What is a neural tube?
The neural tube is the basis of the future nervous system that forms in the fetus, which develops from the outer cellular layer (germ layer - ectoderm) along with the skin, while the digestive system is formed from the endoderm.
The laying of the fetal neural tube begins in the third week of its development. First, the neural plate appears, then small elevations called neural folds form at its edges, in the center of which a groove appears. It will later serve as a cavity for the organ. Around day 24, the plate begins to curl and the rollers close, forming a tube shape.
In front it expands, forming the brain vesicles, and the rest will become the spinal cord. Particles of the ganglion plate are gradually separated from the ridges, from which the nodes of the spinal cord and branches of the autonomic part of the nervous system are then formed. You can see the appearance of spinal ganglia in the embryo after 1.5-2 months.
The cells formed in the ganglion plate gradually move to the ganglia in the sympathetic trunk, the adrenal medulla and the walls of the future intestine.
The final formation of the tube occurs at 5-8 weeks, when the development of all fetal organs begins. At this moment, the baby’s heart, lungs, sensory organs, limbs and other systems are formed. The tube itself also becomes more complicated.
Structure and layers
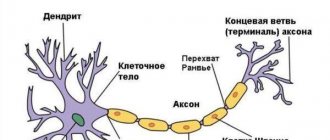
During the development of the nervous system, three layers appear in the tube:
- ependymal or internal;
- mantle or intermediate;
- marginal veil or outer layer.
The first layer serves as the basis for neurons and gliocytes of the nervous system. Some neurons move into the peripheral part of the organ, forming the mantle layer, and the rest form glial cells.
The most important of these, ependymocytes, line the inside of the tube, which will then develop into the central spinal canal and the walls of the ventricles of the brain.
In the inner layer, separate functional zones are distinguished, which over time transform into one another. The division zone contains cells, among which those closer to the center extend processes to the outer edge and move the body of the neuron containing the nucleus there.
At this time, DNA synthesis occurs in it, after which the particles return to their place. The cells “sitting” on the lower edge are divided into two.
At the migration site, these halves interact. One of them begins to divide again, and the other, using it, moves to the intermediate layer.
The intermediate layer appears thanks to neuroblasts - migrant cells that have not lost the ability to divide and are attached to the inner part of the layer.
Neuroblasts gradually form axons, which are sent to the outer layer, thus forming a dendritic tree and turning into neurons. Unattached cells transform into spongioblasts. From the intermediate layer, such a part of the spinal tissue as gray matter is formed.
The layer on the outside consists of the processes of neurons contained in the mantle layer and blood vessels. It acts as the basis for the development of white matter in the brain.
Treatment
Immediately after the birth of a child, doctors eliminate life-threatening conditions - lack of spontaneous breathing, abnormal temperature readings. Specialists determine blood type and Rh, the presence of severe disorders in the functioning of internal organs.
Wounds in the hernia area are treated with antiseptics and a sterile bandage is applied. The newborn should lie on his stomach with his head slightly lowered.
Elimination of defects is carried out mainly by surgical methods. After surgery, antibacterial drugs are prescribed to prevent the development of inflammatory processes in the lungs, kidneys, bladder, and brain. Wounds are constantly treated, bandaged, and therapy is carried out aimed at reducing cerebrospinal fluid pressure.
Restoration of impaired functions begins after the wound has healed, sutures have been removed, and inflammatory processes have stopped.
Formation of the spinal cord
The process of formation of the rudiments of nervous tissue is called neurulation. The basis of the spinal cord is made up of a large half of the tube, which was not involved in the formation of the brain. The constant separation of cells located at opposite ends leads to the formation of a shape resembling an hourglass, consisting of a pterygoid (this is the upper thickening) and a basal plate (or the lower thickening).
From the first, the posterior branches of the spinal cord are gradually formed, and from the second, the anterior ones. The process of differentiation begins. It occurs due to the movement of neuroblasts outside the marginal veil.
In the spinal cord, unlike parts of the brain, cells do not “go” beyond the marginal zone, which ensures the preservation of the separation of layers in a person in the future: into the central canal, gray and white matter.
The formation of the neural tube in human ontogenesis occurs due to the “switching on” of certain groups of genes. Thus, for the formation of the pterygoid plate, the Pax gene must be activated, but for the basal plate it is suppressed.
Diagnostics
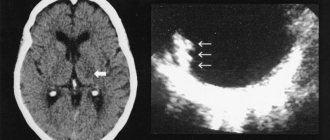
The main diagnostic method is genetic screening; abnormalities in the structure can only be seen on ultrasound. If a pathology is identified, it is necessary to undergo examination by several specialists to exclude an error in diagnosis.
Signs of pathology during ultrasound examination:
- thickening of the vertebrae in the lumbosacral region;
- deformation of the lower extremities;
- hydrocephalus;
- Arnold-Kari syndrome.
Other research methods are amniocentesis, 3D ultrasound. If a developmental pathology is suspected, a woman is prescribed a biochemical blood test for the content of alpha-fetoprotein and acetylcholinesterase.
Confirmation of developmental defects is usually grounds for termination of pregnancy. But, since even the most modern methods of prenatal diagnosis reveal only the presence of pathology, but do not determine the severity, the decision to keep the child is made by the parents.
