior 2/3 of the tongue on the affected side. General symptoms (fever, weakness, sweating, etc.) are not typical for neuritis of the facial nerve. In addition, this disease is not characterized by slowly increasing paresis of facial muscles (over weeks or months) - as a rule, in such cases we have to talk about a tumor etiology.
Some researchers (Lobzin V.S., 1963, 1980) regarded Bell's palsy as an acute regional ischemic disease of the facial nerve requiring emergency care. It has been shown that the use of vasodilators and decongestants during the first two days leads to a rapid cure. [7]
In the affected muscles, a change in electrical excitability develops within two weeks, the degree of which can vary, from a slight decrease to a complete reaction of degeneration. Damage to the facial nerve is usually unilateral. Bilateral lesions develop simultaneously or with an interval of 1-2 days, and are rarely observed.
Tunnel neuropathy of the ulnar nerve: causes and symptoms
The disease is one of the most common pathologies of the brachial plexus nerves. The cause is considered to be compression, that is, compression of the nerve in the specified area.
This is often due to the characteristics of professional activity, for example, if a person has to work with his elbows resting on a desk or machine for a long time. Although in some cases this form of the disease can also develop in athletes with prolonged compression of the base of the palm, as happens with cyclists. A similar picture is typical for those who work a lot with hand tools.
View gallery
The reason that the disease so often affects the ulnar nerve is its superficial location, which makes this area especially vulnerable.
Despite the name “ulnar nerve tunnel neuropathy,” signs of the disease can appear at the level of the wrist, and in the area of the ring finger and little finger.
It all starts with numbness and paresthesia. The function of the radial and median nerves is preserved. But as the disease progresses, the hand begins to resemble a clawed paw, since the main phalanges of the fingers are sharply extended, the little finger is moved to the side. Atrophy of the small muscles of the hand occurs.
NEUROPATHY OF THE EXTERNAL CUTANEOUS NERVE OF THE FEMOR (n. cutaneus femoris lateralis)
This is a sensory nerve; it is responsible for sensitivity in the area of the outer (lateral) thighs.
Neuropathy is manifested by burning persistent pain in the area of the outer surface of the thigh and a feeling of numbness, “crawling”, tingling in the same area.
These phenomena intensify when standing up and walking.
People suffering from neuropathy of the external cutaneous nerve of the thigh describe pain when standing up as a flashing, “ball of fire” in the lateral thigh area and spreading down the thigh, before reaching the knee.
The pain point for this type of neuropathy is detected under the anterosuperior iliac spine.
Pathology of the radial nerve: causes and symptoms
Tunnel neuropathy of the radial nerve is considered an equally common disease. For its symptoms to occur, sometimes it is enough just to place your hand poorly during sleep. Interestingly, this usually happens in people who fall asleep soundly after heavy physical work, or due to prolonged lack of sleep, but this situation also occurs in patients who fall asleep after alcohol intoxication.
But most often it occurs due to muscle overload and injury, and in general is a secondary pathology. This phenomenon is encountered by those who run, conduct, as well as patients who have to use crutches.
View gallery
Other factors contributing to the development of this disease are:
- humerus injuries;
- incorrect application of the tourniquet;
- bursitis, synovitis, other inflammatory diseases, including rheumatoid arthritis;
- infections (including influenza);
- intoxication;
- degenerative joint diseases - arthrosis.
Tunnel neuropathy of the radial joint is characterized by the so-called hanging hand. This means that if the arm is extended forward, the hand on the affected side will not be able to assume a horizontal position and will hang down. At the same time, the index and thumb are pressed against each other.
The patient experiences numbness and paresthesia on the back of the hand, as well as in the area of the index, thumb and middle fingers.
This type of neuropathy includes two main syndromes. This is radial tunnel syndrome, which is characterized by compression of the superficial branch of the nerve in the area of the anatomical snuffbox, as well as Turner syndrome (it is more often observed with a fracture).
Manifestations and diagnosis
Clinical manifestations depend on the location of the lesion. The main symptom defining the syndrome is pain. In this case they can arise:
- paroxysmal or shooting;
- regularly, aching type of pain;
- in the form of a burning sensation;
- as sensory disturbances (dysesthesia).
