Main symptoms:
- Throwing a swallowed lump into the nasal cavity
- Throwing a swallowed lump into the oral cavity
- Difficulty passing food through the esophagus
- Cough
- Lump in the throat
- Inability to swallow food
- Feeling of fullness in the back of the sternum
- Increased salivation
- Suffocation
Dysphagia is a swallowing disorder that occurs with certain diseases of the pharynx, esophagus, or central nervous system. In most clinical situations, this sign is observed in the presence of pathologies of the esophagus (esophageal dysphagia). The esophagus is a kind of muscular tube, the main function of which is to move incoming food from the back of the oropharynx directly into the stomach cavity.
- Causes
- Classification
- Degrees
- Symptoms
- Diagnostics
- Treatment
Risk group:
- premature babies;
- patients who have a history of diseases of the brain or central nervous system;
- elderly people.
Physiology of swallowing
Swallowing while eating is carried out by a person reflexively. This means that we do not think or specifically strain any part of the body to ensure the function of passing food from the mouth to the stomach. Although we can force ourselves by a strong-willed decision to swallow, for example, saliva, a bitter medicine.
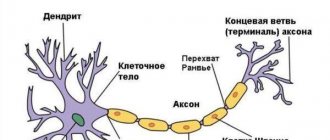
In the act of swallowing, physiologists distinguish 3 successive phases:
- oral - initial, controlled, initiated by the centers of the brain, activating the swallowing apparatus with their impulses, while the contents of the mouth extend beyond the palatine arches;
- pharyngeal - ensured by involuntary movements, responsible for the entry of the food bolus into the upper part of the esophageal tube and reflex movement downwards;
- esophageal - occurs inside the esophagus due to peristaltic movements of the muscles, guarantees the transport of contents through the cardiac sphincter into the stomach.
The study of changes during swallowing showed that esophageal dysphagia as a pathological condition is a disorder of either a functional or organic nature at any stage of the process. The disease can be treated correctly only by understanding the type of lesion.
How to distinguish a spasm in the throat during VSD
The central nervous system controls the functioning of every organ and system of the human body.
The soreness and discomfort in the oropharynx, which are familiar to many, are not always signs of respiratory diseases; their occurrence may well be of a somatic nature. Most often, people with dystonia cannot give an exact date for the onset of problems with swallowing. However, their brain intensively draws pictures, one more terrible than the other, in which they imagine the presence of all sorts of ailments. For this purpose, they study specialized literature that confirms the presence of diseases and causes panic attacks in dystonics, provoking the emergence of new problems that do not allow them to take a sip.
Even before the examination begins, a person may assume that he has cancerous tumors or pathologies of the thyroid gland. You can distinguish a nervous spasm of the pharynx from other diseases based on the following signs:
- absence of problems and discomfort in the throat at night, during sleep or in the morning, immediately after waking up (due to the rest of the brain, which does not send signals for a spasm to occur);
- the appearance of a lump in the throat after vigorous activity has begun and the body has finally awakened;
- passion for some interesting activity or complete immersion in work contribute to the disappearance of unpleasant symptoms, or rather to the switching of the brain to other tasks, which leaves it no time for neurosis-like manifestations.
Important! Throat spasms that prevent you from eating properly are not a symptom of pathological processes of the thyroid gland or cancer. Having problems with the endocrine system can aggravate dystonia, which in turn can cause such a problem.
Causes
Temporary (functional) dysphagia causes excessive stimulation of some cortical centers of the brain. False signals contribute to short-term spastic contractions of the circular muscles of the esophagus. The condition is provoked by mental illness, stress, and strong emotions.
In such cases, people say that the symptoms develop “from nervousness.” In this case, there are no mechanical obstacles to the movement of food.
A similar symptom may occur in a child with a reluctance to eat something, fear, or hysterical behavior.
Nervous dysphagia accompanies other manifestations of neurosis: irritability, tearfulness, insomnia. In such cases, treatment by a neuropsychiatrist is indicated. The use of soothing methods helps to avoid swallowing disorders. Organic causes include diseases of the esophagus and stomach, mouth and pharynx, thyroid gland, heart, and brain.
The most significant lesions of the esophagus include:
Pain in the esophagus after eating
- inflammation (esophagitis);
- narrowing due to scars after a burn (alkali or acid), developmental anomalies, cardiospasm, replacement with connective tissue in scleroderma;
- gastroesophageal reflux disease - the acidic contents of the stomach are thrown back into the lower part of the esophagus, causing inflammation and irritation;
- wall diverticula - saccular protrusions due to the weakening of individual sections of the muscular membrane; they can be congenital or formed as a result of prolonged untreated inflammation;
- tumors of the esophagus, stomach, benign and malignant;
- achalasia cardia - damage to the cardiac sphincter, causing a delay in the passage of food from the esophagus to the stomach;
- injury from a swallowed sharp foreign object (fish bone, small toy, button) or injury to the chest.