Causes and consequences of abnormal development of the neural tube in the fetus
The formation of a fetal tube is a complex and multifaceted process; failure in at least one element leads to severe defects in the development of the organ. They affect the child’s brain and his spine, because the connection between the neural tube and notochord is very tight.
Defects are formed in situations where the formation of the neural tube does not occur completely or does not close. This may cause:
- Spina bifida. It is formed at the base of the column, where a hole is formed through which the spinal cord will exit.
- Anencephaly is formed in the upper part of the neural tube and leads to the immaturity of some elements of the brain and the development of the fetal skull.
- Chiari malformation is characterized by “leakage” of brain tissue into the spinal canal.
- Encephalocele manifests itself as partial protrusion of the brain and membranes through the cranial bones.
The reasons for the formation of such defects have not yet been precisely established. At some point, ontogenesis fails, which subsequently leads to disruption of the entire system. Since the tube is laid in the late gastrula and this stage is completed on the 25th day, its mechanism has not been well studied.
It is known that the likelihood of defects is influenced by hereditary factors and diseases affecting the nervous system.
It influences the formation of the problem and environmental conditions, as well as the condition of the mother. Negative aspects that increase the risk of neural tube defects include:
- radiation exposure;
- arsenic or lead poisoning;
- prolonged fever in a woman in the initial stages of pregnancy;
- lack of nutrition;
- viral infections;
- vitamin A hypervitaminosis;
- excess weight or diabetes in the mother;
- lack of folic acid in a pregnant woman;
- a woman taking certain medications.
The condition of the mother is the first factor that affects the formation of a tube in the fetus. If a woman is in an environmentally unfavorable area, where harmful substances (pesticides, exhaust gases, petroleum products, etc.) can enter the air and water, she inhales them, and together with the blood, these products enter the baby’s body.
For an adult, the risk is lower, since his body is already formed and is able to process most hazardous substances. In the body of the embryo, the defense mechanisms do not yet work and any harmful effect can disrupt the course of processes and lead to the development of pathology, including changes in the condition of the tube.
Poor nutrition also has a negative effect. A lack of nutrients leads to disruption of the processes of organ formation, as well as an excess of biologically active components such as vitamins.
Diagnostics
Detection of such defects is carried out in the prenatal period. Biochemical techniques and various methods of intrascopy of the fetus are used. All pregnant women are divided into several risk groups for developing neural tube defects in the fetus. What does this mean? Diagnostic measures in each group differ.
- For women at low risk, examinations by obstetricians and gynecologists are carried out once a month. After the 15th week of pregnancy, the content of fetoprotein in the woman’s blood and amniotic fluid is examined. If its level is significantly reduced, a repeat examination and ultrasound of the fetus is performed. In the third trimester, another ultrasound is performed.
- In high-risk groups, examination by an obstetrician-gynecologist is also required - already several times a month. After week 15, fetoprotein levels are repeatedly examined. Sonographic examination of the fetus is also carried out regularly. If there are difficulties in diagnosis, tomographic methods are indicated.
Symptoms of defects
If there are neural tube defects, the baby may die before birth, or in the first hours after birth. A similar thing is observed with encephalocele.
If the baby is born viable, he may experience the following symptoms:
- physiological deformation (appearance of spinal tissue in the lumbar region);
- dysfunction of the pelvic organs;
- paralysis and convulsions;
- pain when moving;
- decreased sensitivity of organs;
- developmental disorder.
Problems can also be detected during intrauterine development. This can be done by a doctor during ultrasound diagnostics, which occurs at the stage of 20-22 weeks.
Symptoms of the consequences of developmental anomalies:
- Hidden spinal nonunion located in the lumbar and sacral areas. It has no clinical symptoms and is usually discovered accidentally during an X-ray examination. In this case, no changes appear on the skin, with the exception of rare pigment spots or wen. The consequences of such a defect are poor posture, weakness of the leg muscles, foot deformities, lower back pain, and urinary incontinence.
- Open clefting manifests itself in the form of a cyst - the dura mater, which contains cerebrospinal fluid. Its consequences depend on the number of affected vertebrae. If 3-5 pieces are affected, then the patient exhibits urinary system disorders and muscle weakness. If 6-8 vertebrae are affected, the protrusion becomes visible, and the patient may experience rupture of the cyst sac and leakage of fluid.
- Failure of fusion of the spine and surrounding soft tissues leads to incomplete development of the spinal cord and is often incompatible with life.
Most often, such deviations affect the lumbar region, and extremely rarely the thoracic or cervical region. This is related to the likelihood of fetal survival. Damage to the cervical spine is often incompatible with life and therefore ends in miscarriage.
Causes
Neural tube defects are structural anomalies caused by delayed or incomplete closure. Formed in the embryonic period.
Why does pathology develop:
- hereditary factor;
- Patau, Turner, Edwards syndrome;
- radioactive radiation, poisoning with arsenic, lead, pesticides;
- taking anti-epileptic drugs shortly before or immediately after conception;
- unbalanced diet, vitamin A hypervitaminosis;
- increased spinal pressure in the fetus;
- viral diseases in pregnant women, rubella is especially dangerous;
- significant and prolonged increase in temperature in the early stages;
- obesity caused by diabetes.
But the main cause is considered to be folic acid deficiency during pregnancy.