Tunnel form of neuropathy
If the nerves involved in the stimulation of muscles are pinched, then consequences such as loss of strength and muscle atrophy are possible. When veins and arteries are compressed, vascular disorders can develop. In this case, a decrease in temperature in the affected area appears, the skin becomes pale or cyanotic, and the limb swells.
To determine tunnel types of neuropathies, diagnostic tests have been developed:
- When pressing with a finger, local pain appears at the site of compression.
Diagnosis of tunnel neuropathy
When tapping (percussion) of the affected area, numbness, tingling or crawling occurs in the innervated area.
- Provocative tests. Their use allows you to accurately determine the location of compression. Pain and paresthesia intensify in the localization area.
- Injections containing lidocaine and hydrocortisone. Injected into the intended area of nerve compression. When identifying the compression zone, they help to significantly reduce pain.
- Electroneurography. This procedure allows you to determine the speed at which the impulse travels along the nerve trunk and determine the extent to which it is affected.
Based on their location, the following tunnel neuropathies are most often identified:
wrists – 45% of identified cases of pathology;
- ulnar nerve tunnel syndrome – 15%;
- peroneal nerve – 10%;
- tibial nerve - about 7%;
- in the groin area – 7%;
- brachial (radial) nerve – 4%.
It must be taken into account that in some cases, pain in the wrist or forearm can be caused by osteochondrosis, which manifests itself in the cervical region.
With this condition, it is possible that nerve roots in the spinal canal are irritated, but pain impulses are sent to other parts of the body. To identify instability of the cervical spine, it is necessary to additionally perform magnetic resonance imaging of the affected area.
Pathology of the median nerve: causes and symptoms
Tunnel neuropathy of the median nerve can be caused by a wide variety of causes. These are, for example, injuries to the upper limb or nerve damage associated with professional activities (typical for people who have a large load on their hands, resulting in constant overexertion). Also, a similar situation can be caused by incorrect injection into the antecubital vein.
View gallery
Symptoms of median nerve tunnel neuropathy include pain in the thumb, index and middle fingers. In addition, discomfort or pain of varying degrees of intensity is also felt on the inner surface of the forearm.
It becomes more and more difficult to bend the palms of the hand (during the examination, the doctor specifically asks to clench the palm into a fist to check this feature). Muscles can atrophy quite a lot over time, especially in the big toe area. If you don't do anything about it, the hand will increasingly resemble a monkey's paw.
NEUROPATHY OF THE PUDENTAL NERVE (nervus (n) pudendus) - pudendoneuropathy
The nerve provides sensitivity in the anus and perineum, is responsible for the work (innervates) the muscles of the perineum, bladder (located in the bladder) and urethral (in the urethra) sphincters (muscles responsible for holding urine).
Neuropathy is manifested by: unilateral pain in the perineal area, sometimes in its anterior parts: in women - in the vaginal area, in men - in the scrotum; sometimes in the posterior regions - in the area of the anus and rectum (anorectal), in the coccyx and buttocks.
In addition to pain, unpleasant sensations of numbness, tingling, and burning may occur in these same areas. Pain and discomfort increase when sitting and decrease when standing.
There may be short delays in urination.
Upon examination, no changes in the perineal area are detected.
Tunnel neuropathy of the peroneal nerve and its features
This is a special type of mononeuropathy. It manifests itself in the so-called foot drop syndrome, in which the patient is unable to bend the foot or straighten its toes. In addition, the skin of the anterolateral area of the leg is affected, its sensitivity decreases.
The peculiarity of this pathology, in comparison with those described above, is the following: it affects the peroneal nerve, consisting of relatively thick nerve fibers. They are distinguished by a solid layer of the myelin sheath, but it is this structure that is most susceptible to damage when metabolic processes are disrupted.
According to statistics, in only 30% of patients it is associated with primary damage to the nerve itself, and in most cases it develops during treatment after injuries and surgery.
View gallery
Of course, one should not underestimate other reasons that can lead to such a pathology. This, for example, can be various injuries (from a knee bruise to a shin fracture), vascular disorders leading to ischemia, curvature of the spine, gout, diabetes, wearing excessively tight shoes.
When a joint is injured, the nerve damage is acute and pain immediately appears. In other cases, neuropathy develops gradually, as a chronic disease, in which there is a violation of the extension of the foot, as a result, when walking, the patient is first almost imperceptibly, and then quite strongly forced to bend the affected limb at the knee joint so that the toe does not catch on the floor.