The esophagus can be compressed from the outside by enlarged neighboring organs: dilated veins with portal hypertension (liver cirrhosis), aortic aneurysm, hypertrophied heart, tumor coming from the mediastinum, growth of the thyroid gland, strangulation of the hernial opening in the diaphragm.
The most common causes of dysphagia among diseases of the oropharynx are:
- severe tonsillitis with significant enlargement of the tonsils;
- tumors;
- stuck foreign bodies;
- severe swelling as a manifestation of an acute allergic reaction;
- incorrect positioning of teeth, ulcerative stomatitis.
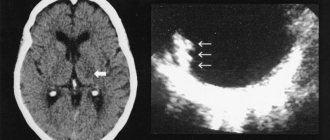
Functional dysphagia must be distinguished from neurogenic dysphagia caused by diseases of the brain (tumors, stroke) and cervical spine. A space-occupying process in brain tissue (including a hematoma) located close to the medulla oblongata, where the swallowing center is located, exerts direct pressure or irritation on neurons and their connections. In addition, impaired blood circulation in certain areas of the brain during an ischemic stroke can lead to paralysis of the pharyngeal muscles.
The nuclei of the medulla oblongata form the respiratory, vasomotor centers, control coughing, vomiting, swallowing and many other body actions
Dysphagia, as a syndrome, is present in patients with Parkinson's disease, multiple sclerosis, cerebral palsy, and myasthenia gravis. Infectious disease doctors observe dysphagia in encephalitis and botulism.
Classification
Depending on the duration of the signs of dysphagia, acute and chronic stages of the disease are distinguished. In addition to functional and organic dysphagia, forms of the disease are distinguished depending on the level of damage to the act of swallowing.
Oropharyngeal or oropharyngeal - the entry of a bolus of food into the upper part of the esophagus is disrupted due to problems in the muscular apparatus of the pharynx, innervation, in neighboring tissues (occurs in 80–85% of patients). In young people, it is more often associated with diseases of an inflammatory nature, the development of connective tissue membranes, and ring-shaped formations. In old age, the cause is cerebrovascular disorders (stroke, parkinsonism, senile dementia).
Esophageal - caused by obstructed passage of food through the esophageal tube, divided into middle and lower. Some authors also identify a pharyngoesophageal form, in which changes concern the involuntary phase of rapid swallowing.
Depending on the course, dysphagia can be:
- constant;
- intermittent (appears from time to time);
- progressive – there is a gradual deterioration in the patient’s condition.
Causes of VSD
People with vegetative-vascular dystonia have the ability to create entire chains in their own thinking, which, in their opinion, are not devoid of logic, which quickly take on real shape. In them, they draw a parallel between the presence of unpleasant manifestations of a lump in the throat with the possible and imminent death of themselves, which causes them serious panic attacks.
Negative events that occurred many years ago and associated with the inability to swallow can become the root cause of the development of panic attacks at the slightest repetition of the situation or the appearance of its characteristic features. The main feature of the work of a person’s consciousness is the consolidation of negative aspects that are accompanied by a constant fear of recurrence of panic attacks, therefore the main cause of anxiety and fear lies in the state of a person’s mental, rather than physical, health.
Factors that provoke problems with swallowing are:
- a nervous spasm of the larynx that occurred earlier while eating, which left an unpleasant impression;
- a vivid attack of panic, during which the person clearly imagined the possibility of suffocation;
- a nervous lump in the throat, which focused on itself all the person’s experiences (most often found in days of severe depression or anxiety), causing him to worry about the inability to eat;
- an unsuccessful meal, during which the rider choked on food and almost suffocated, etched in his memory for a long time (the situation can arise due to talking while eating, laughter, or improper chewing of food).
How it manifests itself
Depending on the cause, impaired swallowing by category can be considered as a separate pathology (primary) or dysphagia syndrome in a specific disease (secondary). Disrupted act of swallowing food causes:
- pain behind the sternum and in the epigastric area;
- belching of food and air;
- heartburn due to regurgitation (return of contents from the stomach), especially when bending forward, at night, if dinner occurs late;
- hoarseness (dysphonia);
- increased salivation;
- feeling of lack of air.
Patients usually complain of difficulty swallowing tough, solid foods, improvement when drinking or switching to liquid meals. Due to disrupted connections and the sequence of physiological processes of swallowing, the contents of the mouth do not enter the esophagus, but into the respiratory tract (nose, larynx, trachea). In response, a spastic contraction, paroxysmal cough, and suffocation develop.