The process is accompanied by pain both in the foot itself and in the lower leg. Over time, muscles can atrophy. The patient cannot stand on his heels or walk on his toes, and this is one of the simplest ways to check which nerve is affected.
Clinical manifestations of root compression in osteochondrosis
| Spine | Spread of pain/area of sensory loss | Atrophied muscles | Decreased/active reflexes |
| L4 | Along the inner anterior thighs to the knee and sometimes below | Quadriceps femoris | Knee |
| L5 | From the lower back to the buttock >> along the outer edge of the thigh >> along the anterior outer surface of the lower leg to the 1-3 toes | Tibialis anterior muscle | — |
| S1 | From the lower back to the buttock >> along the outer back edge of the thigh >> along the outer edge of the lower leg to the 4–5 toes and heel | Triceps surae muscle | Achilles |
*The table shows the most commonly affected roots that can cause pelvic pain (the L5, S1 roots are most often affected).
In conclusion, one cannot help but mention such a pathological condition as COMPRESSION NEUROPATHY - damage to the peripheral nerves, in this case the pelvic nerves, when they are compressed, as the cause of pelvic pain.
Such compression may occur as a result of narrowing of the musculofascial and/or musculoskeletal canals in which the nerves pass. This occurs due to local proliferation of connective tissue, with prolonged monotonous overstrain of the musculo-ligamentous apparatus in athletes and/or as a result of professional activity, with soft tissue injuries and/or dislocations.
Compression syndromes are also called tunnel syndromes, when due to compression of the nerve trunk and the vessels feeding it, certain changes occur in it.
In our article we will look at damage (neuropathy) of the pudendal nerve, obturator nerve, “causalgia syndrome of the inguinal-genital zone”, lateral cutaneous nerve of the thigh and damage to the lumbosacral plexus.
Symptoms of sciatic nerve compression are discussed in piriformis syndrome (see above).
Treatment: basic principles
Treatment of tunnel neuropathies can only be effective if the cause is established and the mechanism of compression is determined. As for the methods, in this case an integrated approach to therapy is used.
Fortunately, in most cases, treatment is conservative. However, in some situations (usually very advanced), a more radical surgical intervention may be required, in which the tissue that has compressed the nerve is dissected. Typically, such an operation is prescribed in cases where conservative treatment has failed. There are practically no absolute indications for its implementation.
View gallery
As for conservative therapy, its methods partly depend on which nerve is affected. For example, if we are talking about tunnel neuropathy of the lower extremities, then treatment begins with the leg being fixed in such a position that the nerve is not compressed. For this purpose, special shoes, orthoses, and other devices are used.
Prednisolone for facial neuropathy
The rationale for using corticosteroids in the acute phase of Bell's palsy is that inflammation and swelling of the facial nerve are the main causes of Bell's palsy and corticosteroids have a powerful anti-inflammatory effect that minimizes nerve damage and thereby improves treatment outcome.
Randomized, double-blind, placebo-controlled studies have provided compelling evidence that treatment with prednisolone improves outcome in patients with Bell's palsy and reduces the time to full recovery. Prednisolone should be used in all patients with acute neuropathy of facial palsy less than 72 hours into the disease who do not have a contraindication to steroid therapy. The dose of prednisolone was 60 mg per day for 5 days and then reduced by 10 mg per day (for a total time of 10 days) or 50 mg per day (in two doses) for 10 days.
Etiotropic therapy
When considering a disease such as tunnel neuropathy, it is necessary to note the important role of etiotropic therapy, which is aimed at eliminating the cause of the pathology. For example, if we are talking about arthrosis or other degenerative joint disease, then medications containing chondroitin sulfate and glucosamine are prescribed.
In a certain sense, they have both anti-inflammatory and analgesic effects, but they work very slowly. Their effect will be noticeable only after 2-3 months of use.
The main thing that these drugs do is they help restore joint tissue, and they are prescribed precisely for this purpose. In addition, they can be taken for a long time, unlike analgesics and non-steroidal anti-inflammatory drugs. The latter relieve acute pain, but they cannot be used for a long time, this is where chondroitin sulfate with glucosamine comes in handy.
School of Practical Myology L. Rozlomiya
Obturator nerve neuropathy (femoral neuropathy) and Practical Myology.
First, it is necessary to provide materials from official medical sources in order to assess the scope and direction in the treatment of this disease. After evaluating what you have read, you can express an alternative point of view, both on the causes leading to neuropathy and on treatment.
Let's read.
“General principles of therapy for femoral neuropathy.
For femoral neuropathy that occurs as a result of the compression effect of space-occupying formations, the main method of treatment is surgery.
The development of a retroperitoneal hematoma with compression of the femoral nerve in the retroperitoneal space is an urgent situation, which usually requires emergency surgical intervention (surgical decompression or endovascular embolization). The volume and nature of the intervention are determined by the location and size of the hemorrhage, the severity of the disturbance of vital functions and the degree of damage to other organs of the retroperitoneal space [21].
The nature of the underlying disease completely determines the treatment tactics for neoplastic (tumor, neuroma) lesions of the femoral nerve. Severe traumatic (including iatrogenic, that is, associated with operations or gynecological manipulations, such as childbirth) damage to the femoral nerve with its complete anatomical break also usually makes surgical revision necessary.
For less severe traumatic lesions, compression-ischemic femoral neuropathies, treatment is conservative, which is carried out in accordance with the general principles of the treatment of peripheral neuropathies [1, 4].
When there is compression by musculo-ligamentous structures in the area of the inguinal ligament, Gunter’s canal or the patella area, injection therapy with solutions of glucocorticoids and local anesthetics is performed [22].
For paresis of the quadriceps, iliopsoas and sartorius muscles, active physical therapy is necessary to maintain range of motion in the joints and activate the affected muscles (prevention of contractures and muscle atrophy), electrical stimulation of paretic muscles and the use of drugs that improve neuromuscular transmission (neostigmine, ipidacrine and etc.).
Therapy aimed at restoring the function of the affected nerve is of great importance. For this purpose, the prescription of vasoactive (for example, aminophylline, pentoxifylline, etc.) and metabolic agents (B vitamins, thioctic acid, etc.) is justified.
A significant problem may be pain, which in case of lesions of the femoral nerve can be very intense and persistent and is predominantly neuropathic in nature. In this regard, in addition to traditional non-steroidal anti-inflammatory drugs and analgesics, anticonvulsants (gabapentin, pregabalin, topiramate) or antidepressants (amitriptyline) that are effective for relieving neuropathic pain should be used.
For incurable neuropathic pain, percutaneous stimulation of the femoral nerve has been proposed [23].
In conclusion, it should be emphasized once again that most cases of femoral neuropathy are potentially curable and, with adequate timely treatment, their prognosis is favorable.
T.V. Zimak"
Having familiarized myself with the presented material, I was surprised to not find even a hint of the muscles through which the nerves that form the obturator nerve penetrate!
PICTURE: Obturator nerves from their origins from the spinal nerves to their exit from the obturator foramen (! - applied meaning).
The rest is the same as always: either an operation, or hormonal drugs and anesthetics.
Undoubtedly, when a tumor or hematoma appears (judging by the article, it is of unknown origin), then surgery is necessary “for health reasons.” However, in all my many years of practice, I do not remember such cases.
I know that during “difficult” births, hematomas in the perineum occur, even if only from applying the same forceps to extract the fetus, but obstetricians quickly deal with them. Whereas in all other cases, the cause of neuropathy of the obturator nerve is associated with muscles - this is the lumbar part of the iliopsoas muscle group and the obturator muscles themselves (internal and external).
PICTURE: Obturator externus and obturator internus muscles.
The functions of these muscles are to rotate the thigh outward (! - applied meaning) (“Anatomy” according to Sinelnikov). Here it would be appropriate to also remind you about the twin muscles, with similar functions, which no one except myologists talks about. And in vain, since Practical Myology associates the occurrence of a number of pathological symptoms (including pain) and conditions with them, which has been proven by practice. They even had to create a special apparatus (as an aid to myologists) so that they could be reached through the thickness of the gluteal muscles.
The antagonists of these muscles are the semitendinosus and semimembranosus muscles, the tensor fasciae lata, the pectineus muscle, as well as the anterior fibers of the gluteus medius and minimus muscles, which internally rotate the thigh (! - applied meaning) .
I list the functions of the hip rotators here specifically to remind my fellow myologists of the great importance of their relationship with each other.
Violation of parity between these muscles leads to the emergence of combined pathologies that cannot be solved either by hormone therapy or operations to (allegedly) remove spinal hernias (mythical in their attributed properties). Only the techniques of Practical Myology can help in diagnosing neuropathy of the obturator nerve through specific palpation of the muscles involved, and in completely curing the patient.