With the oropharyngeal form of the disease, patients always point to the area of the neck and throat that causes difficulty
The oropharyngeal form is characterized by cough, regurgitation of food through the nose, nasal speech, the occurrence of asthma attacks, and other neurological disorders (double vision, impaired speech, drooping eyelids). It is important to consult a neurologist to identify pathology of the cranial nerves that regulate swallowing. Neurologists distinguish between dysphagia in bulbar (the central nuclei are affected) and pseudobulbar disorders (changes are localized in the impulse transmission pathways).
For the esophageal form, more typical complaints are difficulty in passing food, a feeling of a bolus being “stuck”, association with drinking food, regurgitation, pain in the area of the esophagus during swallowing, and weight loss. With functional dysphagia in patients with neuroses, complaints are always described vividly and in detail.
Difficulties in swallowing are associated with the type of food, the time of eating, previous insomnia, and anxiety. After rest, the symptoms disappear.
How is the severity of pathology determined?
The disease is distinguished into certain degrees of dysphagia based on a detailed description of patient complaints:
- I - a person experiences difficulties only when eating dry food or solid foods;
- II - it is impossible to swallow dry and solid food, but semi-liquid and liquid food passes freely;
- III - you can only swallow liquids;
- IV - absolutely impossible to swallow anything.
Depending on the degree, dysphagia treatment tactics are developed.
Why does it occur in children?
A feature of dysphagia in childhood is its connection with a disorder of underdeveloped nervous regulation of swallowing. The disease can be congenital or acquired. Often accompanies cerebral palsy and developmental anomalies.
Constant spitting up should cause concern for parents
Parents can suspect the first signs in infants by slow eating, refusal of nipples with a large hole, choking and coughing when eating quickly, better condition with slow feeding, adjustment of the baby's head before sucking, milk flowing into the nose. Less commonly, the pathology is detected against the background of frequent bronchitis and pneumonia, bronchial asthma.
Prevention of dysphagia
- Timely and sufficient treatment of diseases leading to impaired swallowing (tumors, inflammation, burns, etc.).
- A rational and balanced diet (eating foods high in fiber (vegetables, fruits, greens), avoiding too hot, fried and canned foods).
- Quitting smoking and excessive alcohol consumption.
- Careful care of children (it is necessary to ensure that they do not swallow small parts of toys, tablets, etc.).
Diagnostics
Diagnosis of both forms of dysphagia requires a thorough interview of patients in order to clarify symptoms, identify connections and causes, and establish the level of damage to the act of swallowing. General blood, stool, and urine tests help identify the primary disease that contributes to dysphagia. Therefore, they should be carried out for differential diagnosis.
The results of liver tests and ECG must be studied. To identify the oropharyngeal form, the main criteria are obtained using:
- Screening test - the patient is given to drink 150 ml of water as quickly as possible, at which time the doctor counts the number of sips and time. The data obtained allows us to calculate the rate of swallowing and the volume of the sip (average). Diagnostic accuracy, with a decrease in both indicators, ensures correct diagnosis in 95% of cases.
- Fluoroscopy studies of the upper esophageal sphincter during barium swallow.
- Laryngoscopy is a technique for examining the posterior wall of the larynx.
Esophageal dysphagia is particularly difficult to identify due to the need to exclude many diseases that contribute to the formation of a mechanical obstruction. First of all, the doctor must make sure that there is no malignant process.
The tumor is favored by the duration of dysphagia for more than four months, the progressive course, severe symptoms when eating solid food rather than liquid, and the patient’s weight loss. X-ray examination with contrast reveals disrupted contours of the esophagus, signs of an ulcer or neoplasm, diverticulum, achalasia and other organic pathology.
Endoscopic detection of tumors and disruption of the internal structure of the esophagus
Esophagogastroduodenoscopy - allows you to visually examine the inner surface of the esophagus, stomach and duodenum, and take questionable tissue for examination for biopsy. The motor function of the esophagus is checked with a four- or eight-channel device (water-perfusion catheter), which, like a manometer, measures the tone of the upper and lower esophageal sphincters and the thoracic region.
The technique used in specialized centers is considered more accurate. These are high resolution manometry and 3D volumetric manometry. It is possible to obtain not only indicators, but also a color image of peristalsis waves. The method of radionuclide scintigraphy of the esophagus is based on measurements of radioactivity after the patient swallows water mixed with Technetium 99.
If contractility is impaired, the release of the radioactive substance into the stomach slows down.
To conduct a differential diagnosis, you may need an ultrasound examination of the abdominal organs; magnetic resonance imaging of brain structures, electroencephalography of the brain, consultations with a gastroenterologist, neurologist, or otolaryngologist.
Treatment
In the treatment of oropharyngeal dysphagia with neurological and neuromuscular disorders, there is positive experience with the use of drugs only for myasthenia gravis and Parkinson's disease. In other cases, all therapy is aimed at preventing food from entering the respiratory tract and further complications.
For this, patients are recommended:
- switch to liquid and soft foods;
- adapt to nutrition by choosing a posture.
Swallowing reflexes are activated by adding citric acid to food. Exercises are prescribed to retrain the swallowing act. To suppress the cough reflex, drugs from the group of angiotensin-converting factor inhibitors are recommended. If there is a high risk of aspiration or the impossibility of feeding through the mouth, food is administered by tube.
Stroke patients with oropharyngeal dysphagia have to have a gastrostomy tube (an artificial opening for infusing liquid food directly into the stomach) removed. With the help of surgery, spastic contraction of the laryngeal muscles is eliminated.
Treatment of esophageal dysphagia requires a gentle diet (switching to frequent intake of warm liquid food, in small sips, avoidance of alcohol, fried foods, spices, hot seasonings), prevention of gastroesophageal reflux with the help of drugs that reduce acidity, and anti-inflammatory measures. In case of cicatricial and adhesive processes, the esophagus is bougienage with rubber tubes.
Mechanical obstacles can only be removed surgically. The scope of intervention is determined individually in a particular case.
Treatment of the disease
Therapy for dysphagia syndrome should be based on a differentiated approach, because has both functional and organic causes. With functional dysphagia, the patient should be explained the cause of the pathology, the conditions for a favorable prognosis, and given recommendations on preventing trigger factors, proper nutrition (chew food thoroughly) and changing any psychological situations that can provoke dysphagia syndrome.
In patients with dysphagia caused by nervousness, the use of antidepressant drugs and psychotherapeutic methods is recommended. There is the possibility of applying an empirical extension. For spastic disorders that cause the development of dysphagia, it is recommended to use muscle relaxants, botulinum toxin injections, and dilation of the esophagus using the pneumatic method.
The first step in the treatment of dysphagia of organic etiology is to influence impaired motor skills and eliminate causative factors.
Correction of motility is carried out with the help of medications that have a stimulating or inhibitory effect on the muscular apparatus of the esophagus.
- Treatment with drugs that have an stimulating effect (prokinetics): selective - domperidone and non-selective drug - metoclopramide. Metoclopramide enhances the muscle tone of the lower esophageal sphincter, its peristalsis, and causes the fastest passage of food from the stomach and throughout the intestines. The average dosage of metoclopramide is 10 mg. three times a day, the drug is taken half an hour before meals. Sometimes a fourth dose of metoclopramide can be added. If the drug is prescribed parenterally, the dose will be 10 mg. 1-2 times a day. Another drug that has a selective mechanism of action is domperidone. The effects of the drug are the same, except for the effect on the large and small intestines. There are far fewer side effects than metoclopramide. Dosage 10 mg. three times a day, take 30 minutes before meals or before bed.
- If a patient's dysphagia is accompanied by hypermotility of the digestive system, it is advisable to begin treatment with antispastic medications. These include non-selective anticholinergics, calcium channel blockers, nitrates and myotropic antispasmodics. The best effect is achieved by the selective anticholinergic blocker of M1 receptors - gastrocepin. Take 50 mg. twice a day. Of the calcium channel blockers, dicetel is most often used at a dose of 50-100 mg three times a day. Of the nitrates, preference is given to prolonged ones - isosorbide mononitrate (0.01-0.02 g twice a day), isosorbide dinitrate (0.005-0.01 three or four times a day). Of the myotropic antispasmodics, noshpa (0.04 g), nikoshpan tablet, and duspatalin 0.2 g twice a day are quite effective.
- Treatment of each type of dysphagia has certain subtleties, for example, the main treatment for esophageal achalasia is the balloon pneumocardiodilation method. Less commonly used is a technique based on botulinum toxin - it is injected into the thickness of the lower sphincter of the esophagus. If conservative treatment turns out to be ineffective, they resort to surgical methods, most often myotomy operations.
Treatment of dysphagia in most cases is impossible without prescribing a diet. This is required by the following diseases: gastroesophageal reflux disease, Barrett's esophagus, esophagitis. Hiatal hernias that are asymptomatic do not require treatment; if there are signs of strangulation, hernia treatment is surgical. If a patient is found to have Helicobacter pylori contamination of the mucosa, treatment should begin with eliminating the infection. In case of a complicated course of the underlying disease (recurrent gastroesophageal bleeding, the presence of strictures), as well as insufficient effect of conservative treatment methods, surgical intervention (resection) or endoscopic methods of therapy (methods of laser and photodynamic coagulation of metaplastic areas of the mucosa) are indicated.