You can read about clinical symptoms in the area of the obturator foramen in anatomical reference books, but in this material not a word is written about the signs (symptoms) of an impending disease. While the main ones are internal rotation (! - applied meaning) (more often) of one or both limbs (which happens rarely).
Women experience discomfort (including pain) during sexual intercourse.
Here is a picture of the female pelvis, where the area of the obturator foramen is colored blue with a hint that the muscles located in it are reachable.
IMAGE: Female pelvis.
Constant symptoms include the inability to sit and stand for a long time (especially behind the wheel of a car), as well as the characteristic “start-up syndrome”.
Painful impulses often radiate along the thigh, descending to the big toe (! - applied meaning. An indication of the involvement of the spinal roots that form the obturator nerve and are immediately covered by a group of lumbar muscles) .
The findings are also interesting when palpating the pelvic muscles, especially in the area of the ischial tuberosities, branches of the pubic bones, capsule of the hip joints and the obturator foramen itself with its muscles, and the nerves and vessels penetrating through it.
Using our (from Practical Myology) motto: “From diagnostic methods to treatment methods,” you can quite simply treat all of the listed muscles (synergists and antagonists) and obtain a result of such effectiveness that neither anesthesiologists, nor surgeons, nor endocrinologists have ever dreamed of, and neuropathologists who follow their lead. I’m not even talking about osteopaths, kinesiologists, and other “specialists” about whom I wrote a number of articles at one time. And only for one, and the most important (!) reason - they all do not treat muscles in the form that is in Practical Myology.
Georgy, in a personal letter to you, taking into account your remoteness (“on the other side of the globe”), I briefly outlined the essence of the techniques with which you can now be guaranteed to help your patients, and here, as promised, you will read about their theoretical justification .
OK
Additional treatment
Another direction of etiotropic therapy is the restoration of metabolic processes, normal motor activity, as well as the removal of inflammation and swelling.
For this, the fastest option is to administer glucocorticosteroids by injection directly into the tissues that surround the nerve. In this case, Diprospan is most often used - it is a two-component glucocorticosteroid containing betamethasone dipropionate. It gives a long-lasting anti-inflammatory effect. In extreme cases, novocaine nerve blocks are prescribed.
An alternative option is compresses with anesthetics, dimexide and glucocorticosteroids, which are applied to problem areas for 20-30 minutes. It is also possible to use non-steroidal anti-inflammatory drugs like Ibuprofen, but they are considered less effective.
To improve blood circulation, medications such as nicotinic acid or Pentoxifylline are prescribed. Antioxidants are prescribed - for example, thioctic acid.
In almost all cases, to improve the functioning of the nervous system, B vitamins are prescribed. Massage plays a major role in treatment (it can only be performed by a specialist) and a specially developed set of exercise therapy exercises. Physiotherapy methods are widely used. These are magnetic therapy, electrophoresis, electrical stimulation procedures.
Cost of osteopathy in Moscow
| Service name | Price according to the price list, rub. | Discounted price* until August 31, rub. |
| Initial appointment (examination, consultation) with an osteopathic doctor | 1 500 | 1 000*** |
| Manual therapy session (osteopathic correction), (30 minutes) | 4 000 | 3 600 |
| Manual therapy session (osteopathic correction, soft techniques), (60 minutes) | 6 000 | 4 400 |
* Discounts apply only to primary patients of the clinic. Discounts on individual procedures are available when paying for a course (from 9 procedures).
*** Promotion until 31.08 - when starting treatment (or purchasing herbal medicines) on the day of consultation - consultation is FREE
The administration of the clinic takes all measures to timely update the price list posted on the website, however, prices may differ from the actual ones. Please, in order to avoid possible misunderstandings, check the cost of services at the reception or in the contact center by phone +7 (Moscow) or (St. Petersburg), daily from 9 to 21 hours. The price list posted on the website is not a public offer. Medical services are provided on the basis of a contract. Bank cards VISA, MASTERCARD, MAESTRO, MIR are accepted for payment. Contactless payment by cards, Apple Pay and Google Pay is also available.
Symptomatic therapy
Once diagnosed with tunnel neuropathy, how to treat it is a critical question. And at the same time, the choice of a drug for symptomatic therapy that will help relieve pain plays a special role.
For this purpose, the following types of means are used:
- Anticonvulsants. Their action is based on the fact that they calm certain structures of the spinal cord and brain, which are responsible for the appearance of a pain reaction when a nerve is compressed.
- Anesthetics (it would be more correct to call them transdermal systems with an anesthetic, which is lidocaine). They act in the same way as anticonvulsants.
- Tricyclic antidepressants. They reuptake serotonin and dopamine, which helps relieve pain.
However, tricyclic antidepressants are prescribed only when the potential benefit significantly outweighs the possible side effects: drowsiness, increased blood pressure, impaired coordination of movements. Relatively safe are drugs such as Escitalopram, which are also classified as antidepressants, but in a different group.
If we are talking about the treatment of pathologies such as compression-ischemic tunnel neuropathies (the carpal nerve is damaged or any other), and it is known for sure that mechanical compression of the vascular and nerve trunks by spasmed muscles has occurred, then muscle relaxants are prescribed. They relax muscles and have an analgesic effect.
According to doctors, one of the most effective drugs in this group is Tizanidine; Baklosan and Tolperisone are also used.
ethnoscience
In the course of treatment, you can use the following folk remedies:
- Massage with fir oil has long been considered an excellent way to relax muscles and relieve swelling from the nerve. It is necessary to massage the damaged area with light and smooth movements. You need to repeat the procedure 3 times every day;
- Rose infusion, according to experts, helps to calm down and relieve inflammation. To prepare, you need to take flower petals and pour 250 ml of boiling water over them. You should drink 3 such glasses a day and the course of treatment is 20 days;
- A mixture of tinctures of peony, motherwort, calendula and hawthorn is used in 1 tsp. before bed for 21 days. According to experts, these sedatives will make the spasm subside much faster.
The course of therapy should begin immediately after symptoms are detected. In this case, you can avoid unwanted consequences, for example, contracture or involuntary movements of the facial muscles. The body usually recovers from 30 days to a year, depending on the severity of the damage and the reason for which it occurred.
Facial nerve neuropathy is a rather unpleasant problem and doctors recommend taking preventive measures to prevent it. To do this, you should not overcool and avoid injuries, as well as fully treat all pathologies in the body, especially those of an inflammatory and infectious nature.
Physiotherapy for the treatment of facial neuropathy
Various physical treatments for Bell's palsy such as exercise, laser, electrotherapy, massage and heat therapy have been successfully used to speed up recovery. However, data on the effectiveness of any of these treatments is lacking. A systematic analysis of the effectiveness of physical therapy, electrical stimulation, and exercise on the outcome of Bell's palsy leads to the conclusion that there was no significant benefit or harm from any of these physical treatments for Bell's palsy. There was limited evidence that improvement began earlier with specific exercises.
Antiviral drugs
The rationale for the use of antivirals is that inflammation of the facial nerve in Bell's palsy may be associated with herpes simplex virus (HSV). In a post-mortem study, latent herpesvirus type 1 was isolated from the majority of geniculate ganglion samples. The genome was found in 79% of cases in the facial nerve in the endoneurial fluid of patients with Bell's palsy, but not in controls. However, the benefit of acyclovir or valacyclovir, either as single drugs or in combination with prednisolone, in Bell's palsy has not been conclusively proven. Thus, given the available evidence, the use of acyclovir or valacyclovir should not be routine, and treatment with acyclovir is highly unlikely to be cost-effective.
Procedures and operations
In addition to drug therapy, neuropathy of the peroneal nerve also includes physiotherapeutic procedures:
- Magnetotherapy. It is based on the effect of a magnetic field on the human body, which helps relieve pain, restore nerve cells, and reduce the severity of the inflammatory reaction.
- Amplipulse. It is based on the effect of modulated current on the affected area, due to which nerve cells are restored and swelling is reduced. Has an anti-inflammatory effect.
- Electrophoresis with drugs. It is based on the influence of an electric field, due to which medications enter the site of inflammation.
- Ultrasound therapy. When exposed to ultrasound, blood circulation is stimulated and the severity of pain is reduced. Has a tonic and anti-inflammatory effect.
- Electrical stimulation. Restoration of neuromuscular conduction occurs under the influence of electric current.
Radial nerve neuropathy is treated in the same way. A course massage is also recommended to restore the radial nerve.